Author: Dominik Zbogar, Kelsey Zhao | Reviewer: Peter New | Published: 17 September 2024 | Updated: ~
Key Points
- NTSCI can be broken down into three major categories: congenital, genetic, and acquired which accounts for the large majority of cases.
- Rates of NTSCI vary widely worldwide and much information is lacking. Developed countries tend to have a higher proportion of cases caused by degenerative conditions and tumours. Developing countries tend to have a higher proportion of NTSCI acquired from infection.
- Those with NTSCI are more likely to be older, female, have paraplegia and have an incomplete injury when compared to those with traumatic SCI.
- Much of NTSCI rehabilitation is similar to traumatic SCI rehabilitation, though the rehabilitation stay is shorter.
Spinal cord injuries (SCI) can have traumatic or non-traumatic causes. Traumatic SCIs are caused by external forces in events such as car accidents and falls. Non-traumatic spinal cord injuries (NTSCI) occur without an external physical force and are typically caused by an underlying health condition.
Causes of NTSCI can be divided into three major categories: congenital, genetic, and most commonly – acquired.
Congenital (present at birth)
 Congenital NTSCIs are developmental defects, malformations, and abnormalities affecting the spinal cord which are present at birth. An infant can have one congenital condition, or multiple conditions at the same time. For example, Type 2 Chiari malformations almost always occurs in association with myelomeningocele, a severe form of spina bifida
Congenital NTSCIs are developmental defects, malformations, and abnormalities affecting the spinal cord which are present at birth. An infant can have one congenital condition, or multiple conditions at the same time. For example, Type 2 Chiari malformations almost always occurs in association with myelomeningocele, a severe form of spina bifida
Spinal dysraphism
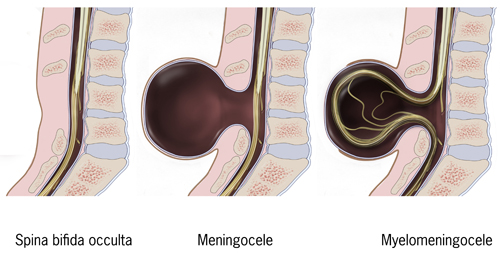
Myelomeningocele is the most severe type of spina bifida as the spinal cord itself protrudes through the opening of the unfused portion of the spinal column.2
Spinal dysraphism is a defect in the development of the neural tube (an early form of the brain and spine) where the canal that houses the spinal cord does not completely close and causes damage to the spinal cord and nerves. A well know type of spinal dysraphism is spina bifida.
Chiari malformations
Chiari malformations are a condition where a part of the brain known as the cerebellum is pushed into the space where the brain connects to the spinal cord.
Skeletal malformations
Skeletal malformations include any deformities or abnormalities in the development of bones or ligaments that affects the spine. These malformations can put the person at higher risk of spine instability which can cause pressure on the spinal cord that can result in NTSCI.
Congenital syringomyelia
Congenital syringomyelia is the formation of a fluid-filled sac, known as a cyst or syrinx, in the spinal cord. This often occurs in association with spina bifida or Chiari malformations, but can also happen on its own, spontaneously.
Genetic
![]() A genetic NTSCI comes from an abnormality in a person’s genes that affects the spinal cord. This abnormaility can be inherited from one’s parents or be a spontaneous mutation that occurred during development. The effects of this genetic abnormality can be present at birth or show up later in life. Most genetic NTSCIs lead to loss of movement and/or sensation from the degeneration of nerve cells.
A genetic NTSCI comes from an abnormality in a person’s genes that affects the spinal cord. This abnormaility can be inherited from one’s parents or be a spontaneous mutation that occurred during development. The effects of this genetic abnormality can be present at birth or show up later in life. Most genetic NTSCIs lead to loss of movement and/or sensation from the degeneration of nerve cells.
Some examples of genetic NTSCI types include hereditary spastic paraplegia, spinocerebellar ataxias (e.g. Freidrich’s ataxia), adrenomyeloneuropathies, leukodystrophies, and spinal muscular atrophy.
