Author: Sharon Jang | Reviewer: Courtney Pollock | Published: 18 October 2023 | Updated: ~
Key Points
- Staying active after SCI has many benefits, but structured workouts may not be for everyone. Sports may be a good alternative to stay physically active.
- Adapted sports (sometimes called “adaptive sports”) are sports that use modified equipment to allow individuals of all abilities to participate.
- Participating in adapted sports is a great way to build social connections with others and to become a part of a community.
- There are a variety of sports that can be played including cycling, court sports, winter sports, and water sports. This article introduces various adapted sports and the required equipment to partake in them.
 Staying physically active after SCI is important for your health. There is moderate to strong evidence that physical activity has many benefits after SCI including:
Staying physically active after SCI is important for your health. There is moderate to strong evidence that physical activity has many benefits after SCI including:
- Allowing you to perform everyday activities (e.g., shopping, cooking, transferring) with more ease,
- Improving depression and quality of life,
- Increasing muscle strength and endurance,
- Management of blood sugar levels,
- Helping you to breathe with more ease,
- Reducing pain and spasticity.
Although going to a gym is one common way to get moving, there are a variety of adapted sports that can also be played. While this article discusses a selection of adapted sports (including handcycling, court sports, winter sports, and water sports), it should be noted that almost any sport can be adapted for participation after SCI.
Refer to our article on Physical Activity for more information!
Adapted sports are sports that can be played with equipment and approaches that are adapted to a person’s physical abilities. Many adapted sports have been altered in one of many ways to promote accessibility. Some of these adaptations include changes to the rules of a game, modifications in the equipment, or specialized equipment to allow you to partake in a sport.
 Athlete Classification
Athlete Classification
There are different levels of adapted sports, ranging from recreational (or just for fun and fitness) to competition. Should you want to become competitive, classifications are used to ensure that competition is equal and fair. Classifications are used to determine which athletes should be grouped together. In adapted sports, classification is based on function (e.g., strength, how many limbs are affected by injury, range of movement, tone/spasticity). This is similar to categorizing by age, gender, or weight in able-bodied sports.
Precautions when trying new sports
While trying out new sports can be fun and exciting, skin health is an important consideration. Trialing new sports is often associated with trying new equipment. When trying new equipment, it is important to check for red marks or pressure spots on your skin including your seat and any area of the body positioned against equipment (e.g., footrest or frame). People will commonly use the cushion from their everyday chair in their sport chair when they first try a sport. However, it is important to remember that although it is the same cushion, you may be sitting in a different position (e.g., seat angle) which will change pressure and potential forces from rubbing. The best approach is like that of trialing a new wheelchair or cushion: frequently check your skin in the early days of your new sport. This means that it is best to start with shorter sessions and work your way up in time once you know that your skin can tolerate the new equipment and positions. In water sports such as kayaking, or in rainy conditions for outdoor sports, make sure to check your skin when you are done since being wet can make the skin more prone to injury.
Additionally, you may want to consider the influence of temperature (extreme hot or cold weather), as temperature regulation may be impaired with an SCI.
Refer to our article on Pressure Injuries for more information!
Handcycles are a type of bicycle that is propelled by the arms instead of the legs. There are different types of handcycles available for all levels of ability. In general, most arm-cycles have alternative handle options for those with limited hand function.
Types of arm cycles
Recumbent cycles
Recumbent arm-cycles are three wheeled bikes that are controlled with the arms while seated in a reclined position. This type of bicycle has support straps to rest the feet in while cycling.
 Upright cycles
Upright cycles
Upright cycles are similar to recumbent bikes in that the feet are on either side of the front wheel. However, the user is seated in a more upright position when using this bike.
 Tandem bikes
Tandem bikes
A variety of tandem arm bikes are available. Bike models are available to allow riders to either ride beside each other, or one in front of the other. Power-assist versions are also available for those who may have some function in their legs.
 Arm cycle add-ons
Arm cycle add-ons
Instead of buying a separate wheelchair, arm-cycle add-ons are available for manual wheelchair users. These add-ons connect to the front of a manual wheelchair, lifting up the casters. This then allows an individual to propel their wheelchair via an arm cycle. Additionally, power-assist versions are available for those with less upper body strength.
