Authors: Dominik Zbogar and Sharon Jang | Reviewer: Susan Harkema | Published: 14 February 2022 | Updated: ~
Key Points
- Epidural stimulation is a treatment that sends electrical signals to the spinal cord.
- Epidural stimulation requires a surgical procedure to implant electrodes close to the spinal cord.
- One of the ways epidural stimulation works is by replacing the signals that would normally be sent from the brain to the spinal cord before spinal cord injury (SCI).
- Epidural stimulation affects numerous systems. Stimulation aimed at activating leg muscles may potentially also affect bowel, bladder, sexual, and cardiovascular function.
- Studies of epidural stimulation in spinal cord injury (SCI) generally do not include a comparison group without stimulation. The benefits of epidural stimulation that have been reported have been in small numbers of participants. So, while reports thus far are encouraging, more research is necessary.
- Because it is in the research and development phase, epidural stimulation for spinal cord injury is not part of standard care nor is it a readily available treatment.
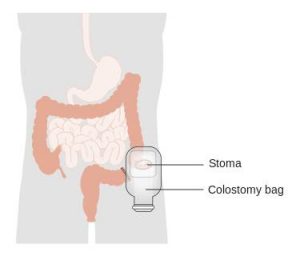
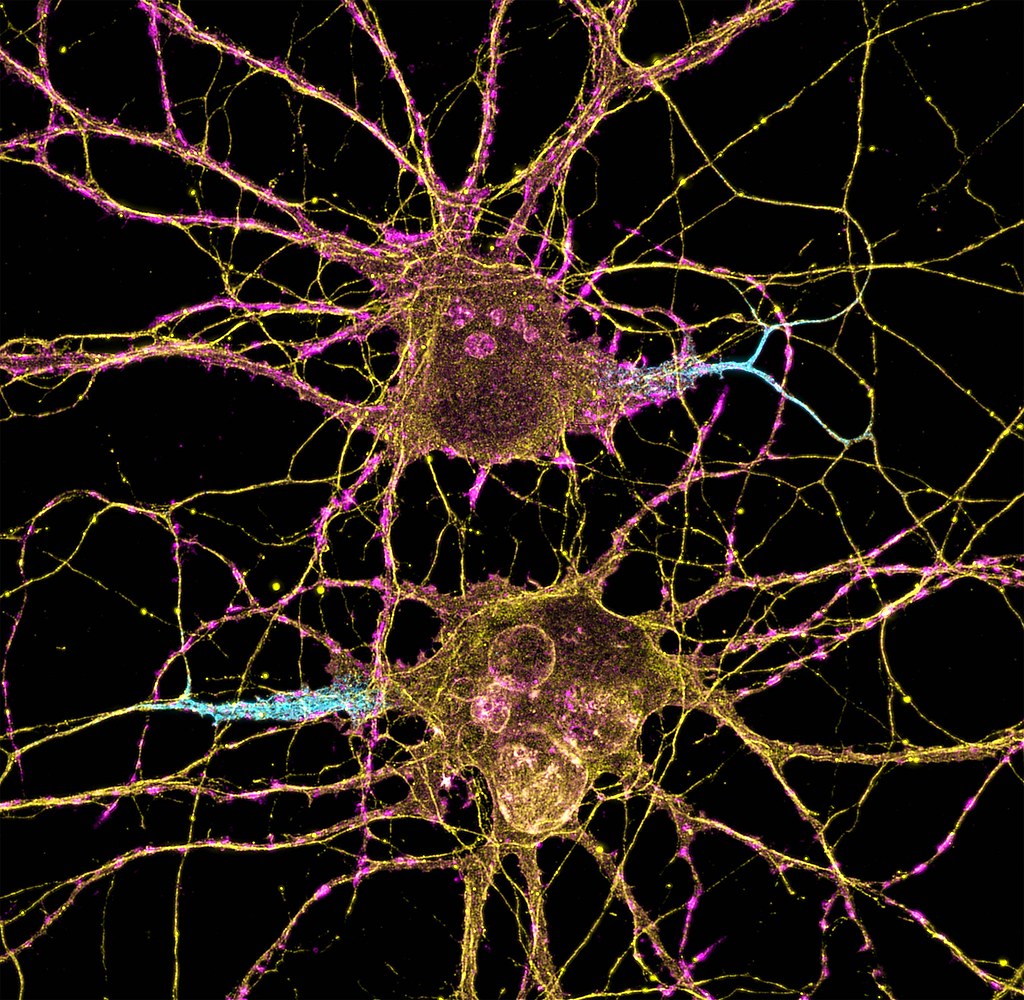
Neuromodulation is a general term for any treatment that changes or improves nerve pathways. Different types of neuromodulation can work at different sites along the nervous system (e.g., brain, nerves, spinal cord) and may or may not be invasive (i.e., involve surgery). Epidural stimulation (also known as epidural spinal cord stimulation or direct spinal cord stimulation) is a type of invasive neuromodulation that stimulates the spinal cord using electrical currents. This is done by placing an electrode on the dura (the protective covering around the spinal cord).
To read more about other types of neuromodulation used in SCI, access these SCIRE Community articles: Functional Electrical Stimulation (FES), Transcutaneous Electrical Nerve Stimulation (TENS), sacral nerve stimulation, and intrathecal Baclofen.
 |  |
 |  |
Watch our neuromodulation series videos! Our experts explainexperimental to more commonplace applications, and individuals with SCI describe how neuromodulation has affected their lives.
What is “an Epidural”?
Epi- is a prefix and means “upon”, and the dura (full name: dura mater) is a protective covering of the spinal cord. So epidural means “upon the dura”, and in the context of epidural stimulation, this is where the electrodes that stimulate the spinal cord are placed. Yes, it is also possible to have sub-dural (under the dura) or endo-dural (within the dura) electrode placement. And, there are more layers between the dura and the spinal cord, not to mention the spinal cord itself where electrodes could be placed in what is called intraspinal microstimulation. The benefit of being beneath the dura and closer to the spinal cord is that there is a more direct stimulation. Having the electrode closer to the spinal cord allows more precision with the signal going more directly to the neurons.
The drawback is that more complications can arise with closer placement because the electrodes are in the spinal cord tissue. Such placement is currently rare, experimental, or non-existent but that will change as the technology advances. Intraspinal microstimulation has been tested in animal models and is in the process of being translated to humans.
 You are probably familiar with the term “epidural” already, as it is often mentioned in relation to childbirth. If a new mother says she had an epidural, what she usually means is that she had pain medication injected into the epidural space for the purpose of managing pain during birth.
You are probably familiar with the term “epidural” already, as it is often mentioned in relation to childbirth. If a new mother says she had an epidural, what she usually means is that she had pain medication injected into the epidural space for the purpose of managing pain during birth.
We specifically discuss epidural spinal cord stimulation in this article. Spinal cord stimulation can also be applied transcutaneously. This type of spinal cord stimulation is non-invasive as the stimulating electrodes are placed on the skin. With transcutaneous stimulation, the signal has to travel a greater distance through muscle, fat, and other tissues, which means the ability to be precise with stimulation is hampered. However, it does allow for more flexibility in electrode placement and does not require surgery. There is research published or underway investigating the impact of transcutaneous stimulation in some of the areas discussed above, including hand, leg, and cardiovascular function.

Normally, input from your senses travels in the form of electrical signals through the nerves, up the spinal cord, and reaches the brain. The brain then tells the muscles or organs what to do by sending electrical signals back down the spinal cord. After a spinal cord injury, this pathway is disrupted, preventing electrical signals from traveling below the level of injury to reach where they need to go. However, the nerves, muscles, and organs can still respond below the injury to electrical signals.
Epidural stimulation works by helping the network of nerves in the spinal cord below the injury function better and take advantage of any leftover signals from the spinal cord. To do so, the stimulation must be fine-tuned to make sure the amount of stimulation is optimal for each person and a specific function, such as moving the legs.
Recent studies of the role of epidural stimulation on standing and walking have noted unexpected beneficial changes in some participants’ bowel, bladder, sexual, and temperature regulation function. This highlights both the potential for epidural stimulation to improve quality of life in multiple ways and that much research remains to be done to understand how epidural stimulation affects the body.
There may still be spared connections in the spinal cord with a complete injury.
How can someone with a complete injury regain movement control with epidural stimulation?
Being assessed with a complete injury implies that there is no spared function below the injury. However, scientists are finding that this may not be the case. Studies have found that even with a complete loss of sensory and motor function, there may be some inactive connections that are still intact across the injury site. These remaining pathways may be important for regaining movement or other functions. Another hypothesis is that epidural stimulation in combination with training may encourage stronger connections across the level of injury. Although these pathways may provide some substitution for the injured ones, they are not as effective as non-injured pathways across the injury level.
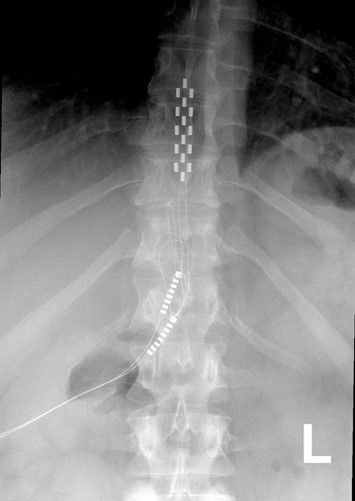
When it is decided that an individual will receive epidural stimulation, a health professional, such as a neurosurgeon, will perform an assessment of the spinal cord using magnetic resonance imaging (MRI) to determine the best place to implant the electrodes.
In most of the studies mentioned in this article, the electrodes were placed between the T9-L1 levels, though researchers are investigating the impact of epidural stimulation on hand function.
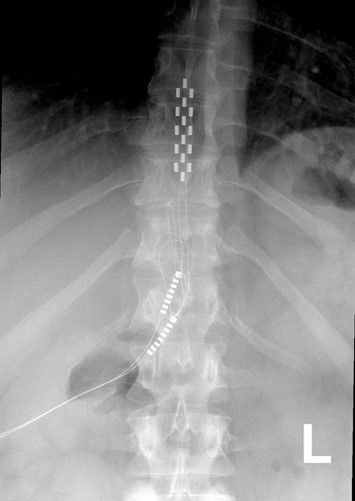
Xray image of wires connecting power and signal to electrodes (red circle) placed on a spinal cord.
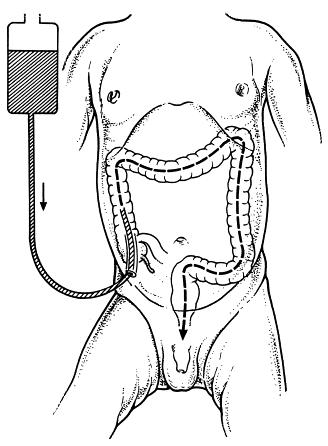
There are two possible procedures. One approach is to have two surgeries. During the initial surgery, a hollow needle is inserted through the skin into the epidural space, guided using fluoroscopy, a type of X-ray that allows the surgeon to see where the needle is in real time. Potential spots on the spinal cord are tested using a stimulator. A clinician will look to see if stimulation over those areas of the spinal cord leads to a desired response. Once found, the electrode array is properly positioned over the dura and the surgery is completed. This begins a trial period where the response to epidural stimulation is monitored. During this time the electrode array is attached to an electrical generator and power supply, which is worn on a belt outside of the body. When it is shown that things are working as desired, the generator is implanted underneath the skin in the abdomen or buttocks. The generator can be rechargeable or non-rechargeable. A remote control allows one to turn the generator on or off and control the frequency and intensity of stimulation.
The second method is to only have one surgery and no trial period. This is possible due to increased knowledge in how to stimulate the spinal cord. Soon after surgery, the individual will be taught how and when to use the epidural stimulation system at home. If needed, the frequency (how often) and intensity (how strong) of the stimulation will be adjusted at follow-up appointments with the physician. In other cases, many practice sessions of learning the right way to stimulate may be needed before a person can stimulate at home.
If the epidural stimulation is used for leg control, movement training, standing, and stepping will be required to learn how to coordinate and control movement during stimulation. This is required for the recovery of voluntary movements, standing and/or walking.
Epidural stimulation can be used in all people with SCI, regardless of the level or completeness of injury. However, certain situations can make it an unsafe treatment in some. It is important to speak to a health professional about your health history before beginning any new treatment.
Epidural stimulation should not be used in the following situations:
- By people with implanted medical devices like cardiac pacemakers
- By people who are unable to follow instructions or provide accurate feedback
- By people with an active infection
- By people with psychological or psychiatric conditions (e.g., depression, schizophrenia, substance abuse)
- By people who are unable to form clots (anticoagulopathy)
- Near areas of spinal stenosis (narrowing of the spinal canal)
Epidural stimulation should be used with caution in the following situations:
- By children or pregnant women
- By people who require frequent imaging tests like ultrasound or MRI (some epidural stimulation systems are compatible)
- By people using anticoagulant medications (blood thinners)
Epidural stimulation is generally well-tolerated, but there is a risk of experiencing negative effects.
The most common risks and side effects of epidural stimulation include:
- Technical difficulties with equipment, such as malfunction or shifting of the electrodes that may require surgery to fix
- Unpleasant sensations of jolting, tingling, burning, stinging, etc. (from improper remote settings)
Other less common risks and side effects of epidural stimulation include:
- Damage to the nervous system
- Leakage of cerebrospinal fluid
- Increased pain or discomfort
- Broken bones
- Masses/lumps growing around the site of the implanted electrode
Risks specific to the surgery which involves the removal of part of the vertebral bone (laminectomy) include:
- bleeding and/or infection at the surgical site
- spinal deformity and instability
Proper training on how to use the equipment and using the stimulation according to the directions of your health provider can help decrease the risks of experiencing these side effects.
 Neuromodulation methods to manage bladder function have usually involved stimulation of the sacral nerves (which are outside of the spinal cord), not with epidural spinal cord stimulation. This is reflected in the fact that almost no research exists regarding the effects of epidural stimulation on bowel and bladder function in the previous century.
Neuromodulation methods to manage bladder function have usually involved stimulation of the sacral nerves (which are outside of the spinal cord), not with epidural spinal cord stimulation. This is reflected in the fact that almost no research exists regarding the effects of epidural stimulation on bowel and bladder function in the previous century.
New information on epidural stimulation relating to bladder function is coming. In the last several years, several studies (weak evidence) from a very small group of participants of participants (who were AIS A or B) have found consistent improvements in bladder function. Participants in these reports were fitted with epidural stimulators for reactivation of paralyzed leg muscles for walking and reported additional benefits of improvements in bladder and/or bowel function. However, other studies have shown small changes to bladder function and no changes to bowel function. Negative changes, such as decreased control over the bladder, have even been noticed by some participants in another study. These findings suggest that epidural stimulation may improve quality of life by safely increasing the required time between catheterizations. Fewer catheterizations and reduced pressure in the bladder would preserve lower and upper urinary tract health. More research is required, especially with respect to bowel function. It must be noted that walk training alone has been shown to improve bladder and bowel function. Epidural stimulation may provide additional improvement to bladder function in comparison to walk training alone. Neuromodulation methods to manage bladder function have usually involved stimulation of the sacral nerves (which are outside of the spinal cord), not with epidural spinal cord stimulation. This is reflected in the fact that almost no research exists regarding the effects of epidural stimulation on bowel and bladder function in the previous century.
For more information, visit our pages on Bowel and Bladder Changes After SCI!
Why does walk/stand training alone have a beneficial effect on bladder, bowel, and sexual function?
Relationships between the leg movement and nerves in the low back regions have been identified.
Some evidence suggests that walk/step training alone can create improvements in bladder/bowel function. Researchers hypothesize that the sensory information created through walking or standing provides stimulation to the nerves in the low back region, which contains the nerves to stimulate bowel, bladder, and sexual function. Research has shown that bending and straightening the legs can be enhanced by how full the bladder is and the voiding of urine.
 One of the consequences of SCI is the loss of muscle mass below the injury and a tendency to accumulate fat inside the abdomen (abdominal fat or visceral fat) and under the skin (subcutaneous fat). These changes and lower physical activity after SCI increase the risk for several diseases.
One of the consequences of SCI is the loss of muscle mass below the injury and a tendency to accumulate fat inside the abdomen (abdominal fat or visceral fat) and under the skin (subcutaneous fat). These changes and lower physical activity after SCI increase the risk for several diseases.
A single (weak-evidence) study measured body composition in four young males with complete injuries. Participants underwent 80 sessions of stand and step training without epidural stimulation, followed by another 160 sessions of stand/step training with epidural stimulation. This involved one hour of standing and one hour of stepping five days a week. After all, training was complete, all four participants had a small reduction in their body fat, and all participants but one experienced an increase in their fat free body mass (i.e., the weight of their bones, muscles, organs, and water in the body) in comparison to their initial values prior to stimulation. While all participants experienced a reduction of fat, the amount of fat loss was minimal, ranging from 0.8 to 2.4 kg over a period of a year.