Acquired
![]() Acquired conditions include the most common causes of NTSCI, such as degenerative spinal cord conditions, tumours, and vascular problems. This is a diverse category and the conditions become more common in older age.
Acquired conditions include the most common causes of NTSCI, such as degenerative spinal cord conditions, tumours, and vascular problems. This is a diverse category and the conditions become more common in older age.
Degenerative
Degenerative NTSCIs include any condition that causes damage to the spinal cord through the degeneration of its bone or ligaments. For example, spondylosis is a condition where there is an abnormal and painful degeneration in the bones and cartilage of the neck that can lead to loss of control or sensation over parts of the body.
Metabolic
Metabolism is the processes in the body that turns food into energy and the components that make up and maintain the body. Nutrient deficiencies like vitamin B12 and folate deficiency, or diseases that affect the maintenance of bone like osteoporosis and Piaget’s disease, can cause degeneration or damage to the spinal cord.
Vascular
Vascular causes of NTSCI refer to spinal cord damage caused by problems with the vessels that carry blood through the body. For example, if a blood vessel bursts and bleeds, if there are issues with abnormal connections between vessels, or if the blood supply is blocked, the spinal cord could be damaged. These issues can happen anywhere in the body and can cause NTSCI when they happen in the spinal cord.
Inflammatory or auto-immune
Inflammatory and auto-immune conditions involve immune system activity that damages the spinal cord through swelling (inflammation) or direct attack on healthy cells (auto-immune). The immune system is normally responsible for protecting us from viruses, bacteria, and other orgamisms but different conditions can cause overactive or innapropriate immune reactions. Examples include transverse myelitis and multiple sclerosis.
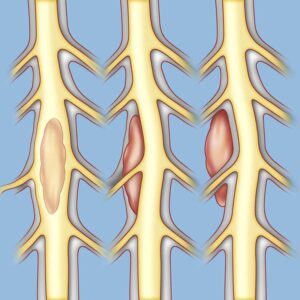
Spinal tumors may be (left to right) intramedullary, intradural-extramedullary, or extradural.5
Tumors and masses
Benign or malignant tumours can cause a NTSCI if the growth of the mass puts pressure on the spinal cord or interferes with the blood supply.
Infection
The spinal cord can be infected by bacteria, viruses or other organisms. Infections can put pressure on the spinal cord due to an abcess (pocket of infection) or interfere with the blood supply.
Other
Other uncommon causes of NTSCI include damage to the spinal cord due to radiation exposure and exposure to toxic substances. Amyotrophic lateral sclerosis and primary lateral sclerosis are both rare degenerative diseases that affect the motor neurons which are the nerve cells involved in the control and coordination of movement.
Are Multiple Sclerosis and ALS types of NTSCI?Multiple sclerosis (MS) is an auto-immune disease where the immune system attacks the protective covering (myelin) of nerve fibers in the central nervous system, which is made up of the brain and spinal cord. Amyotrophic lateral sclerosis (ALS) is a progressive nervous system disease that affects nerve cells in the brain and spinal cord. Because lesions can occur not only in the spinal cord but in the brain too, categorizing them is a challenge. Some studies include MS and ALS with their SCI sample while others choose to exclude these conditions. |

TSCI = traumatic spinal cord injury; NTSCI = non-traumatic spinal cord injury
Although NTSCI still affects males more overall, the proportion of females with NTSCI is higher relative to traumatic SCI. NTSCI is also more likely to affect older people.
The numbers by cause
The incidence of NTSCIs varies depending on the cause and the health services in the country where you live. Although there are many gaps in the research data, existing studies provide an idea how different NTSCI causes are distributed.
Congenital & Genetic
- In the few studies that recorded cases of congenital causes of NTSCI, spina bifida and other congenital conditions cause between 1 to 6% of cases. Overall, congenital and genetic NTSCI make up a very small proportion of NTSCI.
Acquired
- Malignant and benign tumours are common causes of NTSCI globally. Studies from all over the world since 1975 report that tumours are the cause of 14-44% of NTSCI cases
- Degenerative conditions of the spine are a very common cause of NTSCI in high-income developed countries. The percentage of NTSCI cases caused by degenerative conditions ranges from 13 to 62%. Many of these conditions become more prevalent with age.
