Author: SCIRE Community Team | Reviewer: Andrei Krassioukov and Janice Eng | Published: 12 October 2017 | Updated: ~
Autonomic dysreflexia is a medical emergency that can happen after spinal cord injury (SCI). This page provides an overview of what autonomic dysreflexia is and how it is managed.
For information about emergency treatments, see How is autonomic dysreflexia treated?
Key Points
- Autonomic dysreflexia is a potentially life-threatening medical emergency that can affect people with SCI at T6 and above.
- Autonomic dysreflexia involves a sudden rise in blood pressure, which may be accompanied by heart rate changes, headaches, sweating, and other symptoms.
- Autonomic dysreflexia can be triggered by any strong, irritating, or ‘painful’ stimulus below the level of the injury, such as bladder and bowel problems, tight clothing, or pressure ulcers.
- Emergency treatment involves sitting upright, monitoring blood pressure, loosening tight clothing, and searching for and eliminating the cause of the episode (usually problems related to the bladder, bowel, and skin). If the episode does not resolve, emergency medical treatment involves the use of medications to rapidly lower blood pressure.
- Prevention is an important part of managing autonomic dysreflexia. This typically involves maintaining good bladder, bowel, and skin care, and using medications during procedures that could trigger autonomic dysreflexia.
Autonomic dysreflexia (also called autonomic hyperreflexia) is a potentially life-threatening medical condition that can happen after spinal cord injury. Autonomic dysreflexia involves a sudden rise in blood pressure accompanied by changes in heart rate and other symptoms like headaches and sweating. The blood pressure responses in the body are poorly controlled because of the SCI and can become dangerously high.
Autonomic dysreflexia typically affects people with SCI at T6 and above (although occasionally as low as T8). In general, people with higher level of injury and complete injuries are more likely to experience autonomic dysreflexia. Autonomic dysreflexia can occur at any time after the SCI.

Autonomic dysreflexia involves a sudden rise in blood pressure of 20 to 30 mmHg above your normal systolic blood pressure. Since the normal blood pressure of people with SCI is often 20 to 30 mmHg lower than in those without SCI, blood pressure can be in a range that is commonly considered ‘normal’ or ‘slightly elevated’ and still be high for that person.
This rise in blood pressure is usually accompanied by symptoms. Symptoms will be different for everyone and can range from some mild discomfort to life threatening and severe.
Signs and symptoms of autonomic dysreflexia
- A sudden rise in systolic blood pressure (20 to 30 mmHg above normal)
- Changes in heart rate, usually a slow heart rate which sometimes becomes rapid
- A pounding or throbbing headache
- Sweating, flushing, or blotching of the skin above the SCI
- Goosebumps or hair standing on end above the SCI
- Dry and pale skin below the SCI
- Worsening of muscle spasms
- A metallic taste in the mouth
- Feeling anxious or a feeling of ‘impending doom’
- A stuffy or runny nose
- Blurred vision or seeing spots
- Nausea
- Difficulty breathing
 Autonomic dysreflexia can be life threatening when severe. If left untreated, uncontrolled elevated blood pressure can lead to serious conditions like stroke, heart attack, detached retinas, seizures, and even death.
Autonomic dysreflexia can be life threatening when severe. If left untreated, uncontrolled elevated blood pressure can lead to serious conditions like stroke, heart attack, detached retinas, seizures, and even death.
Although these complications are uncommon, it is important that autonomic dysreflexia is recognized and treated immediately. Talk to your health providers about setting up a plan for managing episodes of autonomic dysreflexia as soon as they happen.
Autonomic dysreflexia can be triggered by any strong stimulation below the SCI, including anything that could be considered uncomfortable, irritating, or painful if it could be felt. For example, a wound can trigger autonomic dysreflexia even if it the person does not feel it. Autonomic dysreflexia can also be caused by normal body processes that are strongly stimulating, such as a full bladder or sexual stimulation. The most common triggers are related to the bladder or bowel.
Common causes of autonomic dysreflexia
- A bladder that is full – this may be caused by a blocked or kinked catheter, an overfilled collection bag, or incomplete emptying of urine
- Other bladder causes such as urinary tract infections or bladder procedures (like when putting in a catheter)
- A bowel that is full or impacted (contains a hard mass of stool that is stuck)
- Other bowel causes such as constipation, infections, haemorrhoids, or bowel procedures (such as during digital rectal stimulation)
- Pressure ulcers, wounds, or burns
- Skin irritation from pressure, pinching, ingrown toenails, or tight clothing
- Hot or cold temperatures
- Strong sexual stimulation
- Menstrual cramping
- Labour and delivery
- Broken bones and heterotopic ossification
- Surgery and other medical procedures (including functional electrical stimulation)
- Ulcers and other abdominal conditions
Autonomic dysreflexia is caused by dysfunction of the autonomic nervous system after SCI that leads to poorly controlled blood pressure responses.