 The first use of epidural stimulation was as a treatment for chronic pain in the 1960s. Since then, it has been widely used for chronic pain management in persons without SCI. However, it is important to recognize that the chronic pain experienced by those without SCI is different from the chronic neuropathic pain experienced after SCI. This may explain, to some extent, why epidural stimulation has not been as successful in pain treatment for SCI. The mechanism by which electrical stimulation of the spinal cord can help with pain relief is unclear. Some research suggests that special nerve cells that block pain signals to the brain may be activated by epidural stimulation.
The first use of epidural stimulation was as a treatment for chronic pain in the 1960s. Since then, it has been widely used for chronic pain management in persons without SCI. However, it is important to recognize that the chronic pain experienced by those without SCI is different from the chronic neuropathic pain experienced after SCI. This may explain, to some extent, why epidural stimulation has not been as successful in pain treatment for SCI. The mechanism by which electrical stimulation of the spinal cord can help with pain relief is unclear. Some research suggests that special nerve cells that block pain signals to the brain may be activated by epidural stimulation.
There are a few studies focused on the role of epidural stimulation in managing pain after SCI. A number of other studies included a mix of different people with and without SCI. Because chronic neuropathic pain after SCI may not be the same as the chronic pain others experience, studies that do not separate mixed groups raise questions about the validity of findings. The number of individuals with SCI in these studies is often small, most were published in the 1980s and 1990s and so are quite dated, and the research is classified as weak evidence.
The results of this body of research show that some people may receive some pain reduction. Those who saw the most reduction in pain were individuals with an incomplete SCI. Also, satisfaction with pain reduction drops off over time. One study showed only 18% were satisfied 3 years after implantation. A different study looking at the long-term use of epidural stimulation for pain reduction found seven of nine individuals stopped using this method.
In the only recent study in this area, one woman with complete paraplegia (weak evidence) experienced a reduction in neuropathic pain frequency and intensity, and a reduction in average pain from 7 to 4 out of 10, with 0 being no pain and 10 being the worst imaginable pain. This improvement remained up to three months later after implantation of the epidural stimulation device.
It should be noted that the studies for pain place electrodes in different parts of the spinal cord compared to the more recent studies for voluntary movement, standing and stepping.
Refer to our article on Pain After SCI for more information!
 Using epidural stimulation to improve respiratory function is useful because it contracts the diaphragm and other muscles that help with breathing. Also, these muscles are stimulated in a way that imitates a natural pattern of breathing, reducing muscle fatigue. More common methods of improving respiratory function do not use epidural stimulation, but rather, directly stimulate the nerves that innervate the respiratory muscles. While such methods significantly improve quality of life and function in numerous ways, they are not without issues, including muscle fatigue from directly stimulating the nerves.
Using epidural stimulation to improve respiratory function is useful because it contracts the diaphragm and other muscles that help with breathing. Also, these muscles are stimulated in a way that imitates a natural pattern of breathing, reducing muscle fatigue. More common methods of improving respiratory function do not use epidural stimulation, but rather, directly stimulate the nerves that innervate the respiratory muscles. While such methods significantly improve quality of life and function in numerous ways, they are not without issues, including muscle fatigue from directly stimulating the nerves.
To date, most research into using epidural stimulation to improve respiratory function has been done in animals. Recently, research has been done in humans and weak evidence suggests that epidural stimulation may:
- help produce a cough strong enough to clear secretions independently.
- reduce frequency of respiratory tract infections.
- reduce the time required caregiver support.
- help individuals project their voice better and communicate more effectively.
Long term use of epidural stimulation shows that improvements remain over years and that minimal supervision is needed, making it suitable for use in the community.
Refer to our article on Respiratory Changes After SCI for more information!
![]()
The impact of epidural stimulation on sexual function has been a secondary focus in research studies looking at standing and walking. Currently, there are reports from one male and two females.
![]()
After a training program of walk training with epidural stimulation, one young adult male reported stronger, more frequent erections and the ability to reach full orgasm occasionally, which was not possible before epidural stimulation. However, this study looked at the effects of walk training and epidural stimulation together, which took place after several months of walk training without stimulation. Because the researchers did not describe what the individual’s sexual function was like after walk training, it is difficult to say how much benefit is attributed to epidural stimulation versus walk training.
 In another study with two middle-aged females 5-10 years post-injury, one reported no change in sexual function and the other reported the ability to experience orgasms with epidural stimulation, which was not possible since her injury.
In another study with two middle-aged females 5-10 years post-injury, one reported no change in sexual function and the other reported the ability to experience orgasms with epidural stimulation, which was not possible since her injury.
Refer to our article on Sexual Health After SCI for more information!
 Botulinum toxin (Botox) injections and surgically implanted intrathecal Baclofen pumps are the most common ways to manage spasticity. Baclofen pumps are not without issues, however. Many individuals do not qualify for this treatment if they have seizures or blood pressure instability, and pumps require regular refilling.
Botulinum toxin (Botox) injections and surgically implanted intrathecal Baclofen pumps are the most common ways to manage spasticity. Baclofen pumps are not without issues, however. Many individuals do not qualify for this treatment if they have seizures or blood pressure instability, and pumps require regular refilling.
Research in the 80s and 90s on the use of epidural stimulation for spasticity did not report very positive findings. It was noted that greater benefits were found in those with incomplete injury compared to those who were complete. Another paper concluded that (weak evidence) the beneficial effects of epidural stimulation on spasticity may subside for most users over a short period of time. This, combined with the potential for equipment failure and adverse events, suggested that epidural stimulation was not a feasible approach for ongoing management of spasticity.
More recently, positive results with epidural stimulation have been observed (weak evidence). This is likely due to improvements in technology, electrode placement, and stimulation parameters. Positive findings show that participants:
- reported fewer spasms over 2 years
- reported a reduction in severe spasms over 2 years
- reported a reduction in spasticity
- reported an improvement in spasticity over 1 year
- were able to stop or reduce the dose of antispastic medication
For more information, visit our page on Botulinum Toxin and Spasticity!
 In a study with a single participant (weak evidence) investigating walking, an individual implanted with an epidural stimulator also reported improvement in body temperature control, however details were not provided. More research is required to understand the role of epidural stimulation for temperature regulation.
In a study with a single participant (weak evidence) investigating walking, an individual implanted with an epidural stimulator also reported improvement in body temperature control, however details were not provided. More research is required to understand the role of epidural stimulation for temperature regulation.

 In severe SCI, individuals may suffer from chronic low blood pressure and orthostatic hypotension (fall in blood pressure when moving to more upright postures). These conditions can have significant effects on health and quality of life. Some recent studies have looked at how epidural stimulation affects cardiovascular function to improve orthostatic hypotension. Overall, they show (weak evidence) that epidural stimulation immediately increases blood pressure in individuals with low blood pressure while not affecting those who have normal blood pressure. They also showed that there is a training effect with repeated stimulation. This means that after consistently using stimulation for a while, normal blood pressure can occur even without stimulation when moving from lying to sitting.
In severe SCI, individuals may suffer from chronic low blood pressure and orthostatic hypotension (fall in blood pressure when moving to more upright postures). These conditions can have significant effects on health and quality of life. Some recent studies have looked at how epidural stimulation affects cardiovascular function to improve orthostatic hypotension. Overall, they show (weak evidence) that epidural stimulation immediately increases blood pressure in individuals with low blood pressure while not affecting those who have normal blood pressure. They also showed that there is a training effect with repeated stimulation. This means that after consistently using stimulation for a while, normal blood pressure can occur even without stimulation when moving from lying to sitting.
Moreover, researchers are starting to believe that changes in orthostatic hypotension and blood pressure can promote changes in the immune system (Bloom et al., 2020). In the body, the blood helps to circulate immune cells so they are able to fight infections in various areas. One case study found that after 97 sessions of epidural stimulation, the participant had fewer precursors for inflammation and more precursors for immune responses. Although these changes are exciting, researchers are still unsure why this happens, and whether these effects occur with all people who are implanted with an epidural stimulator.
Refer to our article on Orthostatic Hypotension for more information!
 For individuals with tetraplegia, even some recovery of hand function can mean a big improvement in quality of life. Research into using epidural stimulation to improve hand function consists of one case study (weak evidence) involving two young adult males who sustained motor complete cervical spinal cord injury over 18 months prior.
For individuals with tetraplegia, even some recovery of hand function can mean a big improvement in quality of life. Research into using epidural stimulation to improve hand function consists of one case study (weak evidence) involving two young adult males who sustained motor complete cervical spinal cord injury over 18 months prior.
The researchers reported improvements in voluntary movement and hand function with training while using epidural stimulation implanted in the neck. Training involved grasping and moving a handgrip while receiving stimulation. For 2 months, one man engaged in weekly sessions while the other trained daily for seven days. One participant was tested for a longer time as a permanent electrode was implanted, while the other participant only received a temporary implant. Both participants increased hand strength over the course of one session. Additional sessions brought additional gradual improvements in hand strength as well as hand control (i.e., the ability to move the hand precisely). These improvements carried over to everyday activities, such as feeding, bathing, dressing, grooming, transferring in and out of bed and moving in bed. Notably, these improvements were maintained when participants were not using epidural stimulation.
 Being able to control your trunk (or torso) is important for performing everyday activities such as picking things up or reaching for items. One study found that using epidural stimulation can increase the amount of distance you are able to lean forward. The improvement in forward reach occurred immediately when the stimulation was turned on. The two participants in this study were also able to reach more side to side as well, but the improvement was minor.
Being able to control your trunk (or torso) is important for performing everyday activities such as picking things up or reaching for items. One study found that using epidural stimulation can increase the amount of distance you are able to lean forward. The improvement in forward reach occurred immediately when the stimulation was turned on. The two participants in this study were also able to reach more side to side as well, but the improvement was minor.
Learning to make voluntary movements
Voluntary movements (i.e., being able to move your body when you want to) of affected limbs can occur with the use of epidural stimulation. Researchers are still unsure of the right training regimen to optimize results. For example, one study found that many sessions of step training with epidural stimulation are required for participants to slowly regain voluntary movement of the leg and foot with epidural stimulation when lying down. However, another study found that participants were able to voluntarily move their legs with stimulation and no stand training.
Voluntary movements (i.e., being able to move your body when you want to) of affected limbs can occur with the use of epidural stimulation. Researchers are still unsure of the right training regimen to optimize results. For example, one study found that many sessions of step and stand training with epidural stimulation are required for participants to slowly regain voluntary movement of the leg and foot with epidural stimulation when lying down. However, another study found that participants were able to voluntarily move their legs with stimulation and no stand training though the amount each participant was able to move their legs with epidural stimulation varied greatly. For example, one participant was able to voluntarily move their leg without any stimulation after over 500 hours of stand training with epidural stimulation while another participant from the same study was not able to voluntarily move their leg without stimulation after training. Overall, more than 25 people can move some or all of their leg joints voluntarily from the first time they receive epidural stimulation.
More recently, research shows that some with epidural stimulators can produce voluntary movements without stimulation on and without any intensive training program. In one study, participants did not do a consistent intensive training program, although many of them attended out-patient therapy or did therapy at home. Over the period of a year, 3 of 7 participants were able to voluntarily bend their knee, and bend and straighten their hips. Additionally, of those 3 participants, 2 were able to point their toes up and down. While the number of people able to make voluntary movements without stimulation is small, many more studies are underway.
Recent research indicates that epidural stimulation can influence walking function in individuals with limited or no motor function. While these findings are exciting, researchers are still learning how to use stimulation effectively to produce walking motions. Before being able to walk again, people must be able to make voluntary movements and be able to stand.
Learning to stand
 Some studies have also found that with extensive practice (e.g., 80 sessions), independent standing (i.e., standing without the help of another person, but holding onto a bar) may be achieved without epidural stimulation. Gaining the ability to stand may also occur with stand training combined with epidural stimulation. However, the findings with regard to the effect of stand training with epidural stimulation have been mixed. For example, one study showed that stand training for 5 days a week over a 4 month period with epidural stimulation resulted in independent standing for up to 10 minutes in an individual with a complete C7 injury, while another study has suggested that independent standing for 1.5 minutes can be achieved with epidural stimulation and 2 weeks of non-step specific training in an individual with complete T6 injury.
Some studies have also found that with extensive practice (e.g., 80 sessions), independent standing (i.e., standing without the help of another person, but holding onto a bar) may be achieved without epidural stimulation. Gaining the ability to stand may also occur with stand training combined with epidural stimulation. However, the findings with regard to the effect of stand training with epidural stimulation have been mixed. For example, one study showed that stand training for 5 days a week over a 4 month period with epidural stimulation resulted in independent standing for up to 10 minutes in an individual with a complete C7 injury, while another study has suggested that independent standing for 1.5 minutes can be achieved with epidural stimulation and 2 weeks of non-step specific training in an individual with complete T6 injury.
Learning to walk
 Earlier research has found that epidural stimulation can help with the development of walking-like movements, but these movements do not resemble “normal” walking. Instead, they resemble slight up and down movements of the leg. Recent studies have shown that with 10 months of practicing activities while lying down on the back and on the side, in addition to standing and stepping training, people are able to take a step without assistance from another person or body weight support. While some individuals in these studies have been able to regain some walking function, they are walking at a very slow pace, ranging from 0.19 meters per second to 0.22 meters per second. This is much slower than the 0.66 meters per second required for community walking. For example, of the 4 participants in one study, two were able to walk on the ground with a walker, one was only able to walk on a treadmill, and one was able to walk on the ground while holding the hands of another person. These differences in walking abilities gained by participants were not expected.
Earlier research has found that epidural stimulation can help with the development of walking-like movements, but these movements do not resemble “normal” walking. Instead, they resemble slight up and down movements of the leg. Recent studies have shown that with 10 months of practicing activities while lying down on the back and on the side, in addition to standing and stepping training, people are able to take a step without assistance from another person or body weight support. While some individuals in these studies have been able to regain some walking function, they are walking at a very slow pace, ranging from 0.19 meters per second to 0.22 meters per second. This is much slower than the 0.66 meters per second required for community walking. For example, of the 4 participants in one study, two were able to walk on the ground with a walker, one was only able to walk on a treadmill, and one was able to walk on the ground while holding the hands of another person. These differences in walking abilities gained by participants were not expected.
In late 2018, one researcher demonstrated that constant epidural stimulation was interfering with proprioception, or the body’s ability to know where your limbs are in space, which ultimately hinders the walking relearning process. The solution to this problem involves activating the stimulation in a specific sequence, rather than having it continuously on. With this method and a year’s worth of training, participants were able to begin walking with an assistive device (such as a walker or poles) without stimulation. However, these individuals had to intensively practice standing and walking with stimulation for many months to produce these results. In these studies, one case of injury was reported where a participant sustained a hip fracture during walking with a body weight support. Further studies on how to individualize therapy will be necessary as the response to treatment in these studies varied greatly from person to person depending on the frequency and intensity of the stimulation.
Most of the stand/walk training conducted in the studies is with the use of a body weight support treadmill.Is it the training or the epidural stimulation?
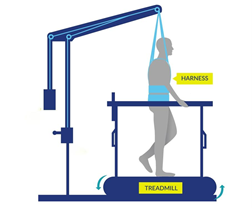
Arm and leg movement and blood pressure have been seen to improve with epidural stimulation, but the role of rehabilitation in these recoveries is unclear. Rehabilitation techniques can have an effect on regaining motor function. For example, step/walk training alone can help improve the ability to make voluntary movements, walking and blood pressure among individuals with incomplete injuries. In much of the current research, epidural stimulation is paired with extensive training (typically around 80 sessions) before and after the epidural stimulator is implanted. Furthermore, these studies do not compare the effects of epidural stimulation to a control group who receives a fake stimulation (a placebo) which would help to see if stimulation truly has an effect. Without this comparison, we are unable to clearly understand the extent of recovery that is attributable to epidural stimulation versus the effects of training. However, evidence now shows that voluntary movement and cardiovascular function can be improved from the first time epidural stimulation is used, if the stimulation parameters are specific for the function and person, which supports the role of epidural stimulation in improving function.
Access to new medical treatment for those requiring it cannot come soon enough. Experimental therapies are typically expensive and not covered by health care. Rigorous and sufficient testing is required before treatments become standard practice and receive health care coverage. Epidural stimulation for improving function in SCI is a unique example because epidural stimulation technology has been used widely to treat intractable back pain in individuals without SCI. The benefit of this is that, if/when epidural stimulation for individuals with SCI is shown to be safe and effective, the move from experimental clinical practice could happen relatively quickly as a number of hurdles from regulatory bodies have already been overcome. That said, current barriers to accessing epidural stimulation noted in a survey study of doctors include a lack of strong evidence research showing benefits, a lack of guidelines for the right stimulation settings, and an inability to determine who will benefit from it.
 In Canada, the cost for an institution to install an epidural stimulation system for back pain in those without spinal cord injury, which is a common procedure, was $21,595 CAD. The cost incurred by a Canadian citizen undergoing implantation in Canada is $0 as it is covered by publicly funded health care.