- In the regions of Sub-Saharan Africa and South Asia, tuberculosis has been reported to cause 15 to 30 % of NTSCI cases. Tuberculosis is an infectious disease caused by bacteria that typically attacks the lungs but can also damage other parts of the body like the spine and brain.
- Other causes of NTSCI commonly reported in research include inflammatory/auto-immune conditions, vascular conditions, and infections.
Pediatric SCITraumatic injury is the most common cause of SCI in adults, while non-traumatic causes are more common in children. The most common non-traumatic causes of pediatric SCI include congenital anomalies, spinal cord tumors, infections, and vascular malformations. Common traumatic causes of pediatric SCIs include motor vehicle accidents, falls, sports-related injuries and iatrogenic harm. Visit SCIRE Professional for more information on Pediatric SCI. |
Where in the World?
 An estimated 20.6 million individuals live with SCI globally. It appears that the incidence of NTSCI is increasing due to the ageing population in many countries. Indeed, in some countries the incidence of NTSCI is now higher than that of traumatic SCI.
An estimated 20.6 million individuals live with SCI globally. It appears that the incidence of NTSCI is increasing due to the ageing population in many countries. Indeed, in some countries the incidence of NTSCI is now higher than that of traumatic SCI.
There is a general lack of information about incidence and types of NTSCI worldwide. That said, developed countries tend to have a higher proportion of cases caused by degenerative conditions (32%) and from tumours (25%) in Western Europe. Developing countries, in comparison, tend to have a higher proportion of NTSCI acquired from infection, particularly tuberculosis and HIV, though tumours are also reported as a major cause. There are many gaps in tracking the global rates of NTSCI.
The onset of NTSCI may be slow and gradual and be related to a progressive condition or a complication from another medical event. Onset can range from minutes to months depending on the cause of injury.
Compared to traumatic SCI, those with NTSCI:
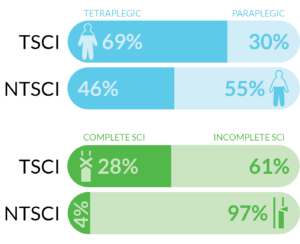
TSCI = traumatic spinal cord injury; NTSCI = non-traumatic spinal cord injury
- are more likely to have paraplegia
- are more likely to have an incomplete injury
- spend less time in rehabilitation and have reduced hospital charges
- have similar discharge destinations.
“Invisible” disability
Compared to people with traumatic SCI, people with NTSCI are more likely to have regained some walking ability when they are discharged from rehabilitation. People with SCI who can walk may face unique physical and psychosocial challenges. The use of mobility devices for walking likes canes and walkers might cause more fatigue and/or pain then a wheelchair. The absence of a wheelchair as a clear indicator of disability can result in misunderstanding and judgement from others due to lack of awareness about people with SCI who can walk. Some feel that they exist in a “grey zone” where they are neither fully abled nor disabled and experience “invisible” challenges.
Some examples of challenges include:
- Misunderstanding from others about the severity of their injury and the impairments they live with.
- Feeling out of place in SCI programs or in the SCI community, especially when the program or space is not built with people who can walk in mind (e.g., no places to sit).
- Unwanted attention and scrutiny when in public or in social situations due to an abnormal gait or assistive devices.
- Lack of empathy from others when they pass as not disabled (e.g., “Can you hurry up? Why are you so slow?”).
There is a need for more programs and services that are welcoming to and consider the needs of people with SCI who can walk. If you or someone you know is struggling with finding community and services as a person with SCI who can walk, it can be helpful to talk to health professionals or peers with similar injuries and experiences. Peer support has been proven to improve adjustment to life after injury and general wellbeing through social/emotional support and sharing knowledge. If pain or fatigue with walking are a problem, it may also be beneficial to consider the intermittent use of wheeled mobility devices.
Read our article on SCI Basics for more information about types of SCI!
Rehabilitation common to all types of SCI
Most of the rehabilitation process will be similar between traumatic and NTSCI while treatment of the underlying conditions that cause NTSCI will vary. Rehabilitation common to both traumatic SCI and NTSCI includes:
- Education about the SCI and the related medical problems that need to be managed.