The autonomic nervous system
The autonomic nervous system controls largely unconscious bodily processes such as blood pressure, heart rate, breathing rate, body temperature, digestion, bladder, bowel, and sexual function. It has two divisions:
The sympathetic nervous system prepares the body for stressful or emergency situations. It is often called the ‘fight or flight’ system, because it prepares the body for action. For example, it increases heart rate and constricts blood vessels.
The parasympathetic nervous system prepares the body for normal, non-emergency situations. It is often called the ‘rest and digest’ system, because it allows the body to restore itself. For example, it slows heart rate and relaxes blood vessels.
The sympathetic and parasympathetic systems have different (and often opposite) effects on the organs and work together to control bodily functions according to the situation.

Blood pressure is carefully controlled by the autonomic nervous system to ensure that circulation works properly. The body monitors blood pressure and makes adjustments to maintain blood pressure within an optimal range. This is done in part by tightening (constricting) or relaxing (dilating) the blood vessels and changing heart rate.
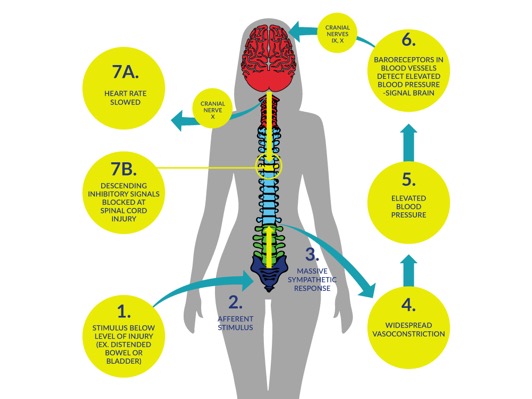
What happens in autonomic dysreflexia
 When the body below the SCI detects strong stimulation, it activates the sympathetic nervous system, causing the constriction of blood vessels in the lower body. This causes blood pressure to rise.
When the body below the SCI detects strong stimulation, it activates the sympathetic nervous system, causing the constriction of blood vessels in the lower body. This causes blood pressure to rise.

Pressure sensors in the arteries then detect the elevated blood pressure and relay this message to the brain. Under normal circumstances, the brain sends signals through the spinal cord and cranial nerves to relax the blood vessels and slow heart rate. This restores blood pressure to normal.
However, when there is an SCI, the signal to relax the blood vessels is blocked from travelling to the lower body. Because of this, the blood vessels remain constricted and the body cannot restore blood pressure to normal. This causes the uncontrolled elevated blood pressure that happens during autonomic dysreflexia.
Why does autonomic dysreflexia happen at T6 and above?
The level of T6 is important because nerves from this part of the spinal cord constrict a large group of blood vessels in the abdomen called the splanchnic vascular bed. These blood vessels contain a large volume of blood, so when the blood vessels are constricted, it causes the blood pressure to rise significantly. Injuries below T6 do not usually cause enough of a change in blood pressure to cause autonomic dysreflexia.

Autonomic dysreflexia is a medical emergency and needs to be treated immediately. Emergency treatment involves a series of steps to lower blood pressure and remove the cause of the episode. If these steps are unsuccessful, emergency medical treatments are used to try to reduce blood pressure quickly.
Immediate treatment of autonomic dysreflexia
- Get into an upright sitting position (or bring your head up) and if possible, lower your legs
- If possible, check your blood pressure and re-check it every 5 minutes
- Loosen tight clothing or devices (including tape, straps, and equipment)
- Search for and remove the cause of the episode:
- Check for bladder problems
- If your catheter is kinked or blocked, reposition or flush the catheter
- If your bladder or collection bag is full, drain
- If your urine is cloudy or smells bad, it could be a bladder infection – contact a health provider
- Check for bowel problems
- If your bowel is full, use your bowel management routine to empty it (such as digital rectal stimulation)
- Check for other problems like hemorrhoids
- Check for bladder problems
- Check for skin problems and remove them if possible (such as ingrown toenails, skin irritation, pressure ulcers, infections, or wounds)
- Check for other problems (such as broken bones)
- Seek medical attention if blood pressure remains high (150 mmHg or above) after following these steps
If blood pressure returns to normal, continue to monitor your symptoms and blood pressure to make sure they do not return and report the incident to a health provider.