In Canada, the cost for an institution to install an epidural stimulation system for back pain in those without spinal cord injury, which is a common procedure, was $21,595 CAD. The cost incurred by a Canadian citizen undergoing implantation in Canada is $0 as it is covered by publicly funded health care.
In the United States, the cost for an institution to install an epidural stimulation system for back pain in those without spinal cord injury ranged between $32,882 USD (Medicare) and $57,896 USD (Blue Cross Blue Shield). The cost incurred for American citizens in the US will vary widely depending on their insurance coverage.
In contrast, for individuals with SCI, an epidural stimulation system is reported to cost over $100,000 USD in Thailand, and higher in other countries. Prospective clients should be aware that the epidural stimulation offered by these clinics may not be the same as that in the research reported in this article.
The recommended course for those wishing to try epidural stimulation is to register in a clinical trial. Regardless, persons interested in pursuing surgery at a private clinic or registering for clinical trials will find it useful to refer to the clinical trial guidelines published by ICORD (https://icord.org/research/iccp-clinical-trials-information/) for information on what they should be aware of when considering having an epidural stimulator implanted. Research studies that involve epidural stimulation can be found by searching the clinicaltrials.gov database.
Overall, there is evidence that epidural stimulation can improve function and health after SCI in numerous ways. However, because of the invasive nature of epidural stimulator implantation, research in this area involves few participants, no control groups, and no randomization, so it is classified as weak evidence. It is therefore important to keep in mind that while these recent reports are encouraging, more rigorous studies with more participants are needed to confirm the benefits and risks of this treatment to determine its place in SCI symptom management.
Epidural stimulation is not “plug and play” technology. Each implanted device needs to be tailored to the spine of the recipient. Some individuals respond to certain stimulation settings while others may respond better to other settings. Furthermore, over time, the need to change stimulation settings or even reposition the implant to maintain effectiveness may be required. Extensive physical training appears to be required for epidural stimulation to be most effective in improving standing or walking. The additional benefit of epidural stimulation to walk training is not always clear from the literature.
For a review of how we assess evidence at SCIRE Community and advice on making decisions, please see SCIRE Community Evidence.
Parts of this page have been adapted from the SCIRE Project (Professional) “Spasticity”, “Bladder Management”, and “Pain Management” chapters:
Hsieh JTC, Connolly SJ, McIntyre A, Townson AF, Short C, Mills P, Vu V, Benton B, Wolfe DL (2016). Spasticity Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Curt A, Mehta S, Sakakibara BM, editors. Spinal Cord Injury Rehabilitation Evidence. Version 6.0.
Available from: scireproject.com/evidence/rehabilitation-evidence/spasticity/
Hsieh J, McIntyre A, Iruthayarajah J, Loh E, Ethans K, Mehta S, Wolfe D, Teasell R. (2014). Bladder Management Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors. Spinal Cord Injury Rehabilitation Evidence. Version 5.0: p 1-196.
Available from: scireproject.com/evidence/rehabilitation-evidence/bladder-management/
Mehta S, Teasell RW, Loh E, Short C, Wolfe DL, Benton B, Hsieh JTC (2016). Pain Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Loh E, McIntyre A, Querée M, editors. Spinal Cord Injury Rehabilitation Evidence. Version 6.0: p 1-92.
Available from: scireproject.com/evidence/rehabilitation-evidence/pain-management/
Evidence for “What is epidural stimulation” is based on the following studies:
International Neuromodulation Society. (2010). Neuromodulation: An Emerging Field.
Toossi, A., Everaert, D. G., Azar, A., Dennison, C. R., & Mushahwar, V. K. (2017). Mechanically Stable Intraspinal Microstimulation Implants for Human Translation. Annals of Biomedical Engineering, 45(3), 681–694. Retrieved from http://link.springer.com/10.1007/s10439-016-1709-0
Evidence for “How does epidural stimulation work?” is based on the following studies:
Evidence for “How are epidural stimulation electrodes implanted?” is based on the following studies:
Lu, D. C., Edgerton, V. R., Modaber, M., AuYong, N., Morikawa, E., Zdunowski, S., … Gerasimenko, Y. (2016a). Engaging Cervical Spinal Cord Networks to Reenable Volitional Control of Hand Function in Tetraplegic Patients. Neurorehabilitation & Neural Repair, 30(10), 951–962. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/27198185
Lu, D. C., Edgerton, V. R., Modaber, M., AuYong, N., Morikawa, E., Zdunowski, S., … Gerasimenko, Y. (2016b). Engaging Cervical Spinal Cord Networks to Reenable Volitional Control of Hand Function in Tetraplegic Patients. Neurorehabilitation & Neural Repair, 30(10), 951–962.
Evidence for “Are there restrictions or precautions for using epidural stimulation?” is based on the following studies:
Moore, D. M., & McCrory, C. (2016). Spinal cord stimulation. BJA Education, 16(8), 258–263. Retrieved from https://linkinghub.elsevier.com/retrieve/pii/S2058534917300975
Wolter, T. (2014). Spinal cord stimulation for neuropathic pain: current perspectives. Journal of Pain Research, 7, 651–663.
Evidence for “Are there risks and side effects of epidural stimulation?” is based on the following studies:
Eldabe, S., Buchser, E., & Duarte, R. V. (2015). Complications of Spinal Cord Stimulation and Peripheral Nerve Stimulation Techniques: A Review of the Literature. Pain Medicine, 17(2), pnv025. Retrieved from https://academic.oup.com/painmedicine/article-lookup/doi/10.1093/pm/pnv025
Taccola, G., Barber, S., Horner, P. J., Bazo, H. A. C., & Sayenko, D. (2020). Complications of epidural spinal stimulation: lessons from the past and alternatives for the future. Spinal Cord, 58(10), 1049–1059. Retrieved from http://dx.doi.org/10.1038/s41393-020-0505-8
Evidence for “Epidural stimulation and bladder and bowel function” is based on the following studies:
Herrity, A. N., Williams, C. S., Angeli, C. A., Harkema, S. J., & Hubscher, C. H. (2018). Lumbosacral spinal cord epidural stimulation improves voiding function after human spinal cord injury. Scientific Reports, 8(1), 1–11. Retrieved from http://dx.doi.org/10.1038/s41598-018-26602-2
Herrity, April N., Aslan, S. C., Ugiliweneza, B., Mohamed, A. Z., Hubscher, C. H., & Harkema, S. J. (2021). Improvements in Bladder Function Following Activity-Based Recovery Training With Epidural Stimulation After Chronic Spinal Cord Injury. Frontiers in Systems Neuroscience, 14(January), 1–14.
Hubscher, C. H., Herrity, A. N., Williams, C. S., Montgomery, L. R., Willhite, A. M., Angeli, C. A., & Harkema, S. J. (2018). Improvements in bladder, bowel and sexual outcomes following task-specific locomotor training in human spinal cord injury. Plos One, 1–26.
Darrow, D., Balser, D., Netoff, T. I., Krassioukov, A., Phillips, A., Parr, A., & Samadani, U. (2019). Epidural Spinal Cord Stimulation Facilitates Immediate Restoration of Dormant Motor and Autonomic Supraspinal Pathways after Chronic Neurologically Complete Spinal Cord Injury. Journal of Neurotrauma, 2336, neu.2018.6006. Retrieved from https://www.liebertpub.com/doi/10.1089/neu.2018.6006
Beck, L., Veith, D., Linde, M., Gill, M., Calvert, J., Grahn, P., … Zhao, K. (2020). Impact of long-term epidural electrical stimulation enabled task-specific training on secondary conditions of chronic paraplegia in two humans. Journal of Spinal Cord Medicine, 0(0), 1–6. Retrieved from https://doi.org/10.1080/10790268.2020.1739894
Evidence for “Epidural stimulation and body composition” is based on the following studies:
Terson de Paleville, D. G. L., Harkema, S. J., & Angeli, C. A. (2019). Epidural stimulation with locomotor training improves body composition in individuals with cervical or upper thoracic motor complete spinal cord injury: A series of case studies. The Journal of Spinal Cord Medicine, 42(1), 32–38.
Evidence for “Epidural stimulation and pain” is based on the following studies:
Guan, Y. (2012). Spinal cord stimulation: neurophysiological and neurochemical mechanisms of action. Current Pain and Headache Reports, 16(3), 217–225.
Marchand, S. (2015). Spinal cord stimulation analgesia. PAIN, 156(3), 364–365.
Tasker, R. R., DeCarvalho, G. T., & Dolan, E. J. (1992). Intractable pain of spinal cord origin: clinical features and implications for surgery. Journal of Neurosurgery.
Cioni, B., Meglio, M., Pentimalli, L., & Visocchi, M. (1995). Spinal cord stimulation in the treatment of paraplegic pain. Journal of Neurosurgery, 82(1), 35–39.
Warms, C. A., Turner, J. A., Marshall, H. M., & Cardenas, D. D. (2002). Treatments for chronic pain associated with spinal cord injuries: many are tried, few are helpful. Clinical Journal of Pain, 18(3), 154–163.
Reck, T. A., & Landmann, G. (2017). Successful spinal cord stimulation for neuropathic below-level spinal cord injury pain following complete paraplegia: a case report. Spinal Cord Series and Cases, 3, 17049.
Evidence for “Epidural stimulation and respiratory function” is based on the following studies:
Hachmann, J. T., Grahn, P. J., Calvert, J. S., Drubach, D. I., Lee, K. H., & Lavrov, I. A. (2017). Electrical Neuromodulation of the Respiratory System After Spinal Cord Injury. Mayo Clinic Proceedings, 92(9), 1401–1414. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/28781176
DiMarco, A. F., Kowalski, K. E., Geertman, R. T., & Hromyak, D. R. (2006). Spinal cord stimulation: a new method to produce an effective cough in patients with spinal cord injury. American Journal of Respiratory and Critical Care Medicine, 173(12), 1386–1389.
DiMarco, A. F., Kowalski, K. E., Geertman, R. T., & Hromyak, D. R. (2009). Lower thoracic spinal cord stimulation to restore cough in patients with spinal cord injury: results of a National Institutes of Health-sponsored clinical trial. Part I: methodology and effectiveness of expiratory muscle activation. Archives of Physical Medicine & Rehabilitation, 90(5), 717–725.
Harkema, S. J., Wang, S., Angeli, C. A., Chen, Y., Boakye, M., Ugiliweneza, B., & Hirsch, G. A. (2018). Normalization of Blood Pressure With Spinal Cord Epidural Stimulation After Severe Spinal Cord Injury. Frontiers in Human Neuroscience, 12, 83.
DiMarco, A. F., Kowalski, K. E., Hromyak, D. R., & Geertman, R. T. (2014). Long-term follow-up of spinal cord stimulation to restore cough in subjects with spinal cord injury. The Journal of Spinal Cord Medicine, 37(4), 380–388.
Evidence for “Epidural stimulation and sexual function” is based on the following studies:
Harkema, S., Gerasimenko, Y., Hodes, J., Burdick, J., Angeli, C., Chen, Y., … Edgerton, V. R. (2011). Effect of epidural stimulation of the lumbosacral spinal cord on voluntary movement, standing, and assisted stepping after motor complete paraplegia: A case study. The Lancet, 377(9781), 1938–1947.
Darrow, D., Balser, D., Netoff, T. I., Krassioukov, A., Phillips, A., Parr, A., & Samadani, U. (2019). Epidural Spinal Cord Stimulation Facilitates Immediate Restoration of Dormant Motor and Autonomic Supraspinal Pathways after Chronic Neurologically Complete Spinal Cord Injury. Journal of Neurotrauma, 2336, neu.2018.6006. Retrieved from https://www.liebertpub.com/doi/10.1089/neu.2018.600
Evidence for “Epidural stimulation and spasticity” is based on the following studies:
Nagel, S. J., Wilson, S., Johnson, M. D., Machado, A., Frizon, L., Chardon, M. K., … Howard, M. A. 3rd. (2017). Spinal Cord Stimulation for Spasticity: Historical Approaches, Current Status, and Future Directions. Neuromodulation: Journal of the International Neuromodulation Society, 20(4), 307–321.
Dekopov, A. V., Shabalov, V. A., Tomsky, A. A., Hit, M. V., & Salova, E. M. (2015). Chronic spinal cord stimulation in the treatment of cerebral and spinal spasticity. Stereotactic and Functional Neurosurgery.
Dimitrijevic, M. R., Illis, L. S., Nakajima, K., Sharkey, P. C., & Sherwood, A. M. (1986). Spinal cord stimulation for the control of spasticity in patients with chronic spinal cord injury: II. Neurophysiologic observations. Central Nervous System Trauma, 3(2), 145–152. Retrieved from http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=med2&AN=3490313
Midha, M., & Schmitt, J. K. (1998). Epidural spinal cord stimulation for the control of spasticity in spinal cord injury patients lacks long-term efficacy and is not cost-effective. Spinal Cord, 36(3), 190–192. Retrieved from https://www.nature.com/articles/3100532
Barolat, G., Singh-Sahni, K., Staas, W. E. J., Shatin, D., Ketcik, B., & Allen, K. (1995). Epidural spinal cord stimulation in the management of spasms in spinal cord injury: a prospective study. Stereotactic & Functional Neurosurgery, 64(3), 153–164.
Dekopov, A. V., Shabalov, V. A., Tomsky, A. A., Hit, M. V., & Salova, E. M. (2015). Chronic spinal cord stimulation in the treatment of cerebral and spinal spasticity. Stereotactic and Functional Neurosurgery.
Pinter, M. M., Gerstenbrand, F., & Dimitrijevic, M. R. (2000). Epidural electrical stimulation of posterior structures of the human lumbosacral cord: 3. Control Of spasticity. Spinal Cord, 38(9), 524–531. Retrieved from https://www.nature.com/articles/3101040
Evidence for “Epidural stimulation and temperature regulation” is based on the following studies:
Edgerton, V. R., & Harkema, S. (2011). Epidural stimulation of the spinal cord in spinal cord injury: current status and future challenges. Expert Review of Neurotherapeutics, 11(10), 1351–1353. Retrieved from http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=med7&AN=21955190
Harkema, S. J., Gerasimenko, Y., Hodes, J., Burdick, J., Angeli, C., Chen, Y., … Edgerton, V. R. (2011). Supplementary index: Effect of epidural stimulation of the lumbosacral spinal cord on voluntary movement, standing, and assisted stepping after motor complete paraplegia: A case study. The Lancet, 377(9781), 1938–1947. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/21601270
Evidence for “Epidural stimulation and cardiovascular function” is based on the following studies:
Bloom, O., Wecht, J. M., Legg Ditterline, B. E., Wang, S., Ovechkin, A. V., Angeli, C. A., … Harkema, S. J. (2020). Prolonged Targeted Cardiovascular Epidural Stimulation Improves Immunological Molecular Profile: A Case Report in Chronic Severe Spinal Cord Injury. Frontiers in Systems Neuroscience, 14(October), 1–11.