- Complication management and prevention: In people with all types of SCI, complications like urinary tract infection, pneumonia, pressure ulcers, spasticity and neuropathic pain are common and managed in rehabilitation. Prevention and education are essential to minimize complications.
- Physical and occupational therapy: Physical therapists work with patients to regain mobility, strength, and coordination. Occupational therapists focus on helping patients adapt to their new circumstances, relearn daily living skills, and regain independence. Both are critical essential to rehabilitation after SCI.
- Assistive devices: Mobility aids, adaptive equipment, assistive technologies, and other supports like cushions and mattresses can significantly improve the quality of life for people with SCIs. These devices help with mobility, communication, daily tasks, and prevent complications like pressure ulcers.
- Pain management: Chronic pain is a common issue in that can be managed with medications, nerve blocks, or other interventions to alleviate discomfort.
- Bladder and bowel training: Medical treatments can be used to treat bladder and bowel problems. Training also includes learning how to manage your bladder and bowel care after rehabilitation.
- Psychological support: Psychological support and counseling can help individuals and their families navigate the challenging emotional aspects of coping with SCI.
- Community reintegration: In preparation for leaving rehabilitation, the health team should provide support in finding local resources and services, managing finances, returning to regular life activities, and adapting the home for SCI.
Read our article on Understanding Rehabilitation for more information!
Read our articles on the areas listed here and many other Topics!
Rehabilitation unique to non-traumatic SCI
Predicting recovery
NTSCI presents unique rehabilitation challenges. Given that those with NTSCI tend to be older, there is an increased likelihood of chronic conditions such as arthritis, diabetes, cardiovascular disease, obesity, and other conditions. These comorbidities can negatively impact rehabilitation and recovery.
Predicting rehabilitation outcomes after injury is particularly difficult in those with a progressive NTSCI, where the condition underlying the SCI leads to a deterioration over time compared to those with a non-progressive cause of NTSCI. The cause of NTSCI is an important predictor of outcomes, length of stay, and survival.
Considering the older age of many people with NTSCI, the various possible chronic health conditions that they may have, and that many NTSCI are incomplete, it can be very hard to predict the recovery from NTSCI. Making comparisons with traumatic SCI is also very hard for the same reasons.
Access to rehabilitation services
People with NTSCI have improved recovery outcomes when they are treated in a spinal-specific rehabilitation unit rather than in general rehabilitation. Clinicians agree that that a spinal rehabilitation unit that specializes in NTSCI is the ideal setting for treatment. However, there is a tendency for spinal rehabilitation units to give preference to traumatic SCI when admitting clients as NTSCI is considered less urgent and they may exclude older patients or those with metastatic cancer presumably referring them to gerontology and oncology units, respectively.
Concurrent treatment
Depending on the cause of the NTSCI, some people will undergo treatments for the underlying condition at the same time as rehabilitation. This could include surgeries, radiation therapy and chemotherapy for tumours, immunosuppressant medications for auto-immune conditions, antibiotics for bacterial infections, etc. The rehabilitation unit needs to be aware of these treatments for safety and to optimally plan treatments and rehabilitation therapy. Some treatments for underlying conditions can be draining and negatively impact rehabilitation if therapy is scheduled soon after.
Diagnosis of underlying cause
There is also a possibility for people with NTSCI to be admitted to rehabilitation without a diagnosis or with an incorrect diagnosis of the underlying condition. In these situations, rehabilitation clinicians and therapists may end up being involved in determining the correct diagnosis.
The many different types of NTSCI can be grouped into three categories: congenital, genetic, and acquired. Each will have their unique presentation and treatment needs. That said, the large majority of NTSCIs result from acquired conditions. In developed countries, most acquired NTSCIs are degenerative conditions and tumors, while developing countries tend to have a higher proportion from infection.
Those with NTSCI are more likely to be older, female, have paraplegia and have an incomplete injury when compared to those with traumatic SCI.
Much of NTSCI rehabilitation is similar to traumatic SCI rehabilitation, though the rehabilitation stay is shorter and less costly.