This approach is considered to be the most effective first treatment for autonomic dysreflexia. However, although this procedure is commonly used and recommended by health providers, it is supported primarily by expert opinion rather than evidence from research studies.
Emergency medical treatments
 If the steps above do not reduce blood pressure and it remains high (150 mmHg or above), seek emergency medical attention by calling an ambulance or visiting an emergency department. Emergency medical treatments involve the use of medications that rapidly lower blood pressure. The health providers may also run a series of tests to identify the cause of the episode if one has not been found.
If the steps above do not reduce blood pressure and it remains high (150 mmHg or above), seek emergency medical attention by calling an ambulance or visiting an emergency department. Emergency medical treatments involve the use of medications that rapidly lower blood pressure. The health providers may also run a series of tests to identify the cause of the episode if one has not been found.
The most commonly used drugs for autonomic dysreflexia are:
- Captopril
- Nifedipine (Adalat, Procardia)
- Nitrates (Nitroglycerine, Depo-Nit, Nitrostat, Nitrol, Nitro-Bid)
However, there is little research evidence to suggest which medications work best for treating autonomic dysreflexia. Speak to your health providers for more information about medications used in autonomic dysreflexia emergencies.
The most effective way of managing autonomic dysreflexia is to prevent triggering it in the first place. People who get autonomic dysreflexia may be able to take steps to avoid triggering episodes, especially during procedures that are known to cause autonomic dysreflexia.
Learn to recognize autonomic dysreflexia and your triggers
In order to be able to manage episodes of autonomic dysreflexia, it is important to be able to recognize an episode and know what to do when it happens.
- Learn about and educate family members and friends about what autonomic dysreflexia is, how to recognize it, and what to do if it happens.
- Work with your health providers to identify your risk for autonomic dysreflexia, how to prevent it, and what to do if it happens.
- Carry an autonomic dysreflexia medical emergency card. These wallet-sized cards describes autonomic dysreflexia and its symptoms and treatments for use in an emergency – it can be used to quickly describe the condition and its treatment to your health providers.
Preventing autonomic dysreflexia from bladder problems
 Bladder problems are the most common triggers of autonomic dysreflexia. Methods that may be used to prevent bladder problems from triggering autonomic dysreflexia include:
Bladder problems are the most common triggers of autonomic dysreflexia. Methods that may be used to prevent bladder problems from triggering autonomic dysreflexia include:
- Maintaining a bladder routine is the most important way to prevent problems like bladder distension and urinary tract infections.
- Preventing irritation during bladder procedures (such as catheterization) using anaesthetic medications (such as capsaicin or lidocaine).
- Managing reflex spasms of the bladder muscles (detrusor hyperreflexia) through methods including botulinum toxin (Botox) injections or sacral denervation (deafferentation) surgery.
- Bladder surgeries, such as bladder augmentation, may be used for some individuals with bladder dysfunction after an SCI and have been shown to help reduce episodes of autonomic dysreflexia.
See our article on Urinary Tract Infections to learn more!
Preventing autonomic dysreflexia from bowel problems
 Bowel problems are another common trigger of autonomic dysreflexia. Methods that may be used to prevent bowel problems from triggering autonomic dysreflexia include:
Bowel problems are another common trigger of autonomic dysreflexia. Methods that may be used to prevent bowel problems from triggering autonomic dysreflexia include:
- Maintaining a bowel routine and management (including fibre and fluid intake) to prevent problems like bowel distension, faecal impaction, and constipation.
- Preventing irritation during invasive bowel procedures or medical procedures (such as digital rectal stimulation) using anesthetics (such as lidocaine gel or lidocaine anal blocks).
- Bowel surgeries, such as colostomy or ileostomy, may be considered for people with chronic bowel problems that cause autonomic dysreflexia and other problems.
See our article on Bowel Changes after Spinal Cord Injury for more information!