Evidence for “Epidural stimulation and hand function” is based on the following study:
Lu, D. C., Edgerton, V. R., Modaber, M., AuYong, N., Morikawa, E., Zdunowski, S., … Gerasimenko, Y. (2016a). Engaging Cervical Spinal Cord Networks to Reenable Volitional Control of Hand Function in Tetraplegic Patients. Neurorehabilitation & Neural Repair, 30(10), 951–962. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/27198185
Evidence for “Epidural stimulation and movement: trunk control” is based on the following studies:
Evidence for “Epidural stimulation and movement: voluntary movements” is based on the following studies:
Rejc, E., Angeli, C. A., Bryant, N., & Harkema, S. J. (2017). Effects of Stand and Step Training with Epidural Stimulation on Motor Function for Standing in Chronic Complete Paraplegics. Journal of Neurotrauma, 34, 1787–18023. Retrieved from www.liebertpub.com
Angeli, C. A., Edgerton, V. R., Gerasimenko, Y. P., & Harkema, S. J. (2014). Altering spinal cord excitability enables voluntary movements after chronic complete paralysis in humans. Brain, 137(Pt 5), 1394–1409. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3999714/
Peña Pino, I., Hoover, C., Venkatesh, S., Ahmadi, A., Sturtevant, D., Patrick, N., Freeman, D., Parr, A., Samadani, U., Balser, D., Krassioukov, A., Phillips, A., Netoff, T. I., & Darrow, D. (2020). Long-Term Spinal Cord Stimulation After Chronic Complete Spinal Cord Injury Enables Volitional Movement in the Absence of Stimulation. Frontiers in systems neuroscience, 14, 35. https://doi.org/10.3389/fnsys.2020.00035
Evidence for “Epidural stimulation and movement: walking and standing” is based on the following studies:
Grahn, P. J., Lavrov, I. A., Sayenko, D. G., Straaten, M. G. Van, Gill, M. L., Strommen, J. A., … Lee, K. H. (2017). Enabling Task-Specific Volitional Motor Functions via Spinal Cord Neuromodulation in a Human with Paraplegia. Mayo Clinic Proceedings, 92(4), 544–554. Retrieved from http://dx.doi.org/10.1016/j.mayocp.2017.02.014
Harkema, S. J., Gerasimenko, Y., Hodes, J., Burdick, J., Angeli, C., Chen, Y., … Edgerton, V. R. (2011). Supplementary index: Effect of epidural stimulation of the lumbosacral spinal cord on voluntary movement, standing, and assisted stepping after motor complete paraplegia: A case study. The Lancet, 377(9781), 1938–1947. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/21601270
Rejc, E., Angeli, C. A., Atkinson, D., & Harkema, S. J. (2017). Motor recovery after activity-based training with spinal cord epidural stimulation in a chronic motor complete paraplegic. Scientific Reports, 7(1), 13476. Retrieved from www.nature.com/scientificreports
Rejc, E., Angeli, C., & Harkema, S. (2015). Effects of Lumbosacral Spinal Cord Epidural Stimulation for Standing after Chronic Complete Paralysis in Humans. PLoS ONE [Electronic Resource], 10(7), e0133998. Retrieved from http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=med8&AN=26207623
Grahn, P. J., Lavrov, I. A., Sayenko, D. G., Straaten, M. G. Van, Gill, M. L., Strommen, J. A., … Lee, K. H. (2017). Enabling Task-Specific Volitional Motor Functions via Spinal Cord Neuromodulation in a Human with Paraplegia. Mayo Clinic Proceedings, 92(4), 544–554. Retrieved from http://dx.doi.org/10.1016/j.mayocp.2017.02.014
Gill, M. L., Grahn, P. J., Calvert, J. S., Linde, M. B., Lavrov, I. A., Strommen, J. A., … Zhao, K. D. (2018). Neuromodulation of lumbosacral spinal networks enables independent stepping after complete paraplegia. Nature Medicine, 24(11), 1677–1682. Retrieved from https://doi.org/10.1038/s41591-018-0175-7
Angeli, C. A., Boakye, M., Morton, R. A., Vogt, J., Benton, K., Chen, Y., … Harkema, S. J. (2018). Recovery of Over-Ground Walking after Chronic Motor Complete Spinal Cord Injury. New England Journal of Medicine, 379(13), 1244–1250. Retrieved from http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=medl&AN=30247091
van de Port, I. G., Kwakkel, G., & Lindeman, E. (2008). Community ambulation in patients with chronic stroke: How is it related to gait speed? Journal of Rehabilitation Medicine, 40(1), 23–27.
Wagner, F. B., Mignardot, J.-B., Le Goff-Mignardot, C. G., Demesmaeker, R., Komi, S., Capogrosso, M., … Courtine, G. (2018). Targeted neurotechnology restores walking in humans with spinal cord injury. Nature, 563(7729), 65–71. Retrieved from http://www.nature.com/articles/s41586-018-0649-2
Angeli, C. A., Edgerton, V. R., Gerasimenko, Y. P., & Harkema, S. J. (2014). Altering spinal cord excitability enables voluntary movements after chronic complete paralysis in humans. Brain, 137(Pt 5), 1394–1409. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3999714/
Carhart, M. R., He, J., Herman, R., D’Luzansky, S., & Willis, W. T. (2004). Epidural spinal-cord stimulation facilitates recovery of functional walking following incomplete spinal-cord injury. IEEE Transactions on Neural Systems & Rehabilitation Engineering, 12(1), 32–42. Retrieved from http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=med5&AN=15068185
Harkema, S. J., Wang, S., Angeli, C. A., Chen, Y., Boakye, M., Ugiliweneza, B., & Hirsch, G. A. (2018). Normalization of Blood Pressure With Spinal Cord Epidural Stimulation After Severe Spinal Cord Injury. Frontiers in Human Neuroscience, 12, 83.
Legg Ditterline, B. E., Aslan, S. C., Wang, S., Ugiliweneza, B., Hirsch, G. A., Wecht, J. M., & Harkema, S. (2020). Restoration of autonomic cardiovascular regulation in spinal cord injury with epidural stimulation: a case series. Clinical Autonomic Research, (0123456789), 2–5. Retrieved from https://doi.org/10.1007/s10286-020-00693-2
Evidence for “Costs and availability of epidural stimulation” is based on the following studies:
Solinsky, R., Specker-Sullivan, L., & Wexler, A. (2020). Current barriers and ethical considerations for clinical implementation of epidural stimulation for functional improvement after spinal cord injury. Journal of Spinal Cord Medicine, 43(5), 653–656.
Kumar, K., & Bishop, S. (2009). Financial impact of spinal cord stimulation on the healthcare budget: a comparative analysis of costs in Canada and the United States. Journal of Neurosurgery: Spine.
Image credits
- Image by SCIRE Community Team
- Image by SCIRE Community Team
- Image by SCIRE Community Team
- Image by SCIRE Community Team
- Adapted from image made by Mysid Inkscape, based on plate 770 from Gray’s Anatomy (1918, public domain).
- Pregnant woman holding tummy. [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)] via Google Images.
- Edited from Nervous system, Musculature. ©Servier Medical Art. CC BY 3.0.
- Neurons ©NIH Image Gallery. CC BY-NC 2.0.
- Image by SCIRE Community
- bladder by fauzan akbar from the Noun Project
- Large Intestine by BomSymbols from the Noun Project
- Feet by Matt Brooks from the Noun Project
- hip by priyanka from the Noun Project
- visceral fat by Olena Panasovska from the Noun Project
- Lightning by FLPLF from the Noun Project
- Lungs by dDara from the Noun Project
- Love by Jake Dunham from the Noun Project
- Male by Centis MENANT from the Noun Project
- Female by Centis MENANT from the Noun Project
- Image by SCIRE Community
- Temperature by Adrien Coquet from the Noun Project
- Heart by Nick Bluth from the Noun Project
- Image by SCIRE Community
- Hand by Sergey Demushkin from the Noun Project
- Torso by Ronald Vermeijs from the Noun Project
- Yoga posture by Gan Khoon Lay from the Noun Project
- Standing by Rafo Barbosa from the Noun Project
- Walking by Samy Menai from the Noun Project
- Image by SCIRE Community
- Canada by Yohann Berger from the Noun Project
- United States of America by Yohann Berger from the Noun Project
Authors: Sharon Jang, Vanessa Mok, Dominik Zbogar | Reviewer: Phillip Popovich | Published: 5 May 2020 | Updated: ~
The gut microbiome, also known as gut flora or gut microbiota, refers to the organisms that live in our digestive system. Research suggests that changes to the gut microbiome can affect the development of long-term complications and recovery following spinal cord injury (SCI).
Key Points
- The microbiome is a community of organisms in the gut that contribute to the body’s day-to-day functions
- Factors such as diet, medications, physical activity, sleep, smoking, and stress have been shown to affect the balance of the gut microbiome in the general population.
- After SCI, the gut microbiome experiences unique challenges and changes. The implications of these changes are poorly understood.
- Currently, very few studies exist regarding the gut microbiome in people with SCI.
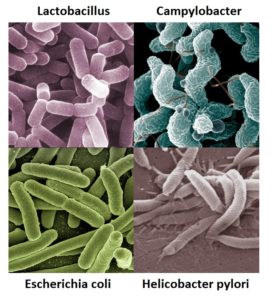
Examples of bacteria that can be found in the digestive system.1-4
The microbiome refers to the trillions of viruses, fungi, and bacteria living all over the body. Although you may see the terms “microbiota” and “microbiome” sometimes used interchangeably, the microbiome technically refers to the genetic makeup (i.e. the DNA) of these organisms, while the microbiota refers to the organisms themselves. The core microbiota in humans is similar between people, however each of us has their own distinct variation of bacteria, viruses, and fungi that comprises their microbiota. These organisms exist in many areas of the body, including on the skin, in the nose, in the vagina, and in the bladder. However, microbiota have the highest density and variation in the large intestine.
Our past view of microbiota was focused on their potential to cause infection. However, more recent research has shown that microbiota play a substantial role in normal development and daily body functions. The greater the diversity or variation of the microbiota, the healthier and more resilient it is. The opposite has been associated with negative long-term effects on diseases later in life. Although research on the microbiome is still emerging, researchers have discovered that the microbiome is responsible for:
- Preventing the growth of other harmful organisms
- Stimulating the immune system to help fight off infections
- Preventing the development of allergies
- Food digestion and nutrient absorption
- Sugar and fat metabolism
- Brain development
- Drug metabolism
In recent years, the microbiome has gained a lot of interest in research. This is partly due to new technology which allow scientists to observe the DNA of bacteria, resulting in a more specific analysis. Bacteria is primarily prevalent in the intestines, and amount to 10 times more than all the cells in the human body. This adds up to 1-3% of body mass, or 2-6 lbs of your weight. This article will focus on the gut microbiota, specifically the bacterial component of the microbiota, as most of the research on the microbiome thus far has focused on bacteria rather than fungi and viruses.
Development of the gut microbiome
|
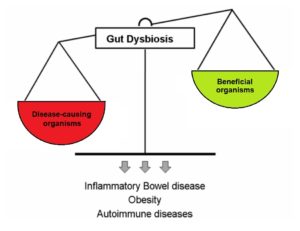
Dysbiosis occurs when disease-causing organisms become more dominant than beneficial organisms.6
The microbiota is comprised of both good and bad bacteria, as well as bacteria that may be good or bad depending on the environment and circumstances. When your body is healthy, the good bacteria are able to keep pathogens in check, thus preventing illness. However, there are certain situations when disease-causing organisms become more prevalent than the beneficial bacteria. Known as dysbiosis, this state in which the microbiota is not in balance may be caused by stress, antibiotic use, and dysfunction of the intestines. Traumatic SCI can cause neurological and psychological complications which require care that may predispose these individuals to dysbiosis. These include:
- Psychological stress after injury and during adaptation
- Having a neurogenic bowel/bladder
- A weakened immune system, which creates a greater need for antibiotics
Dysbiosis can also lead to short-term negative effects such as food intolerances, stomach upset, and an increased risk of developing infections. It is also linked to chronic conditions such as:
- Allergies
- Psychiatric conditions (e.g. depression, anxiety)
- Autoimmune diseases (e.g. rheumatoid arthritis, Crohn’s disease, inflammatory bowel disease)
- Metabolic disorders (e.g. obesity, diabetes)
- Neurologic conditions (e.g. pain, Alzheimer’s, neurogenic bowel dysfunction)
- Non-alcoholic fatty liver disease
Many of these conditions are already common in people living with SCI. Hence, a healthy microbiome may be important in maintaining the regular functions of the microbiome and preventing the consequences of dysbiosis following SCI.
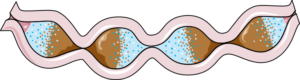
Movement of the gut slows as a consequence of neurogenic bowel, which is a common in SCI, especially with higher levels of injury.7
After SCI, one of the main group of nerves that innervates the gut, the sympathetic nervous system, becomes impaired. This can impact the gut microbiota in 3 ways: through slowing gut movement, through modifying the ability for microbiota to thrive, and through modifying the immune system in the gut. The slower movement of the gut contents, one of the results of impaired bowel function (known as neurogenic bowel dysfunction) after SCI, can impact the microbiota at the far end of the intestines by delaying the delivery of important nutrients. This is of concern because bacteria in the gut thrive by fermenting or breaking down foods such as starches and fibre, and produce metabolites such as butyrate. One study with weak evidence found that people with chronic (at least 12 months post-injury) complete SCI had significant decreases in butyrate-producing bacteria compared to the non-SCI population. As butyrate has anti-inflammatory effects on the nervous system, researchers believe that low butyrate levels can negatively affect long-term recovery following SCI due to increased inflammation.

Millions of bacteria grow on the mucus in the gut, forming a biofilm.8
Secondly, the sympathetic nervous system is responsible for stimulating mucus secretion within the gut. With a lack of input from the sympathetic nervous system, the production of mucus is decreased. This has important implications for the microbiota in the intestines, as mucus acts as a surface that allows for bacteria to bind to it, thus creating a biofilm. A biofilm is a group of bacteria that has formed a structured community on a surface. With a reduced amount of area for bacteria to thrive, the types of bacteria living in the gut may be altered.
Thirdly, the gut has a protective barrier to prevent bad bacteria from entering the body through the intestinal walls. This immune system within the gut is known as the gastrointestinal-associated lymphoid tissue (GALT) and is controlled by the sympathetic nervous system. With a lack of signaling from the sympathetic nervous system, functioning of the GALT may become compromised. In addition, chronic stress or trauma (which can be brought on by SCI) may change the permeability of the wall of the intestine, allowing harmful bacteria into the body. This may be a potential source of inflammation following SCI and may partly explain why people with SCI are more prone to long-term complications. While research with SCI rat models shows this compromise of the protective barrier and movement of bacteria into places it does not usually reside, (like the blood), it is not yet known if the same is true for humans.
Individuals with SCI are found to have different bacteria comprising their microbiota, compared to able-bodied individuals. For example, one study (weak evidence) found that the diversity of gut bacteria and number of overall bacteria of individuals with chronic tetraplegia were less than in able-bodied individuals. Conversely, another study found individuals with SCI to harbour greater bacterial diversity in their gut relative to people without SCI. However, the greater variation of bacteria in people with SCI consist of bacteria less commonly found in able-bodied individuals. The implications of these differences are unknown and have yet to be researched.
 Comparing gut bacteria between different populationsDifferences in bacterial composition have been noted in people with other health conditions (such as schizophrenia and diabetes), but whether these differences contributed to the progression of the disease or arose due to the condition is unclear. Also, differences between countries exist and may be attributed to differences in environmental conditions (e.g. diet, lifestyle). However, impacts of these alterations are largely unknown. |
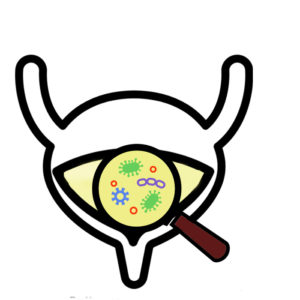 Previously, it was thought that urine was clean and sterile – that urine should be free from bacteria and white blood cells, which are both signs of infection. In recent years, researchers have discovered that healthy urine is not always sterile. In a conditioned called asymptomatic bacteriuria, non-harmful bacteria are found in the urine, but the individual does not experience any symptoms of a urinary tract infection (UTI) or other illness. Although certain strains of bacteria in urine may be healthy, after SCI, the proportion and composition of bacteria found in urine changes. One (weak evidence) study suggests that individuals with SCI and neurogenic bladders have microbiomes with more unhealthy bacteria, which may be a precursor for UTIs.
Previously, it was thought that urine was clean and sterile – that urine should be free from bacteria and white blood cells, which are both signs of infection. In recent years, researchers have discovered that healthy urine is not always sterile. In a conditioned called asymptomatic bacteriuria, non-harmful bacteria are found in the urine, but the individual does not experience any symptoms of a urinary tract infection (UTI) or other illness. Although certain strains of bacteria in urine may be healthy, after SCI, the proportion and composition of bacteria found in urine changes. One (weak evidence) study suggests that individuals with SCI and neurogenic bladders have microbiomes with more unhealthy bacteria, which may be a precursor for UTIs.
With the knowledge that pre-existing bacteria live in the bladder, some researchers have questioned whether it would be possible to modify the microbiota to prevent UTIs. Bacterial interference is a process whereby non-harmful bacteria are injected into the bladder. Ideally, the benign bacteria prevent the growth of harmful bacteria by creating competition for nutrients and space to colonize. Multiple studies (weak evidence) indicate bacterial interference may decrease the occurrence of UTIs in individuals with SCI, and may delay the recurrence of UTIs. However, there are barriers to using bacterial interference, including:
- The process of injecting bacteria into the bladder, which is a cumbersome process that requires multiple administrations over consecutive days.
- The maintenance of the injected bacteria, which may not successfully colonize the bladder.
Given these limitations to bacterial interference in the bladder, other researchers have attempted to change the microbiome through indwelling catheters. Individuals who use indwelling catheters are at risk for UTIs, as bacteria can grow in the catheter and make its way back up into the bladder. To counter this, some researchers have observed the impact of coating indwelling catheters with non-harmful bacteria in attempts to reduce rates of UTI. Using the concept of bacterial interference again, the purpose of coating an indwelling catheter is to prevent harmful bacteria from growing inside it, thus preserving the bladder microbiota. These studies (weak evidence) found this method decreased the average number of UTIs experienced per year, and that using bacterial interference in catheters is a successful strategy for preventing the growth of harmful bacteria.