For a review of how we assess evidence at SCIRE Community and advice on making decisions, please see SCIRE Community Evidence.
Parts of this page have been adapted from the SCIRE Professional “Rehabilitation Practices” Module available from: scireproject.com/evidence/rehabilitation-practices/factors-affecting-rehabilitation-outcomes/traumatic-vs-non-traumatic-sci/
Evidence for “What causes non-traumatic SCI?” is based on:
Molinares DM, Gater DR, Daniel S, Pontee NL. Nontraumatic Spinal Cord Injury: Epidemiology, Etiology and Management. J Pers Med. 2022 Nov 8;12(11):1872.
New PW, Reeves RK, Smith É, Eriks-Hoogland I, Gupta A, Scivoletto G, et al. International retrospective comparison of inpatient rehabilitation for patients with spinal cord dysfunction: Differences according to etiology presented in part to the international spinal cord society, September 2-5, 2012, London, United Kingdom. Arch Phys Med Rehabil. 2016 Mar 1;97(3):380–5.
New PW, Marshall R. International Spinal Cord Injury Data Sets for non-traumatic spinal cord injury. Spinal Cord. 2014 Feb 8;52(2):123–32.
Klimo P, Rao G, Brockmeyer D. Congenital Anomalies of the Cervical Spine. Neurosurg Clin N Am. 2007 Jul;18(3):463–78.
Hart DJ. Syringomyelia. Encyclopedia of the Neurological Sciences. 2014 Jan 1;378–81.
Kuo DT, Tadi P. Cervical Spondylosis. In: StatPearls. StatPearls Publishing; 2023.
Evidence for “Who gets non-traumatic SCI?” is based on:
Cosar SNS, Yemisci OU, Oztop P, Cetin N, Sarifakioglu B, Yalbuzdag SA, et al. Demographic characteristics after traumatic and non-traumatic spinal cord injury: a retrospective comparison study. Spinal Cord 2010 48:12. 2010 May 4;48(12):862–6.
McCaughey EJ, Purcell M, McLean AN, Fraser MH, Bewick A, Borotkanics RJ, et al. Changing demographics of spinal cord injury over a 20-year period: a longitudinal population-based study in Scotland. Spinal Cord. 2016 Apr 13;54(4):270–6.
New PW, Cripps RA, Bonne Lee B. Global maps of non-traumatic spinal cord injury epidemiology: towards a living data repository. Spinal Cord 2013 52:2. 2013 Jan 15;52(2):97–109.
Niemi-Nikkola V, Koskinen E, Väärälä E, Kauppila AM, Kallinen M, Vainionpää A. Incidence of Acquired Nontraumatic Spinal Cord Injury in Finland: A 4-Year Prospective Multicenter Study. Arch Phys Med Rehabil. 2021 Jan;102(1):44–9.
Smith É, Fitzpatrick P, Lyons F, Morris S, Synnott K. Epidemiology of non-traumatic spinal cord injury in Ireland – a prospective population-based study. J Spinal Cord Med. 2022;45(1):76–81.
Choi Y, Leigh JH, Jeon J, Lee GJ, Shin HI, Bang MS. Trends in the Incidence and Etiology of Non-Traumatic Spinal Cord Injury in Korea: A Nationwide Population-Based Study From 2007 to 2020. J Korean Med Sci. 2023 May 5;38(18).
Cunha NSC, Malvea A, Sadat S, Ibrahim GM, Fehlings MG. Pediatric Spinal Cord Injury: A Review. Children. 2023 Sep 1;10(9).
Jain NB, Ayers GD, Peterson EN, Harris MB, Morse L, O’Connor KC, et al. Traumatic Spinal Cord Injury in the United States, 1993–2012. JAMA. 2015 Jun 6;313(22):2236
DeVivo MJ, Vogel LC. Epidemiology of spinal cord injury in children and adolescents. J Spinal Cord Med. 2004;27 Suppl 1.
Safdarian M, Trinka E, Rahimi-Movaghar V, Thomschewski A, Aali A, Abady GG, et al. Global, regional, and national burden of spinal cord injury, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2023 Nov 1;22(11):1026–47.