Preventing autonomic dysreflexia from skin problems
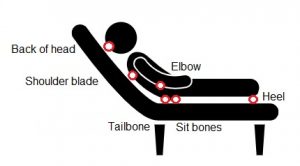 Pressure ulcers, ingrown toenails, and burns can all be additional causes of autonomic dysreflexia. Methods that may be used to prevent skin problems from triggering autonomic dysreflexia include:
Pressure ulcers, ingrown toenails, and burns can all be additional causes of autonomic dysreflexia. Methods that may be used to prevent skin problems from triggering autonomic dysreflexia include:
- Maintain an effective skin care routine, which involves regular pressure relief, inspection of skin, and proper cleaning.
- Avoid wearing tight clothing and keep clothing and sheets smooth.
- Maintain regular foot care.
- Treat skin injuries and infections early.
Preventing autonomic dysreflexia from other causes
- Although individuals with SCI do not have sensation in areas where surgeries may occur, anesthesia should be used to avoid triggering autonomic dysreflexia during surgery.
- Anesthesia (spinal or epidural if possible) is needed with vaginal, Caesarean, or instrumental delivery to prevent autonomic dysreflexia during labour.
- Be aware that strong sexual stimulation can cause autonomic dysreflexia. Take precautions and be aware of your responses to stimulation.
The bottom line
Autonomic dysreflexia is a serious medical condition that requires immediate recognition and treatment. First line treatment involves sitting up, removing tight clothing, and removing the cause of episode. This is supported by expert opinion. Emergency medical treatments for episodes of autonomic dysreflexia involve fast acting anti-hypertensive agents such as nifedipine, nitrates, and captopril, although the best treatment to use has not been determined.
It is best to discuss treatment options with your health providers to find out which treatments are suitable for you. For a review of how we assess evidence at SCIRE Community and advice on making decisions, please see SCIRE Community Evidence.
Krassioukov A, Blackmer J, Teasell RW, Eng JJ (2014). Autonomic Dysreflexia Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors.
Spinal Cord Injury Rehabilitation Evidence. Version 5.0. Vancouver: p 1- 35. Available from: http://scireproject.com/evidence/rehabilitation-evidence/autonomic-dysreflexia.
Barton CH, Khonsari F, Vaziri ND, Byrne C, Gordon S, Friis R. T http://scireproject.com/evidence/rehabilitation-evidence/autonomic-dysreflexia The effect of modified transurethral sphincterotomy on autonomic dysreflexia. J Urol 1986;135:83-85.http://scireproject.com/evidence/rehabilitation-evidence/autonomic-dysreflexia-re/
Sidi AA, Becher EF, Reddy PK, Dykstra DD. Augmentation enterocystoplasty for the management of voiding dysfunction in spinal cord injury patients. J Urol 1990;143:83-85.
Perkash I. Transurethral sphincterotomy provides significant relief in autonomic dysreflexia in spinal cord injured male patients: Long-term followup results. J Urol 2007;177:1026-1029.
Ke QS, Kuo HC. Transurethral incision of the bladder neck to treat bladder neck dysfunction and voiding dysfunction in patients with high-level spinal cord injuries. Neuro Uro 2010;29:748-752.
Hohenfellner M, Pannek J, Botel U, Bahms S, Pfitzenmaier J, Fichtner J, et al. Sacral bladder denervation for treatment of detrusor hyperreflexia and autonomic dysreflexia. Urol 2001;58:28-32.
Kutzenberger J. Surgical therapy of neurogenic detrusor overactivity (hyperreflexia) in paraplegic patients by sacral deafferentation and implant driven micturition by sacral anterior root stimulation: methods, indications, results, complications, and future prospects. Acta Neurochir Suppl 2007;97:333-339.
Coggrave MJ, Ingram RM, Gardner BP, Norton CS. The impact of stoma for bowel management after spinal cord injury. Spinal Cord 2012;50:848-852.
Cosman BC, Vu TT. Lidocaine anal block limits autonomic dysreflexia during anorectal procedures in spinal cord injury: a randomized, double-blind, placebo-controlled trial. Dis Colon Rectum 2005;48:1556-1561.
Cosman BC, Vu TT, Plowman BK. Topical lidocaine does not limit autonomic dysreflexia during anorectal procedures in spinal cord injury: a prospective, double-blind study. Int J Colorectal Dis 2002;17:104-108.
Furusawa K, Sugiyama H, Tokuhiro A, Takahashi M, Nakamura T, Tajima F. Topical anesthesia blunts the pressor response induced by bowel manipulation in subjects with cervical spinal cord injury. Spinal Cord 2009;47:144-148.
Cross LL, Meythaler JM, Tuel SM, Cross LA. Pregnancy, labor and delivery post spinal cord injury. Paraplegia 1992;30:890-902.