Changes to the vaginal microbiome after SCIThe vaginal microbiota is primarily dominated by Lactobacilli bacteria, which act as a first line of defence against harmful bacteria. This is done by Lactobacilli creating an acidic environment, competing for nutrients and growth sites, and stimulating the immune system. As a result, the vagina is protected from the growth of harmful bacteria, including those causing sexually transmitted infections (STIs). In one study (weak evidence), researchers found that women with SCI have less Lactobacilli bacteria and more bacteria associated with UTIs and yeast infections. Overall, there is limited evidence demonstrating microbiome differences in the urinary and reproductive systems of people with SCI. More research is needed to determine the implications of these variations and whether intervention is beneficial or necessary. |
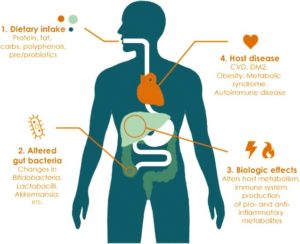
Lifestyle factors can have a large impact on the bacterial composition in the gut. This in turn can cause biological changes that may predispose an individual to long-term diseases.11
The numerous factors known to affect the balance of the gut microbiome, and their relationship to SCI are discussed below.
Diet
Diet has a large impact on the composition of the bacteria in the gut. In particular, processed foods in the Western diet may contribute to decreases in microbiome function and diversity. Conversely, a diet that is comprised of a variety of whole foods and probiotics can promote a diverse community of bacteria. Many studies with weak to moderate evidence have demonstrated an association between the bacterial community in the gut and the development of diseases such as diabetes and obesity. However, there is still much to learn about the functions of the gut microbiome before we can find an optimal approach to diet that will control microbiome-induced chronic diseases.
Alcohol

Drinking alcohol can affect the integrity of the gut microbiome, but these effects may be dependent on the type of alcohol consumed. One study in able-bodied males found that those who consumed gin had decreased numbers of beneficial gut bacteria. On the other hand, those who consumed red wine had decreased numbers of harmful bacteria and increased numbers of beneficial bacteria. The researchers believed that moderate consumption of red wine provided a source of polyphenols which may explain differences seen between the two groups. Polyphenols are compounds found in plants that may have prebiotic-like effects. While the effects of alcohol on the microbiome in SCI are unknown, alcohol should be limited to avoid the known health risks on other body systems.
Medications
Antibiotics are a well-known class of drugs that can disrupt the growth of both harmful and beneficial organisms in the gut. This can effectively decrease the number and diversity of the bacteria. Susceptibility to urinary tract and lung infections and pressure ulcers is increased following SCI. Because antibiotics are frequently used to treat these conditions, people with SCI may experience further disruptions to an already disrupted microbiome. Some may also report fatigue, emotional, or neurological issues with antibiotic use, suggesting that what is happening in the gut can have an effect in other parts of the body.
Physical Activity
 There is large variability in the amount of exercise performed by people with SCI, but most do not engage in any. Various studies on able-bodied individuals report a greater amount of certain healthy gut bacteria in physically active people compared to less active people. Thus, in SCI there may be a missed opportunity for physically inactive people to benefit from these healthy bacteria in their gut, some of which have anti-inflammatory effects and can protect from obesity.
There is large variability in the amount of exercise performed by people with SCI, but most do not engage in any. Various studies on able-bodied individuals report a greater amount of certain healthy gut bacteria in physically active people compared to less active people. Thus, in SCI there may be a missed opportunity for physically inactive people to benefit from these healthy bacteria in their gut, some of which have anti-inflammatory effects and can protect from obesity.
Refer to our chapter on Exercise Guidelines to learn more about physical activity following SCI.
Sleep
Sleep problems occur more commonly in individuals with SCI compared with the general population. This is important because sleep deprivation can cause disruptions in cognition, immune function, and many other body functions. A recent study looked at how the lack of sleep impacted bacteria in the gut among the general population. It found that just two consecutive days of sleep deprivation lead to increased amounts of bacteria that are implicated in conditions such as weight gain and diabetes. These conditions are already prevalent in people living with SCI.
Smoking

Smoking can lead to unwanted effects on the gut microbiome.14
There is evidence that smoking can cause negative changes in the diversity of the gut microbiome. Notably, the bacterial composition changes caused by smoking appear to be similar to the changes brought about by conditions like inflammatory bowel disease and obesity. Not only does smoking upset the balance of the microbiome, but it can lead to many short-term and long-term consequences like pneumonia which is especially harmful in people with SCI who have pre-existing breathing problems.
Stress
Recent evidence suggests a link between stress and negative changes in the gut microbiome. Stress may play a role in gut bacteria disruptions following spinal cord injury as people with SCI experience both massive physical stress from the injury itself and significant psychological stress due to dramatic life changes.
There is limited data on interventions that affect the gut microbiome in the SCI population. Proposed interventions include the use of probiotics, prebiotics, and fecal transplantation.
Probiotics
 Probiotics are live organisms that can be consumed to replenish the microbiome. Probiotics are available as supplements and are often present in cultured/fermented food products like yogurt, kefir, sauerkraut, kimchi, and miso. However, some of these food sources contain high levels of salt, saturated fat, or other ingredients associated with health risks, so ensuring moderation and variety of these types of food is important. Often times, many of these products to not contain large enough concentrations of probiotic bacteria to have a meaningful benefit. Also, production of supplements is not government regulated so there is no way to know if the amount and type of bacteria listed on a supplement label is actually found in that product.
Probiotics are live organisms that can be consumed to replenish the microbiome. Probiotics are available as supplements and are often present in cultured/fermented food products like yogurt, kefir, sauerkraut, kimchi, and miso. However, some of these food sources contain high levels of salt, saturated fat, or other ingredients associated with health risks, so ensuring moderation and variety of these types of food is important. Often times, many of these products to not contain large enough concentrations of probiotic bacteria to have a meaningful benefit. Also, production of supplements is not government regulated so there is no way to know if the amount and type of bacteria listed on a supplement label is actually found in that product.
Individuals with SCI frequently receive antibiotics given their increased risk of bacterial infections and this puts people with SCI at risk for antibiotic-associated diarrhea. One study with moderate evidence showed that probiotic drinks may prevent dysbiosis in people with SCI who are at risk of antibiotic-associated diarrhea. Another study with moderate evidence supported the use of probiotics after SCI as treatment for antibiotic-associated diarrhea by shortening the course of diarrhea by about 2 days. More research is needed to confirm these results and determine the safety and effectiveness of probiotics in people with SCI.
Antibiotic-associated diarrhea vs. C. difficile-associated diarrhea The bacterium Clostridium difficile is responsible for C. difficile-associated diarrhea.16 Antibiotic-associated diarrhea is defined as the passing of three or more loose, watery stools per day due to taking oral antibiotics. This form of diarrhea generally requires little to no treatment and stops after discontinuation of the antibiotics. Antibiotics can cause dysbiosis in the gut, leading to increased vulnerability to Clostridium difficile bacteria (also known as C. difficile or C. diff). This pathogenic bacterium releases a toxin that can cause diarrhea as well as other signs of infection such as fever and inflammation. This form of diarrhea, known as C. difficile-associated diarrhea requires treatment to get rid of the bacteria |
Prebiotics
Prebiotics are dietary substances that are fermented or broken down by bacteria. In this way, prebiotics support the growth of beneficial gut bacteria by acting as a nutrient source. Foods high in fermentable fibres contain prebiotics. Examples of prebiotic-containing sources include whole grain products like barley as well as fruits and vegetables like bananas, onions, and asparagus.
The prebiotic lactulose is widely known as a treatment for constipation and hepatic encephalopathy (decreased brain function due to liver failure). Research suggests that prebiotics may also be a potential treatment for irritable bowel disease, but less is known about the use of prebiotics in other conditions. Although consuming 5-20 g/day of prebiotics was shown to significantly increase gut bacteria, there is insufficient data on the use of prebiotics in SCI to draw any conclusions at this time
Fecal transplantation
In one case study (weak evidence), a male with tetraplegia experiencing recurrent C. difficile infection was successfully treated with antibiotics following fecal transplantation (also known as fecal microbiota transplant or FMT). The researchers reported that transplants given through the oral route may be more feasible to avoid adverse effects related to transplants given through colonoscopies.
In another case study (weak evidence) of a male with tetraplegia, fecal transplantation resulted in resolution of C. difficile infection. Other noted benefits following his fecal transplant included a reduction in antibiotic-resistant organisms, episodes of sepsis (blood poisoning), infections, and antibiotic use.
What are fecal transplants Stool can be freeze-dried and placed into capsules in preparation for fecal transplantation.17 Fecal transplantation involves the replacement of gut bacteria by transferring stool from a healthy donor into the digestive tract of the recipient. Delivery methods include enemas, oral capsules of frozen stool, colonoscopies, rectal tubes, or feeding tubes. Fecal transplants are currently used as a treatment option after multiple failed courses of antibiotics in people with recurrent infections due to C. difficile bacteria. It is believed that introducing stool containing organisms into a recipient’s gut enhances microbiome diversity and increases resistance to pathogenic organisms. However, fecal transplants are not without risk. Side effects that have been reported in studies include constipation, diarrhea, stomach upset, and fever. Other negative effects may result from the endoscopy procedure (e.g. bleeding) or the transmission of pathogenic organisms (ex. infection). Fecal transplantation has been gaining attention as a potential management option for other conditions like inflammatory bowel disease, inflammatory bowel syndrome, hepatic encephalopathy, autism, metabolic syndrome, and obesity. Long-term safety data is not well-defined, but with the surge of ongoing studies, this gap may be filled in the near future. |
Differences in bacterial composition have been identified in people with SCI and people without. As dysbiosis has been linked to various chronic diseases, maintaining a healthy gut microbiome may be a target to prevent or reduce the development of many long-term complications that develop after SCI.
There are currently limited studies on interventions affecting the gut microbiome in people with SCI. Diet has been demonstrated to have a significant role in shaping the microbiome and can be optimized by eating a healthy, plant-based diet. Probiotics may also be consumed to counteract some negative effects of antibiotics. Research in the able-bodied population also suggests that engaging in regular physical activity, achieving adequate sleep, avoiding smoking, and reducing stress may be key in supporting good bacteria and reducing bad gut bacteria.
We have only just begun to scratch the surface of how important the role of the microbiome is in various functions, and its relationship with genetics and the physical environment. Until more research evidence is available, the best course of action is to consult your health provider to find out how lifestyle factors can be modified to enhance the health of your microbiome.
For a review of how we assess evidence at SCIRE Community and advice on making decisions, please see SCIRE Community Evidence.
Evidence for “What is the gut microbiome” is based on:
Valdes, A. M., Walter, J., Segal, E., & Spector, T. D. (2018). Role of the gut microbiota in nutrition and health. BMJ (Online), 361, 36–44. https://doi.org/10.1136/bmj.k2179
Rescigno, M. (2014). Intestinal microbiota and its effects on the immune system. Cellular Microbiology, 16(7), 1004–1013. https://doi.org/10.1111/cmi.12301
Darouiche, R. O., & Hull, R. A. (2012). Bacterial interference for prevention of urinary tract infection. Clinical Infectious Diseases, 55(10), 1400–1407. https://doi.org/10.1093/cid/cis639
Rescigno, M. (2014). Intestinal microbiota and its effects on the immune system. Cellular Microbiology, 16(7), 1004–1013. https://doi.org/10.1111/cmi.12301
Ma, B.; Forney, L.; Ravel, J. (2013). The vaginal microbiome: rethinking health and diseases, 371–389.
Bull, M. J., & Plummer, N. T. (2014). Part 1: The Human Gut Microbiome in Health and Disease. Integrative medicine (Encinitas, Calif.), 13(6), 17–22
Bäckhed, F., Ding, H., Wang, T., Hooper, L. V, Koh, G. Y., Nagy, A., … Gordon, J. I. (2004). The gut microbiota as an environmental factor that regulates fat storage. Proceedings of the National Academy of Sciences of the United States of America, 101(44), 15718–15723. https://doi.org/10.1073/pnas.0407076101
Kigerl, K. A., Hall, J. C. E., Wang, L., Mo, X., Yu, Z., & Popovich, P. G. (2016). Gut dysbiosis impairs recovery after spinal cord injury. The Journal of Experimental Medicine, 213(12), 2603–2620. https://doi.org/10.1084/jem.20151345
Collins, S. M., Surette, M., & Bercik, P. (2012). The interplay between the intestinal microbiota and the brain. Nature Reviews Microbiology, 10(11), 735–742. https://doi.org/10.1038/nrmicro2876
Jandhyala, S., Talukdar, R., Subramanyam, C., Vuyyuru, H., Sasikala, M., & Reddy, D. (2015). Role of the normal gut microbiota. World Journal of Gastroenterology, 21(29), 8836–8847. https://doi: 10.3748/wjg.v21.i29.8787
Linsenmeyer, T. (2018). Catheter-associated urinary tract infections in persons with neurogenic bladders. Journal of Spinal Cord Medicine, 41(2), 132-141. https://doi.org/10.1080/10790268.2017.1415419
Tanaka, M., & Nakayama, J. (2017). Development of the gut microbiota in infancy and its impact on health in later life. Allergology International, 66(4), 515–522. https://doi.org/10.1016/j.alit.2017.07.010
Voreades, N., Kozil, A., & Weir, T. L. (2014). Diet and the development of the human intestinal microbiome. Frontiers in Microbiology, 5, 494. https://doi.org/10.3389/fmicb.2014.00494
Evidence for “What happens when the gut microbiome is out of balance?” is based on:
Kigerl, K.A., & Popovich, P.G. (2019). Gut Dysbiosis and Recovery of Function After Spinal Cord Injury. Oxford Research Encyclopedia of Neuroscience. https://doi.org/10.1093/acrefore/9780190264086.013.242
Cao, S., Feehley, T. J., & Nagler, C. R. (2014). The role of commensal bacteria in the regulation of sensitization to food allergens. FEBS Letters, 588(22), 4258–4266. https://doi.org/10.1016/j.febslet.2014.04.026
Foster, J. A., & McVey Neufeld, K.-A. (2013). Gut–brain axis: how the microbiome influences anxiety and depression. Trends in Neurosciences, 36(5), 305–312. https://doi.org/10.1016/j.tins.2013.01.005
Maeda, Y., & Takeda, K. (2017). Role of Gut Microbiota in Rheumatoid Arthritis. Journal of Clinical Medicine, 6(6). https://doi.org/10.3390/jcm6060060
Hold, G. L., Smith, M., Grange, C., Watt, E. R., El-Omar, E. M., & Mukhopadhya, I. (2014). Role of the gut microbiota in inflammatory bowel disease pathogenesis: what have we learnt in the past 10 years? World Journal of Gastroenterology, 20(5), 1192–1210. https://doi.org/10.3748/wjg.v20.i5.1192
Castaner, O., Goday, A., Park, Y.-M., Lee, S.-H., Magkos, F., Shiow, S.-A. T. E., & Schröder, H. (2018). The Gut Microbiome Profile in Obesity: A Systematic Review. International Journal of Endocrinology, 2018, 1–9. https://doi.org/10.1155/2018/4095789