New PW, Epi MC, Biering-Sørensen F. Review of the History of Non-traumatic Spinal Cord Dysfunction. Top Spinal Cord Inj Rehabil. 2017 Sep 1;23(4):285.
Kennedy P, Hasson L. An audit of demographics and rehabilitation outcomes in non-traumatic spinal cord injury. Spinal Cord 2016 54:11. 2016 Mar 22;54(11):1020–4.
Evidence for “How does non-traumatic SCI present?” is based on:
New PW, Marshall R. International Spinal Cord Injury Data Sets for non-traumatic spinal cord injury. Spinal Cord. 2014 Feb 8;52(2):123–32.
New PW, Cripps RA, Bonne Lee B. Global maps of non-traumatic spinal cord injury epidemiology: towards a living data repository. Spinal Cord 2013 52:2. 2013 Jan 15;52(2):97–109.
McKinley WO, Seel RT, Gadi RK, Tewksbury MA. Nontraumatic vs. traumatic spinal cord injury : A rehabilitation outcome comparison. Am J Phys Med Rehabil. 2001;80(9):693–9.
Citterio A, Franceschini M, Spizzichino L, Reggio A, Rossi B, Stampacchia G. Nontraumatic spinal cord injury: An Italian survey. Arch Phys Med Rehabil. 2004 Sep 1;85(9):1483–7.
Dionne A, Richard-Denis A, Lim • Victor, Mac-Thiong JM. Factors associated with discharge destination following inpatient functional rehabilitation in patients with traumatic spinal cord injury. Spinal Cord. 2021;59:642–8.
Franceschini M, Bonavita J, Cecconi L, Ferro S, Pagliacci MC, Ferro S, et al. Traumatic spinal cord injury in Italy 20 years later: current epidemiological trend and early predictors of rehabilitation outcome. Spinal Cord 2020 58:7. 2020 Jan 29;58(7):768–77.
Halvorsen A, Pettersen AL, Nilsen SM, Halle KK, Schaanning EE, Rekand T. Non-traumatic spinal cord injury in Norway 2012–2016: analysis from a national registry and comparison with traumatic spinal cord injury. Spinal Cord. 2019 Apr 14;57(4):324–30.
McKinley WO, Conti-Wyneken AR, Vokac CW, Cifu DX. Rehabilitative functional outcome of patients with neoplastic spinal cord compression. Arch Phys Med Rehabil [Internet]. 1996 Sep 1;77(9):892–5.
Jeawon M, Hase B, Miller S, Eng J, Bundon A, Chaudhury H, et al. Exploring the Quality of Life of People with Incomplete Spinal Cord Injury Who Can Ambulate. Disabilities. 2023 Oct 6;3(4):455–76.
Jeawon M, Hase B, Miller S, Eng JJ, Bundon A, Chaudhury H, et al. Understanding the experiences, needs, and strengths of people with incomplete spinal cord injury who can ambulate. Disabil Rehabil. 2024 Jan 30;46(3):546–55.
Evidence for “How is non-traumatic SCI treated?” is based on:
New PW. Non-traumatic spinal cord injury: what is the ideal setting for rehabilitation? Australian Health Review. 2006;30(3):353.
New PW, Eriks-Hoogland I, Scivoletto G, Reeves RK, Townson A, Marshall R, et al. Important Clinical Rehabilitation Principles Unique to People with Non-traumatic Spinal Cord Dysfunction. Top Spinal Cord Inj Rehabil. 2017 Oct;23(4):299–312.
Image credits
- Baby by Nick Abrams
- Different types of spina bifida by Centers for Disease Control and Prevention, Public Domain
- DNA by Adrien Coquet
- old man by Gan Khoon Lay
- Spinal Tumors Illustration by Thom Graves, CMI; used with permission of Weill Cornell Medicine Neurological Surgery.
- The Blue Marble (remastered) NASA/Apollo 17 Crew, Public Domain
- TSCI/NTSCI 1 ©SCIRE
- TSCI/NTSCI 2 ©SCIRE