Hughes SJ, Short DJ, Usherwood MM, Tebbutt H. Management of the pregnant woman with spinal cord injuries. Br J Obstet Gynaecol 1991;98:513-518.
Cross LL, Meythaler JM, Tuel SM, Cross AL. Pregnancy following spinal cord injury. West J Med 1991;154:607-611.
Skowronski E, Hartman K. Obstetric management following traumatic tetraplegia: case series and literature review. Aust N Z J Obstet Gynaecol 2008;48:485-491.
Lambert DH, Deane RS, Mazuzan JE. Anesthesia and the control of blood pressure in patients with spinal cord injury. Anesth Analg 1982;61:344-348.
Eltorai IM, Wong DH, Lacerna M, Comarr, AE, Montroy R. Surgical aspects of autonomic dysreflexia. J Spinal Cord Med 1997;20:361-364.
Matthews JM, Wheeler GD, Burnham RS, Malone LA, Steadward RD. The effects of surface anaesthesia on the autonomic dysreflexia response during functional electrical stimulation. Spinal Cord 1997;35:647-651.
Kim JH, Rivas DA, Shenot PJ, Green B, Kennelly M, Erickson, JR, O’Leary M, Yoshimura N, Chancellor MB. Intravesical resiniferatoxin for refractory detrusor hyperreflexia: a multicenter, blinded, randomized, placebo-controlled trial. J Spinal Cord Med 2003;26:358-363.
Giannantoni A, Di Stasi SM, Stephen RL, Navarra P, Scivoletto G, Mearini E, Porena M. Intravesical capsaicin versus resiniferatoxin in patients with detrusor hyperreflexia: a prospective randomized study. J Urol 2002;167:1710-1714.
Igawa Y, Satoh T, Mizusawa H, Seki S, Kato H, Ishizuka O, Nishizawa O. The role of capsaicin-sensitive afferents in autonomic dysreflexia in patients with spinal cord injury. BJU Int 2003;91:637-641.
Dykstra DD, Sidi AA, Scott AB, Pagel JM, Goldish GD. Effects of botulinum A toxin on detrusor-sphincter dyssynergia in spinal cord injury patients. J Urol 1988;139:919-922.
Schurch B, Stohrer M, Kramer G, Schmid DM, Gaul G, Hauri D. Botulinum-A toxin for treating detrusor hyperreflexia in spinal cord injured patients: a new alternative to anticholinergic drugs? Preliminary results. J Urol 2000;164:692-697.
Chen SL, Bih LI, Huang YH, Tsai SJ, Lin TB, Kao YL. Effect of single botulinum toxin A injection to the external urethral sphincter for treating detrusor external sphincter dyssynergia in spinal cord injury. J Rehabil Med 2008;40:744-748.
Kuo HC. Satisfaction with urethral injection of botulinum toxin A for detrusor sphincter dyssynergia in patients with spinal cord lesion. Neurourol Urodyn 2008; 27: 793-796.
Chen SF, Kuo HC. Improvement in autonomic dysreflexia after detrusor onabotulinumtoxinA injections in patients with chronic spinal cord injuries. Tzu Chi Medical Journal 2012;24:201-204.
Giannantoni A, Di Stasi SM, Scivoletto G, Mollo A, Silecchia A, Fuoco U, Vespasiani G. Autonomic dysreflexia during urodynamics. Spinal Cord 1998;36:756-860.
Bycroft J, Shergill I, Choong E, Arya N, Shah P. Autonomic dysreflexia: a medical emergency. Postgraduate Medical Journal. 2005;81(954):232-235.
Image Credits
- Image by SCIRE Professional Team
- Headache ©8thBox, CC0 1.0
- Doctor1 ©Clker-Free-Vector-Images, CC0 1.0
- Voltage ©Clker-Free-Vector-Images, CC0 1.0
- Highbp ©stevepb, CC0 1.0
- Headshock ©Geralt, CC0 1.0
- Body vessels © Clker-Free-Vector-Images, CC0 1.0
- Stetho ©Clker-Free-Vector-Images, CC0 1.0
- Ambulance ©Pettycon, CC0 1.0
- Excretory system ©Olena Panasovska, CC BY 3.0 US
- Digestive System ©Design Science, CC0 1.0
- Modified from: Man Resting on Long Chair ©Gan Khoon Lay, CC BY 3.0
- Tasklist ©Pettycon, CC0 1.0