Aw, W., & Fukuda, S. (2018). Understanding the role of the gut ecosystem in diabetes mellitus. Journal of Diabetes Investigation, 9(1), 5–12. https://doi.org/10.1111/jdi.12673
Tilg, H., Kaser, A. (2011). Gut microbiome, obesity, and metabolic dysfunction. Journal of Clinical Investigation, 121(6), 2126-32. https://doi.org/10.1172/JCI58109
Murri, M., Leiva, I., Gomez-Zumaquero, J. M., Tinahones, F. J., Cardona, F., Soriguer, F., & Queipo-Ortuño, M. I. (2013). Gut microbiota in children with type 1 diabetes differs from that in healthy children: a case-control study. BMC Medicine, 11(1), 46. https://doi.org/10.1186/1741-7015-11-46
Rousseaux, C., Thuru, X., Gelot, A., Barnich, N., Neut, C., Dubuquoy, L., … Desreumaux, P. (2007). Lactobacillus acidophilus modulates intestinal pain and induces opioid and cannabinoid receptors. Nature Medicine, 13(1), 35–37. https://doi.org/10.1038/nm1521
Jiang, C., Li, G., Huang, P., Liu, Z., & Zhao, B. (2017). The Gut Microbiota and Alzheimer’s Disease. Journal of Alzheimer’s Disease, 58(1), 1–15. https://doi.org/10.3233/JAD-161141
Zhang, C., Zhang, W., Zhang, J., Jing, Y., Yang, M., Du, L., … Li, J. J. J. (2018). Gut microbiota dysbiosis in male patients with chronic traumatic complete spinal cord injury. Journal of Translational Medicine, 16(1), 353. https://doi.org/10.1186/s12967-018-1735-9
Waldman, A. J., & Balskus, E. P. (2018). The Human Microbiota, Infectious Disease, and Global Health: Challenges and Opportunities. ACS Infectious Diseases, 4(1), 14–26. https://doi.org/10.1021/acsinfecdis.7b00232
Myers, J., Lee, M., & Kiratli, J. (2007). Cardiovascular Disease in Spinal Cord Injury. American Journal of Physical Medicine & Rehabilitation, 86(2), 142–152. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/17251696
Sauerbeck, A.D., Laws, J.L., Bandaru, V.V., Popovich, P.G., Haughey, N.J., & McTigue, D.M. (2015). Spinal cord injury causes chronic liver pathology in rats. Journal of Neurotrauma, 32(3), 159–169. https://doi.org/10.1089/neu.2014.3497
Boekamp, J. R., Overholser, J. C., & Schubert, D. S. P. (1996). Depression following a Spinal Cord Injury. The International Journal of Psychiatry in Medicine, 26(3), 329–349. https://doi.org/10.2190/CMU6-24AH-E4JG-8KBN
Elliott, T. R., & Frank, R. G. (1996). Depression following spinal cord injury. Archives of Physical Medicine and Rehabilitation, 77(8), 816–823. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8702378
Mehta, S., Robert, M. A., Loh, E., Short, C., Frcpc, M. D., Wolfe, D. L., … Msc, H. (2013). Pain Following Spinal Cord Injury. Retrieved from www.scireproject.com
Evidence for “What changes occur in the gut microbiome after SCI?” is based on:
Kigerl, K.A., Zane, K., Adams, K., Sullivan, M.B., & Popovich, P.G. (2020). The spinal cord-gut-immune axis as a master regulator of health and neurological function after spinal cord injury. Experimental Neurology, 323, 113085. https://doi.org/10.1016/j.expneurol.2019.113085
Gungor, B., Adiguzel, E., Gursel, I., Yilmaz, B., & Gursel, M. (2016). Intestinal Microbiota in Patients with Spinal Cord Injury. PLOS ONE, 11(1), e0145878. https://doi.org/10.1371/journal.pone.0145878
Choong, S., & Whitfield, H. (2000). Biofilms and their role in infections in urology. BJU International, 86, 935–941
Noller, C.M., Groah, S.L., Nash, M.S. (2017). Inflammatory Stress Effects on Health and Function After Spinal Cord Injury. Topics in Spinal Cord Injury Rehabilitation, 23(3), 207–217. https://doi.org/10.1310/sci2303-207
Liu, J., An, H., Jiang, D., Huang, W., Zou, H., Meng, C., Li, H. (2004). Study of bacterial translocation from gut after paraplegia caused by spinal cord injury in rats. Spine, 29(2):164–169. https://doi.org/10.1097/01.BRS.0000107234.74249.CD
Kigerl, K. A., Hall, J. C. E., Wang, L., Mo, X., Yu, Z., & Popovich, P. G. (2016). Gut dysbiosis impairs recovery after spinal cord injury. The Journal of Experimental Medicine, 213(12), 2603–2620. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/2781092
Zhang, C., Zhang, W., Zhang, J., Jing, Y., Yang, M., Du, L., … Li, J. (2018). Gut microbiota dysbiosis in male patients with chronic traumatic complete spinal cord injury. Journal of Translational Medicine, 16(1), 353. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/30545398
Jeffrey, E. (2018). Investigation of Spinal Cord Injury-Induced Gastrointestinal Dysfunction and Related Microbiota, Fungal, and Intestinal Alterations in a Rat Model and Humans with Spinal Cord Injury. University of Miami. Retrieved from https://scholarlyrepository.miami.edu/cgi/viewcontent.cgi?article=1738&context=oa_theses
Evidence for “Comparing gut bacteria between different populations” is based on:
Nguyen, T.T., Kosciolek, T., Maldonado, Y., Daly, R.E., Martin, A.S., McDonald, D., … Jeste, D.V. (2019) Differences in gut microbiome composition between persons with chronic schizophrenia and healthy comparison subjects. Schizophrenia Research, 204, 23–29. https://doi.org/10.1016/j.schres.2018.09.014
Sedighi, M., Razavi. S., Navab-Moghadam, F., Khamseh, M.E., Alaei-Shahmiri, F., Mehrtash, A., Amirmozafari, N. (2017). Comparison of gut microbiota in adult patients with type 2 diabetes and healthy individuals. Microbial Pathogenesis, 111, 362–369. https://doi.org/10.1016/j.micpath.2017.08.038
Schnorr, S. L., Candela, M., Rampelli, S., Centanni, M., Consolandi, C., Basaglia, G., … Crittenden, A. N. (2014). Gut microbiome of the Hadza hunter-gatherers. Nature Communications, 5, 3654. https://doi.org/10.1038/ncomms4654
Martínez, I., Stegen, J. C., Maldonado-Gómez, M. X., Eren, A. M., Siba, P. M., Greenhill, A. R., & Walter, J. (2015). The gut microbiota of rural papua new guineans: composition, diversity patterns, and ecological processes. Cell Reports, 11(4), 527–538. https://doi.org/10.1016/j.celrep.2015.03.049
De Filippo, C., Cavalieri, D., Di Paola, M., Ramazzotti, M., Poullet, J.B., Massart, S., Collini, S., Pieraccini, G., Lionetti, P.. (2010). Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proceedings of the National Academy of Sciences of the United States of America, 107, 33, 14691–14696. https://doi.org/10.1073/pnas.1005963107
Evidence for “What changes occur to the bladder microbiome after SCI?” is based on:
Groah, S. L., Pérez-Losada, M., Caldovic, L., Ljungberg, I. H., Sprague, B. M., Castro-Nallar, E., … Pohl, H. G. (2016). Redefining Healthy Urine: A Cross-Sectional Exploratory Metagenomic Study of People With and Without Bladder Dysfunction. Journal of Urology, 196(2), 579–587. https://doi.org/10.1016/j.juro.2016.01.088
Fouts, D. E., Pieper, R., Szpakowski, S., Pohl, H., Knoblach, S., Suh, M.-J., … Groah, S. L. (2012). Integrated next-generation sequencing of 16S rDNA and metaproteomics differentiate the healthy urine microbiome from asymptomatic bacteriuria in neuropathic bladder associated with spinal cord injury. Journal of Translational Medicine, 10, 174. https://doi.org/10.1186/1479-5876-10-174
Darouiche, R. O., & Hull, R. A. (2012). Bacterial interference for prevention of urinary tract infection. Clinical Infectious Diseases, 55(10), 1400–1407. https://doi.org/10.1093/cid/cis639
Bossa, L., Kline, K., McDougald, D., Lee, B. B., & Rice, S. A. (2017). Urinary catheter-associated microbiota change in accordance with treatment and infection status. PloS One, 12(6), e0177633. https://doi.org/10.1371/journal.pone.0177633
Darouiche, R. O., Green, B. G., Donovan, W. H., Chen, D., Schwartz, M., Merritt, J., … Hull, R. A. (2011). Infectious Diseases Multicenter Randomized Controlled Trial of Bacterial Interference for Prevention of Urinary Tract Infection in Patients With Neurogenic Bladder. Infectious Diseases, 78(2), 341–610. https://doi.org/1016/j.urology.2011.03.062
Hull, R., Rudy, D., Donovan, W., Svanborg, C., Wieser, I., Stewart, C., & Darouiche, R. (2000). Urinary tract infection prophylaxis using Escherichia coli 83972 in spinal cord injured patients. Journal of Urology, 163(3), 872–877.
Prasad, A., Riosa, S., Darouiche, R. O., & Trautner, B. W. (2009). A bacterial interference strategy for prevention of UTI in persons practicing intermittent catheterization. Spinal Cord, 47, 565–569. https://doi.org/10.1038/sc.2008.166
Sundén, F., Håkansson, L., Ljunggren, E., & Wullt, B. (2010). Escherichia coli 83972 Bacteriuria Protects Against Recurrent Lower Urinary Tract Infections in Patients With Incomplete Bladder Emptying. Journal of Urology, 184(1), 179–185. https://doi.org/10.1016/j.juro.2010.03.024
Trautner, B.W., Hull, R.A., & Darouiche, R.O. (2003). Escherichia coli 83972 inhibits catheter adherence by a broad spectrum of uropathogens. Urology, 61(5),1059–1062. https://doi.org/0.1016/s0090-4295(02)02555-4
Ceccarani, C., Foschi, C., Parolin, C., D’Antuono,A., Gaspari, V., Consolandi, C., … Marangoni, A. (2019). Diversity of vaginal microbiome and metabolome during genital infections. Scientific Reports, 9, 14095. https://doi.org/10.1038/s41598-019-50410-x
Evidence for “Changes to the vaginal microbiome after SCI” is based on:
Pires, C.V., Linhares, I.M., Serzedello, F., Fukazawa, E.I., Baracat, E.C., & Witkin, S.S. (2016). Alterations in the Genital Microbiota in Women With Spinal Cord Injury. Obstetrics & Gynecology, 127(2), 273-278. https://doi.org/10.1097/AOG.0000000000001257
Evidence for “What affects the gut microbiome?” is based on:
Coyle, D. (2017). 8 Surprising Things That Harm Your Gut Bacteria. Retrieved February 12, 2019, from https://www.healthline.com/nutrition/8-things-that-harm-gut-bacteria
Makki, K., Deehan, E. C., Walter, J., & Bäckhed, F. (2018, June 13). The Impact of Dietary Fiber on Gut Microbiota in Host Health and Disease. Cell Host and Microbe. Cell Press.
Claesson, M. J., Jeffery, I. B., Conde, S., Power, S. E., O’Connor, E. M., Cusack, S., … O’Toole, P. W. (2012). Gut microbiota composition correlates with diet and health in the elderly. Nature, 488(7410), 178–184. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22797518
Lozupone, C. A., Stombaugh, J. I., Gordon, J. I., Jansson, J. K., & Knight, R. (2012). Diversity, stability and resilience of the human gut microbiota. Nature, 489(7415), 220–230. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22972295
Singer-Englar, T., Barlow, G., & Mathur, R. (2019, January 2). Obesity, diabetes, and the gut microbiome: an updated review. Expert Review of Gastroenterology and Hepatology. Taylor and Francis Ltd.
Górowska-Kowolik, K., & Chobot, A. (2019). The role of gut micorbiome in obesity and diabetes. World Journal of Pediatrics, 15(4), 332–340.
David, L. A., Maurice, C. F., Carmody, R. N., Gootenberg, D. B., Button, J. E., Wolfe, B. E., … Turnbaugh, P. J. (2014). Diet rapidly and reproducibly alters the human gut microbiome. Nature, 505(7484), 559–563. Retrieved from http://www.nature.com/articles/nature12820
Queipo-Ortuño, M. I., Boto-Ordóñez, M., Murri, M., Gomez-Zumaquero, J. M., Clemente-Postigo, M., Estruch, R., … Tinahones, F. J. (2012). Influence of red wine polyphenols and ethanol on the gut microbiota ecology and biochemical biomarkers. The American Journal of Clinical Nutrition, 95(6), 1323–1334. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22552027
Evans, C. T., LaVela, S. L., Weaver, F. M., Priebe, M., Sandford, P., Niemiec, P., … Parada, J. P. (2008). Epidemiology of Hospital-Acquired Infections in Veterans With Spinal Cord Injury and Disorder. Infection Control & Hospital Epidemiology, 29(03), 234–242. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/18248306
Wolfe, D., McIntyre, A., Ravenek, K., Martin-Ginis, K., Cheung, A. L., Eng, J. J., … Hsieh, J. T. (2014). Physical Activity Participation Levels in SCI. Retrieved February 11, 2019, from https://scireproject.com/evidence/rehabilitation-evidence/physical-activity/increasing-physical-activity-participation-in-sci/physical-sci/
Zbogar, D., Eng, J. J., Miller, W. C., Krassioukov, A. V, & Verrier, M. C. (2016). Physical activity outside of structured therapy during inpatient spinal cord injury rehabilitation. Journal of Neuroengineering and Rehabilitation, 13(1), 99. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/27846851
Monda, V., Villano, I., Messina, A., Valenzano, A., Esposito, T., Moscatelli, F., … Messina, G. (2017). Exercise Modifies the Gut Microbiota with Positive Health Effects. Oxidative Medicine and Cellular Longevity, 2017, 1–8. Retrieved from https://www.hindawi.com/journals/omcl/2017/3831972/
Clarke, S. F., Murphy, E. F., O’Sullivan, O., Lucey, A. J., Humphreys, M., Hogan, A., … Cotter, P. D. (2014). Exercise and associated dietary extremes impact on gut microbial diversity. Gut, 63(12), 1913–1920. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25021423
Bressa, C., Bailén-Andrino, M., Pérez-Santiago, J., González-Soltero, R., Pérez, M., Montalvo-Lominchar, M. G., … Larrosa, M. (2017). Differences in gut microbiota profile between women with active lifestyle and sedentary women. PLOS ONE, 12(2), e0171352. Retrieved from https://dx.plos.org/10.1371/journal.pone.0171352
Estaki, M., Pither, J., Baumeister, P., Little, J. P., Gill, S. K., Ghosh, S., … Gibson, D. L. (2016). Cardiorespiratory fitness as a predictor of intestinal microbial diversity and distinct metagenomic functions. Microbiome, 4(1), 42. Retrieved from http://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-016-0189-7
Biering-Sørensen, F., Jennum, P., & Laub, M. (2009). Sleep disordered breathing following spinal cord injury. Respiratory Physiology and Neurobiology, 169(2), 165–170.
Benedict, C., Vogel, H., Jonas, W., Woting, A., Blaut, M., Schürmann, A., & Cedernaes, J. (2016). Gut microbiota and glucometabolic alterations in response to recurrent partial sleep deprivation in normal-weight young individuals. Molecular Metabolism, 5(12), 1175–1186. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/27900260
Savin, Z., Kivity, S., Yonath, H., & Yehuda, S. (2018). Smoking and the intestinal microbiome. Archives of Microbiology, 200(5), 677–684. Retrieved from http://link.springer.com/10.1007/s00203-018-1506-2
Stolzmann, K. L., Gagnon, D. R., Brown, R., Tun, C. G., & Garshick, E. (2010). Risk factors for chest illness in chronic spinal cord injury: a prospective study. American Journal of Physical Medicine & Rehabilitation, 89(7), 576–583. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/20463565
Clark, A., & Mach, N. (2016). Exercise-induced stress behavior, gut-microbiota-brain axis and diet: a systematic review for athletes. Journal of the International Society of Sports Nutrition, 13(1), 43. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/27924137
Tillisch, K., Mayer, E. A., Gupta, A., Gill, Z., Brazeilles, R., Le Nevé, B., … Labus, J. S. (2017). Brain Structure and Response to Emotional Stimuli as Related to Gut Microbial Profiles in Healthy Women. Psychosomatic Medicine, 79(8), 905–913. Retrieved from http://insights.ovid.com/crossref?an=00006842-201710000-00010
Knowles, S. R., Nelson, E. A., & Palombo, E. A. (2008). Investigating the role of perceived stress on bacterial flora activity and salivary cortisol secretion: A possible mechanism underlying susceptibility to illness. Biological Psychology, 77(2), 132–137. Retrieved from https://www.sciencedirect.com/science/article/pii/S0301051107001597
Kigerl, K. A., Hall, J. C. E., Wang, L., Mo, X., Yu, Z., & Popovich, P. G. (2016). Gut dysbiosis impairs recovery after spinal cord injury. Journal of Experimental Medicine, 213(12), 2603–2620.
Boekamp, J. R., Overholser, J. C., & Schubert, D. S. P. (1996). Depression following a Spinal Cord Injury. The International Journal of Psychiatry in Medicine, 26(3), 329–349. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8976473
Elliott, T. R., & Frank, R. G. (1996). Depression following spinal cord injury. Archives of Physical Medicine and Rehabilitation, 77(8), 816–823. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8702378
Evidence for “What treatments have a positive effect on the gut microbiome in people with SCI?” is based on:
Wong, S., Jamous, A., O’Driscoll, J., Sekhar, R., Weldon, M., Yau, C. Y., … Forbes, A. (2014). A Lactobacillus casei Shirota probiotic drink reduces antibiotic-associated diarrhoea in patients with spinal cord injuries: A randomised controlled trial. British Journal of Nutrition.
Curtin,P., Casella,G.D., & Turk, M.A. (2017). P7 Can probiotics shorten the duration of antibiotic associated diarrhea in spinal cord injury patients with neurogenic bowel? The Journal of Spinal Cord Medicine, 40(5), 605–625. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/28758546
Hod, K., & Ringel, Y. (2017). Treatment of Functional Bowel Disorders With Prebiotics and Probiotics. In The Microbiota in Gastrointestinal Pathophysiology: Implications for Human Health, Prebiotics, Probiotics, and Dysbiosis (pp. 355–364). Elsevier Inc.
Roberfroid, M. B. (2005). Introducing inulin-type fructans. British Journal of Nutrition, 93(S1), S13–S25.
Tuohy, K. M., Probert, H. M., Smejkal, C. W., & Gibson, G. R. (2003, August 1). Using probiotics and prebiotics to improve gut health. Drug Discovery Today.
Gibson, G. R., Probert, H. M., Loo, J. Van, Rastall, R. A., & Roberfroid, M. B. (2004). Dietary modulation of the human colonic microbiota: updating the concept of prebiotics. Nutrition Research Reviews, 17(2), 259–275.
Brechmann, T., Swol, J., Knop-Hammad, V., Willert, J., Aach, M., Cruciger, O., … Hamsen, U. (2015). Complicated fecal microbiota transplantation in a tetraplegic patient with severe Clostridium difficile infection. World Journal of Gastroenterology, 21(12), 3736–3740.
Crum-Cianflone, N. F., Sullivan, E., & Ballon-Landa, G. (2015). Fecal Microbiota Transplantation and Successful Resolution of Multidrug-Resistant-Organism Colonization. Journal of Clinical Microbiology, 53(6), 1986–1989. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25878340
Khanna, S., Vazquez-Baeza, Y., González, A., Weiss, S., Schmidt, B., Muñiz-Pedrogo, D. A., … Kashyap, P. C. (2017). Changes in microbial ecology after fecal microbiota transplantation for recurrent C. difficile infection affected by underlying inflammatory bowel disease. Microbiome, 5(1), 55. Retrieved from http://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-017-0269-3
Wang, J. W., Kuo, C. H., Kuo, F. C., Wang, Y. K., Hsu, W. H., Yu, F. J., … Wu, D. C. (2019, March 1). Fecal microbiota transplantation: Review and update. Journal of the Formosan Medical Association. Elsevier B.V.
Rossen, N. G., Fuentes, S., Van Der Spek, M. J., Tijssen, J. G., Hartman, J. H. A., Duflou, A., … Ponsioen, C. Y. (2015). Findings From a Randomized Controlled Trial of Fecal Transplantation for Patients With Ulcerative Colitis. Gastroenterology, 149(1), 110-118.e4.
Paramsothy, S., Paramsothy, R., Rubin, D. T., Kamm, M. A., Kaakoush, N. O., Mitchell, H. M., & Castaño-Rodríguez, N. (2017). Faecal microbiota transplantation for inflammatory bowel disease: A systematic review and meta-analysis. Journal of Crohn’s and Colitis, 11(10), 1180–1199.
Moayyedi, P., Surette, M. G., Kim, P. T., Libertucci, J., Wolfe, M., Onischi, C., … Lee, C. H. (2015). Fecal Microbiota Transplantation Induces Remission in Patients With Active Ulcerative Colitis in a Randomized Controlled Trial. Gastroenterology, 149(1), 102-109.e6.
Johnsen, P. H., Hilpüsch, F., Cavanagh, J. P., Leikanger, I. S., Kolstad, C., Valle, P. C., & Goll, R. (2018). Faecal microbiota transplantation versus placebo for moderate-to-severe irritable bowel syndrome: a double-blind, randomised, placebo-controlled, parallel-group, single-centre trial. The Lancet Gastroenterology and Hepatology, 3(1), 17–24.
Bajaj, J. S., Kassam, Z., Fagan, A., Gavis, E. A., Liu, E., Cox, I. J., … Gillevet, P. M. (2017). Fecal microbiota transplant from a rational stool donor improves hepatic encephalopathy: A randomized clinical trial. Hepatology, 66(6), 1727–1738.
Millan, B., Laffin, M., & Madsen, K. (2017, September 1). Fecal Microbiota Transplantation: Beyond Clostridium difficile. Current Infectious Disease Reports. Current Medicine Group LLC 1.
Kootte, R. S., Levin, E., Salojärvi, J., Smits, L. P., Hartstra, A. V., Udayappan, S. D., … Nieuwdorp, M. (2017). Improvement of Insulin Sensitivity after Lean Donor Feces in Metabolic Syndrome Is Driven by Baseline Intestinal Microbiota Composition. Cell Metabolism, 26(4), 611-619.e6.
Krajicek, E., Fischer, M., Allegretti, J. R., & Kelly, C. R. (2019, January 1). Nuts and Bolts of Fecal Microbiota Transplantation. Clinical Gastroenterology and Hepatology. W.B. Saunders.
Wang, Y., Wiesnoski, D. H., Helmink, B. A., Gopalakrishnan, V., Choi, K., DuPont, H. L., … Jenq, R. R. (2018). Fecal microbiota transplantation for refractory immune checkpoint inhibitor-associated colitis. Nature Medicine, 24(12), 1804–1808.
Image credits
- Modified from: Lactobacillus casei ©AJC1, CC BY-SA 2.0
- Modified from: Campylobacter bacteria ©Microbe World, CC BY-NC-SA 2.0
- Modified from: Koli Bacteria ©geralt geralt / 18959 images, CC0 1.0
- Modified from: jpg ©Lamiot, CC0 1.0
- Baby ©Nick Abrams, CC BY 3.0 US
- Modified from: Mazmanian SK, Lee YK. (2014). Interplay between intestinal microbiota and host immune system. Journal of Bacteriology and Virology, 44(1),1-9. CC BY-NC 3.0.
- Intestine segmentation ©Servier Medical Art, CC BY 3.0
- Modified from: Colon ©Servier Medical Art, CC BY 3.0
- The Earth seen from Apollo 17 ©NASA, Public Domain
- Modified from: Bacteria ©Maxim Kulikov, CC BY 3.0 US; urethra ©Prettycons, CC BY 3.0 US; and Zoom Out ©fahmionline, CC BY 3.0 US
- Modified from: Singh RK, Chang HW, Yan D, Lee KM, Ucmak D, Wong K. (2017). Influence of diet on the gut microbiome and implications for human health. Journal of Translational Medicine, 15, 73. CC BY 4.0.
- Red Wine bottle pouring ©Push Doctor, CC BY-NC 2.0
- Army Trials at Fort Bliss 160306-A-QR477-037 ©Adasia Ortiz, CC0 1.0
- Smoke ©Joffrey, CC BY-NC-ND 2.0
- yoghurt pack ©Oleksandr Panasovskyi, CC BY 3.0 US
- Clostridium difficile ©CDC, CC0 1.0
- Freeze-dried poop pills ©Patrik Nygren, CC BY-SA 2.0
Authors: Vanessa Mok, Dominik Zbogar | Reviewers: Janet Parker, Gita Joshi | Published: 23 December 2019 | Updated: ~
Adequate fibre intake is important to ensure proper nutrition after spinal cord injury (SCI). This page outlines the current recommendations for dietary fibre and its role in managing conditions such as neurogenic bowel in SCI.
Key Points
- Foods such as vegetables, fruits, legumes, and whole grains are great sources of dietary fibre.
- Research in the general population shows that increasing dietary fibre reduces the risk for heart disease, obesity, diabetes, high blood pressure, and certain cancers.
- Increasing dietary fibre in people with SCI may not have the same result as in the general population. It is important to continuously monitor how an increasing fibre intake affects you.
- Increasing fibre in the diet should be done incrementally and may require increased fluid intake to prevent constipation.
- An increased fibre intake may require a change in your bowel and bladder routine.
Dietary fibre is a kind of carbohydrate that is difficult for the body to break down, so it is not absorbed in the small intestines. Instead, it passes into the colon. Therefore, fibre supplies little to no calories.
Fibre can be classified into two types: soluble and insoluble. Both types of fibre play an important role in gut health and prevention of various health issues. Soluble fibre mixes with water in the intestine to form a gel-like substance that traps certain body wastes and moves them out of the body. Soluble fibre also decreases cholesterol, helps control blood sugar fluctuations, and feeds the good bacteria in the gut. Insoluble fibre absorbs and holds water, producing bulkier and uniform stool which helps with bowel movements, and it reduces the risk of colon cancer and diverticulitis among other benefits. Whole plant foods and fungi contain both types of fibre in varying amounts while animal food products contain no fibre.
| Soluble fibre | Insoluble fibre |
|
|
When the spinal cord is injured, some or all of the nerve signals that would normally allow the brain and bowel (intestine or ‘gut’) to communicate are blocked. This can contribute to a number of bowel changes known as neurogenic bowel dysfunction. They include:
- Reduced sensation
- Slowed movement of stool through the bowel
- Loss of bowel control
Depending on whether your injury is above or below T12, you may experience spastic bowel or flaccid bowel, respectively. Spastic bowel is characterized by increased muscle tone in the intestines and sphincters while flaccid bowel is characterized by decreased tone. This difference can play a role in how your body responds to changes in diet including increased fibre intake.
Dietary fibre is an important part of a bowel management program for neurogenic bowel. After a SCI, food moves through the bowels at a much slower pace. Slow movement means that food takes much longer to digest, which can lead to dry, hard stools and constipation. Too little fibre in the diet can worsen constipation, resulting in pain and difficulty when emptying the bowels. Fibre can increase bulk and soften stool. This stimulates bowel movements and makes stool easier to pass. Foods with high fibre content tend to be lower in calories too. As a result, diets that are low in fibre can contribute to uncontrolled weight gain and lead to less stable blood sugar levels after meals.
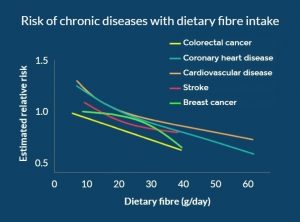
Figure 1. In the general population, with increasing dietary fibre, the risk for various lifestyle diseases decreases in a dose-response manner.8
Research in the general population shows that adequate dietary fibre intake is associated with a decreased risk of developing numerous chronic diseases, including heart disease, high blood pressure, obesity, stroke, type 2 diabetes, and intestinal diseases (e.g. constipation, hemorrhoids).
As people with SCI are more prone to developing these health conditions due to factors including sedentary lifestyle and changes in metabolism, getting enough fibre in the diet may provide long-term health benefits.
There is emerging evidence suggesting that an imbalance of bacteria in the gut is linked to the progression of chronic conditions including diabetes, obesity, pain, and neurogenic bowel dysfunction. Additionally, recent studies have demonstrated that imbalances to the bacterial composition in the gut may result following SCI. Since fibre supports the growth of healthy bacteria in the gut, a fibre-rich diet may help to decrease these health risks in people with SCI.
Refer to our article on the Microbiome in SCI for more information!
A detailed look at fibre in the diet of individuals with SCI shows similarity between countries:
- Canada (see the graph to the right): little variation between males and females or with age with values ranging from 15-23 g/day
- Switzerland: people with acute SCI average 14.4 g/day and those with chronic SCI get 15.6 g/day
- United States: 17.1 g/day
- Iran:17.9 g/day
| Individuals with SCI should not uniformly follow high fibre diets. For individuals with SCI, fibre should be increased slowly to avoid side effects and to assess tolerance. If symptoms of intolerance arise such as bloating or cramping, then one should try reducing or changing the type of fiber. |
 It is important to recognize that after a spinal cord injury, fibre can affect people differently and there is no agreed upon ideal amount of fibre for individuals with SCI. However, based on expert opinion, an initial diet containing no less than 15 g/day of fiber is recommended. One study (weak evidence) found that increasing dietary fibre from 25 g/day to 31 g/day with the addition of 40 g of “Kellogg’s All Bran” cereal a day to the diet worsened bowel function in 11 individuals with SCI. In fact, the higher fibre intake increased the time needed for food to move through the colon from 28 hours to 42 hours! While the Canadian recommendation for the general population is 25-38 grams per day, this study shows that individuals with SCI may respond differently to fibre. Further research is required on the effects of different types of fibre, as well as fluid intake on bowel function after an SCI.
It is important to recognize that after a spinal cord injury, fibre can affect people differently and there is no agreed upon ideal amount of fibre for individuals with SCI. However, based on expert opinion, an initial diet containing no less than 15 g/day of fiber is recommended. One study (weak evidence) found that increasing dietary fibre from 25 g/day to 31 g/day with the addition of 40 g of “Kellogg’s All Bran” cereal a day to the diet worsened bowel function in 11 individuals with SCI. In fact, the higher fibre intake increased the time needed for food to move through the colon from 28 hours to 42 hours! While the Canadian recommendation for the general population is 25-38 grams per day, this study shows that individuals with SCI may respond differently to fibre. Further research is required on the effects of different types of fibre, as well as fluid intake on bowel function after an SCI.
Increase fibre and increase water
 Drinking enough water during the day is important for your health and may help prevent complications such as urinary tract infections. There is a temptation to keep water intake low to reduce catheterization frequency or other disruptions to your bladder/bowel routine. But, when you increase fibre intake it is important to also increase fluid intake to compensate. Fibre sources such as fruits and vegetables naturally contain lots of water with all the fibre they provide. However, fibre supplements, cereals, or dried fruit, nuts, ground flax seed, and the like should be accompanied by increased water consumption. It is important to strike a balance between increased fluid intake, increased fibre, and the potential impacts on your bowel and bladder routine.
Drinking enough water during the day is important for your health and may help prevent complications such as urinary tract infections. There is a temptation to keep water intake low to reduce catheterization frequency or other disruptions to your bladder/bowel routine. But, when you increase fibre intake it is important to also increase fluid intake to compensate. Fibre sources such as fruits and vegetables naturally contain lots of water with all the fibre they provide. However, fibre supplements, cereals, or dried fruit, nuts, ground flax seed, and the like should be accompanied by increased water consumption. It is important to strike a balance between increased fluid intake, increased fibre, and the potential impacts on your bowel and bladder routine.
Interestingly, little to no attention is given in guidelines to how the source of fibre may affect the bowel. In one study in the general population, it was shown that doubling stool output could be accomplished with 10 g of grain or vegetable fibre while such a doubling required 25 g of fruit fibre. The interaction of different types of dietary fibre in SCI requires investigation.
The effect of increased fibre in individuals with SCI may differ depending on whether one has spastic or flaccid bowel. One study (weak evidence) interviewing individuals about their bowel routines noted that more individuals with flaccid bowel reported benefits by modifying their diet with high fibre foods than those with spastic bowel.
Given the benefits of dietary fibre in reducing a number of diseases, it makes sense to want to increase how much you get in your diet. Individuals with SCI should increase fibre in their diet slowly to avoid side effects. In addition, for some people, high amounts of fibre may not be tolerated and fibre should be reduced if it worsens their bowel function.
Assess how much dietary fibre you currently eat
- Take a week-long diet history by writing down what and how much you eat and drink every day for a week. You can then calculate your fibre based on the foods you have eaten using an online fibre calculator.
- At the same time, also record the effects of your current fibre intake on stool consistency (see the Bristol Stool Scale), frequency and duration of bowel movements.
- With this information, you will know how much fibre you are currently getting and how it affects your bowel routine. Then, you may decide to stay where you are or to increase your fibre intake.
Increase dietary fibre slowly and continue to monitor your diet
- If you decide to increase your fibre intake, proceed gradually and obtain fibre from a wide variety of sources as described in the beginning of this article.
- Make one or two changes a week such as adding a daily serving of fruit or switching to whole grain pasta and continue to keep track of stool consistency, frequency of bowel movements, as well as any symptoms of intolerance. Keep track of how your body responds to more fibre, different sources of fibre-containing foods and more fluids to help you make informed decisions.
- Recognize that some foods may not agree with you. These may be spicy foods that disrupt the digestive system or certain foods that cause more gas. Beans and cruciferous vegetables (like broccoli and Brussel sprouts) have a reputation for increasing flatulence, but this is usually temporary and your body adapts. Start off with small amounts of these foods and increase gradually. Recognize that you can develop a tolerance to certain foods.
- Should symptoms of intolerance occur (e.g., bloating, cramping, and gas), reduce your dietary fibre intake or try a different source of fibre.
- Balance the amount of water needed for optimal stool consistency with that needed for bladder management. Based on expert opinion, people with SCI should aim for a daily fluid intake of 500 mL more than the general population. This can be calculated by using the formula: 40 mL x body weight in kg + 500 mL.
Read our article on Bowel Changes After SCI for more information!
Incorporating higher dietary fibre intake into your life
- It is likely that increased dietary fibre and increased water in your diet will affect your bowel and bladder routine. Bowel movements may be required on a daily basis as opposed to every other day or less and more catheterizations may be required for the bladder.
- These consequences of increased dietary fibre intake need to be weighed by you and your caregivers. If the changes are not acceptable, a new balance must be reached that works for your lifestyle.
The main way to increase fibre is to make vegetables, fruit, whole grains, and plant-based protein foods the cornerstone of your diet, as per Canada’s Food Guide.
Eating a whole food plant-based diet to meet your fibre needs instead of supplements is preferred as whole foods provide nutritional benefits that fibre supplements do not. Indeed, studies which reduced the risk of disease with fibre used food and not supplements. It is not clear if fibre from supplements brings similar benefits. However, there may be situations where a fibre supplement is the best solution.
Below is an example from Dietitians of Canada of how a low fibre diet can be modified into a high fibre diet.
Other simple ways to increase fibre in your diet include:
- Choose whole fruit over fruit juices
- Try a fruit or vegetable you’ve never heard of
- Avoid peeling vegetables and fruits where appropriate
- Add legumes such as lentils, beans, and peas to soups, salads, and other dishes
- Add seaweed to soup
- Switch white for 100% % whole grain bread, pasta and rice
- Eat nuts and seeds as snacks or toppings to salads
- Use whole grain flour when baking
- Add ground flax seed to your morning oatmeal or smoothie
- Read food nutrition labels and choose foods containing more fibre
 Calculating the percent daily value for fibre
Calculating the percent daily value for fibre
The percent daily value (% DV) is a guideline to help you make informed food choices.
According to Canada’s Food Guide, food with 5% DV or less per serving size is considered little of a nutrient. On the other hand, food with 15% DV or more per serving size is considered a lot of a nutrient. To help reach the recommended amount of fibre in your diet, aim for food containing 15% DV or greater.
In Canada, the DV of fibre is 25 g/day. The box of crackers in the picture indicates that each serving size provides 2 g of fibre. The % DV would be calculated to be (2 g ÷ 25 g) x 100 = 8% DV.
Dietary fibre is an important part of a healthy bowel routine. Based on expert opinion, an initial diet containing at least 15 g/day of fiber is recommended in people with SCI. Increases in fibre should be individualized and done gradually. General population fibre guidelines may not be appropriate for people after SCI, and in some cases may worsen their bowel function.
Research in the general population shows that increasing fibre in the diet reduces the risk of many lifestyle diseases that individuals with SCI are at a higher risk of developing. If you are interested in increasing your dietary fibre, adding fibre requires an individualized approach.
The recommended individualized approach is to track your diet for a week before and then during the process of increasing fibre. With the information in the food journal, you can see out how much fibre and fluids you are getting on an average day and how increased fibre and fluids affect your bowel and bladder routine. Increases in dietary fibre should be progressed slowly and monitored closely by the individual and their health care provider.
For a review of how we assess evidence at SCIRE Community and advice on making decisions, please see SCIRE Community Evidence.
Coggrave M, Mills P, Williams R, Eng JJ, (2014). Bowel Dysfunction and Management Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors. Spinal Cord Injury Rehabilitation Evidence. Version 5.0. Vancouver: p 1-48.
Available from: https://scireproject.com/evidence/bowel-dysfunction-and-management/
Evidence for “Why is fibre important in spinal cord injury?” is based on:
Lockyer, S., Spiro, A., & Stanner, S. (2016). Dietary fibre and the prevention of chronic disease – should health professionals be doing more to raise awareness? Nutrition Bulletin, 41(3), 214–231. https://doi.org/10.1111/nbu.12212
Slavin, J. L. (2008). Position of the American Dietetic Association: health implications of dietary fiber. Journal of the American Dietetic Association, 108(10), 1716–1731. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/18953766
Gungor, B., Adiguzel, E., Gursel, I., Yilmaz, B., & Gursel, M. (2016). Intestinal Microbiota in Patients with Spinal Cord Injury. PLOS ONE, 11(1), e0145878. https://doi.org/10.1371/journal.pone.0145878
Zhang, C., Zhang, W., Zhang, J., Jing, Y., Yang, M., Du, L., … Li, J. (2018). Gut microbiota dysbiosis in male patients with chronic traumatic complete spinal cord injury. Journal of Translational Medicine, 16(1), 353. https://doi.org/10.1186/s12967-018-1735-9
Data for Figure 1 “Risk of chronic diseases with dietary fibre intake” is based on:
Aune, D., Chan, D. S. M., Lau, R., Vieira, R., Greenwood, D. C., Kampman, E., & Norat, T. (2011). Dietary fibre, whole grains, and risk of colorectal cancer: Systematic review and dose-response meta-analysis of prospective studies. BMJ (Online). http://doi.org/10.1136/bmj.d6617
Threapleton, D. E., Greenwood, D. C., Evans, C. E. L., Cleghorn, C. L., Nykjaer, C., Woodhead, C., … Burley, V. J. (2013). Dietary fibre intake and risk of cardiovascular disease: systematic review and meta-analysis. BMJ (Clinical Research Ed.), 347, f6879. http://doi.org/10.1136/bmj.f6879
Threapleton, D. E., Greenwood, D. C., Evans, C. E. L., Cleghorn, C. L., Nykjaer, C., Woodhead, C., … Burley, V. J. (2013). Dietary Fiber Intake and Risk of First Stroke. Stroke, 44(5), 1360–1368. http://doi.org/10.1161/STROKEAHA.111.000151
Aune, D., Chan, D. S. M., Greenwood, D. C., Vieira, A. R., Navarro Rosenblatt, D. A., Vieira, R., & Norat, T. (2012). Dietary fiber and breast cancer risk: A systematic review and meta-analysis of prospective studies. Annals of Oncology. http://doi.org/10.1093/annonc/mdr589
Evidence for “How much fibre do we get?” is based on:
Walters, J. L., Buchholz, A. C., Martin Ginis, K. A., & SHAPE-SCI Research Group. (2009). Evidence of dietary inadequacy in adults with chronic spinal cord injury. Spinal Cord, 47(4), 318–322. https://doi.org/10.1038/sc.2008.134
Perret, C., & Stoffel-Kurt, N. (2011). Comparison of nutritional intake between individuals with acute and chronic spinal cord injury. The Journal of Spinal Cord Medicine, 34(6), 569–575. https://doi.org/10.1179/2045772311Y.0000000026
Tomey, K. M., Chen, D. M., Wang, X., & Braunschweig, C. L. (2005). Dietary intake and nutritional status of urban community-dwelling men with paraplegia. Archives of Physical Medicine and Rehabilitation, 86(4), 664–671. https://doi.org/10.1016/j.apmr.2004.10.023
Sabour, H., Javidan, A. N., Vafa, M. R., Shidfar, F., Nazari, M., Saberi, H., … Emami Razavi, H. (2012). Calorie and macronutrients intake in people with spinal cord injuries: An analysis by sex and injury-related variables. Nutrition, 28(2), 143–147. https://doi.org/10.1016/j.nut.2011.04.007
Data for Figure 2 “Median fibre intake in people with SCI” is based on:
Walters, J. L., Buchholz, A. C., Martin Ginis, K. A., & SHAPE-SCI Research Group. (2009). Evidence of dietary inadequacy in adults with chronic spinal cord injury. Spinal Cord, 47(4), 318–322. https://doi.org/10.1038/sc.2008.134
Evidence for “How much fibre should you get?” is based on:
Health Canada. (2019). Fibre. Retrieved January 2, 2019, from https://www.canada.ca/en/health-canada/services/nutrients/fibre.html
Consortium for Spinal Cord Medicine. (1998). Clinical practice guidelines: Neurogenic bowel management in adults with spinal cord injury. Retrieved from http://www.pva.org/media/pdf/cpg_neurogenic bowel.pdf
Cameron, K. J., Nyulasi, I. B., Collier, G. R., & Brown, D. J. (1996). Assessment of the effect of increased dietary fibre intake on bowel function in patients with spinal cord injury. Spinal Cord, 34(5), 277–283. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8963975
de Vries, J., Birkett, A., Hulshof, T., Verbeke, K., & Gibes, K. (2016). Effects of Cereal, Fruit and Vegetable Fibers on Human Fecal Weight and Transit Time: A Comprehensive Review of Intervention Trials. Nutrients, 8(3), 130. https://doi.org/10.3390/nu8030130
Yim, S. Y., Yoon, S. H. S., Lee, I. Y., Rah, E. W., & Moon, H. W. (2001). A comparison of bowel care patterns in patients with spinal cord injury: Upper motor neuron bowel vs lower motor neuron bowel. Spinal Cord, 39(4), 204–207. https://doi.org/10.1038/sj.sc.3101131
Evidence for “How do you choose the right foods?” is based on:
Threapleton, D. E., Greenwood, D. C., Evans, C. E. L., Cleghorn, C. L., Nykjaer, C., Woodhead, C., … Burley, V. J. (2013). Dietary fibre intake and risk of cardiovascular disease: systematic review and meta-analysis. BMJ (Clinical Research Ed.), 347, f6879. https://doi.org/10.1136/bmj.f6879
Hartley, L., May, M. D., Loveman, E., Colquitt, J. L., & Rees, K. (2016). Dietary fibre for the primary prevention of cardiovascular disease. Cochrane Database of Systematic Reviews, (1), CD011472. https://doi.org/10.1002/14651858.CD011472.pub2
Dietitians of Canada. (2014). Healthy Eating Guidelines for Increasing your Fibre Intake. Retrieved from www.dietitians.ca
Health Canada. (2019). Percent daily value. Retrieved January 31, 2019, from https://www.canada.ca/en/health-canada/services/understanding-food-labels/percent-daily-value.html
Image credits
- Top view walnuts texture horizontal ©8photo, CC BY 2.0
- Almond almonds brazil nut ©David Stewart, CC BY 2.0
- Mr Beans ©Kenneth Leung, CC BY 2.0
- Vegan Nine Grain Whole Wheat Bread ©Veganbaking.net, CC BY-SA 2.0
- Banana © kimwang yip, CC0 1.0
- IMG_8230 1 ©Dennis Amith, CC BY-NC 2.0
- Modified from: Stomach Colon Rectum Diagram ©William Crochot, CC BY-SA 4.0
- Image ©SCIRE
- Modified from: Lactobacillus casei ©AJC1, CC BY-SA 2.0
- Modified from: Campylobacter bacteria ©Microbe World, CC BY-NC-SA 2.0
- Modified from: Koli Bacteria ©geralt geralt / 18959 images, CC0 1.0
- Modified from: jpg ©Lamiot, CC0 1.0
- Image ©SCIRE
- Kellogg’s Cereals #2 ©Like_the_Grand_Canyon, CC BY-NC 2.0
- Water ©rawpixel, CC0 1.0
- Image ©SCIRE
- Canada’s Food Guide ©Health Canada. All Rights Reserved. Adapted and reproduced with permission from the Minister of Health, 2019.
- sun ©Maxim Kulikov, CC BY 3.0 US
- sun ©johartcamp, CC BY 3.0 US
- sunset ©ruliani, CC BY 3.0 US
- Moon ©Three Six Five, CC BY 3.0 US
- Kombu ©Alice Wiegand, CC BY-SA 3.0
- Modified from: Ground flax seed ©Veganbaking.net, CC BY-SA 2.0
- Image ©SCIRE
- Daily Value meter ©Health Canada. All Rights Reserved. Adapted and reproduced with permission from the Minister of Health, 2019.

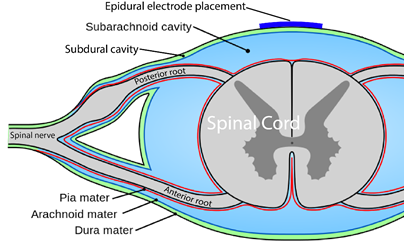
 While recent studies have shown that transmission of bacteria from the mother to the fetus is possible and occurs even before birth, it appears that much of the gut microbiome is established during delivery as the baby comes into contact with the microbes present in the mother’s birth canal and skin. Hence, a baby that is born through a C-section will have a different microbial composition. The gut microbiome continues to change due to organisms in the breastmilk; formula-fed infants will present with a different gut microbiome. The diversity of the microbiome increases until it resembles that of an adult around 3 years of age when a solid food diet is established.
While recent studies have shown that transmission of bacteria from the mother to the fetus is possible and occurs even before birth, it appears that much of the gut microbiome is established during delivery as the baby comes into contact with the microbes present in the mother’s birth canal and skin. Hence, a baby that is born through a C-section will have a different microbial composition. The gut microbiome continues to change due to organisms in the breastmilk; formula-fed infants will present with a different gut microbiome. The diversity of the microbiome increases until it resembles that of an adult around 3 years of age when a solid food diet is established.

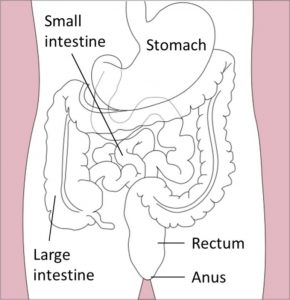
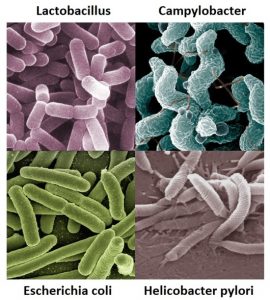
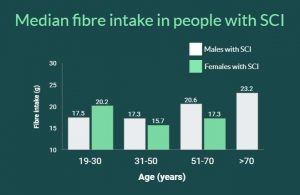


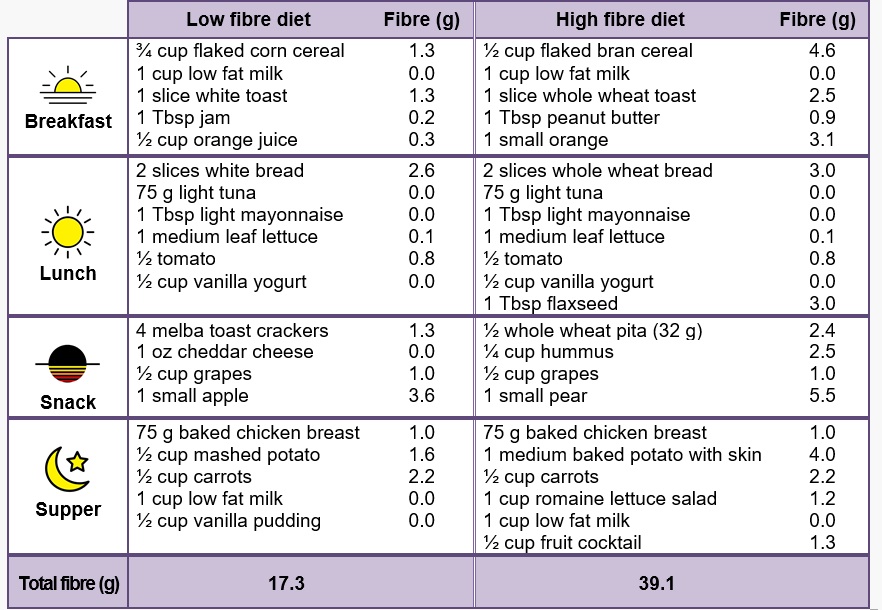




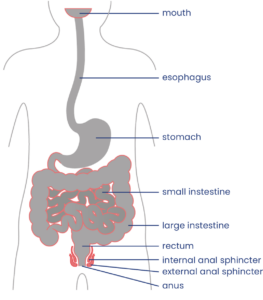





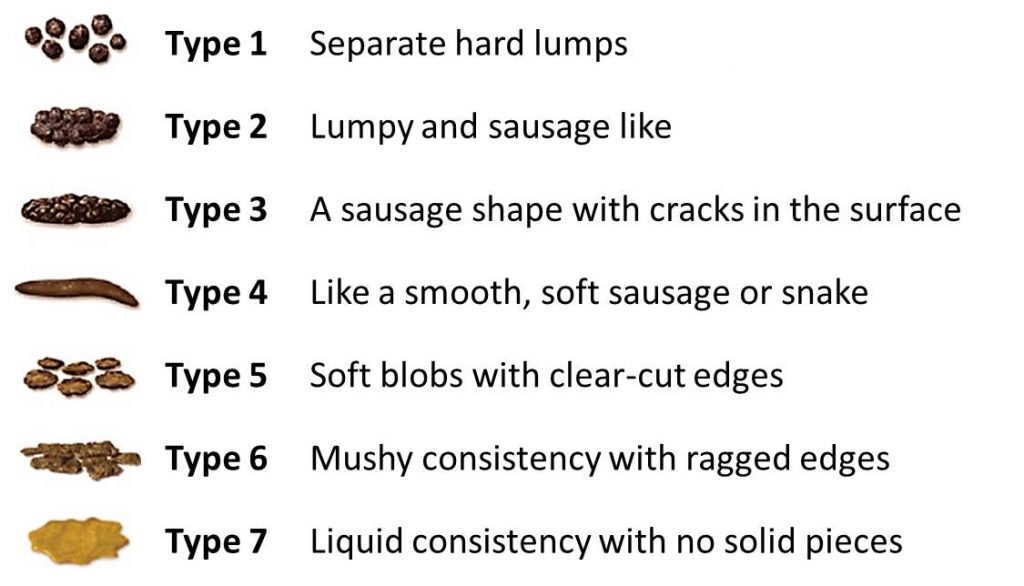
 Your bowel function and symptoms may change over time. Most health providers recommend people with SCI to have a check-up once every two to three years or if there are changes to bowel function to keep track of changes to your bowel function and care.
Your bowel function and symptoms may change over time. Most health providers recommend people with SCI to have a check-up once every two to three years or if there are changes to bowel function to keep track of changes to your bowel function and care. every day or every other day to empty the bowel. There is a wide range of different components that may make up a bowel routine, such as hands-on emptying techniques, diet and lifestyle changes, and the use of
every day or every other day to empty the bowel. There is a wide range of different components that may make up a bowel routine, such as hands-on emptying techniques, diet and lifestyle changes, and the use of 
 People with injuries at T6 and above may trigger
People with injuries at T6 and above may trigger 


 The
The