Off-road wheelchairs
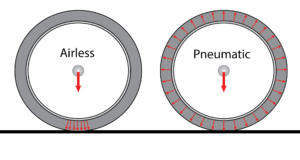
 If you are looking to go on some trails, an off-road wheelchair may appeal to you. These wheelchairs are used for recreational riding, such as going for a hike, or going fishing. Off-road wheelchairs often have larger, knobbier tires that are meant to withstand the trail, roots, and rocks. Like the arm-cycles, off-road wheelchairs come in a variety of set ups. Some setups may look like a typical manual wheelchair, but with larger wheels. There are also ones that are controlled with push-levers (such as the mountain trike), and powered wheelchairs with more power, suspension, and agility (such as the x5 frontier, and the x8-extreme all-terrain wheelchair).
If you are looking to go on some trails, an off-road wheelchair may appeal to you. These wheelchairs are used for recreational riding, such as going for a hike, or going fishing. Off-road wheelchairs often have larger, knobbier tires that are meant to withstand the trail, roots, and rocks. Like the arm-cycles, off-road wheelchairs come in a variety of set ups. Some setups may look like a typical manual wheelchair, but with larger wheels. There are also ones that are controlled with push-levers (such as the mountain trike), and powered wheelchairs with more power, suspension, and agility (such as the x5 frontier, and the x8-extreme all-terrain wheelchair).
Wheelchair racing

 For those who are interested in competition, wheelchair racing may be an option. Wheelchair race events range from the 100m, 200m, 400m, 800m, 1500m, and 5k distance races in track and field, to marathons. Racing wheelchairs differ from the wheelchairs and cycles listed above in that they typically have two wheels with a third one extended out in front. Ideally, race chairs should be light-weight to enhance performance. When seated, the wheelchair should fit “like a glove”, and there should be little movement in the seat. Unlike arm-cycles, the feet are bent down and kept closer to the body. In addition, specialized rubber gloves are worn to push the rims during races.
For those who are interested in competition, wheelchair racing may be an option. Wheelchair race events range from the 100m, 200m, 400m, 800m, 1500m, and 5k distance races in track and field, to marathons. Racing wheelchairs differ from the wheelchairs and cycles listed above in that they typically have two wheels with a third one extended out in front. Ideally, race chairs should be light-weight to enhance performance. When seated, the wheelchair should fit “like a glove”, and there should be little movement in the seat. Unlike arm-cycles, the feet are bent down and kept closer to the body. In addition, specialized rubber gloves are worn to push the rims during races.
Refer to our article on Wheelchair Propulsion Assist Devices for more information!
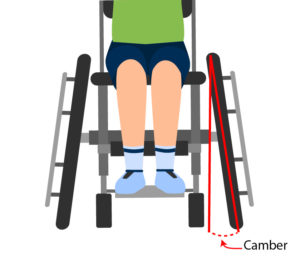
Tennis
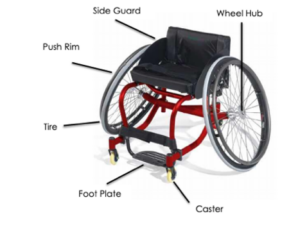 Wheelchair tennis is played on the same court as able-bodied tennis, and with similar rules. One rule difference is that in wheelchair tennis, players are allowed two bounces instead of one, and the second bounce can be anywhere – even out of bounds. Although one can play wheelchair tennis in their day chair, tennis wheelchairs are often preferred during play. These wheelchairs are faster, lighter, more agile, and more stable. The wheels on the wheelchair are also angled (i.e., there is more camber ) to allow for more swift turning. For those with limited hand function, taping the racquet to your hand is common practice, though it can take some time to find the optimal tension for you. Therefore, people with all levels of ability can play wheelchair tennis.
Wheelchair tennis is played on the same court as able-bodied tennis, and with similar rules. One rule difference is that in wheelchair tennis, players are allowed two bounces instead of one, and the second bounce can be anywhere – even out of bounds. Although one can play wheelchair tennis in their day chair, tennis wheelchairs are often preferred during play. These wheelchairs are faster, lighter, more agile, and more stable. The wheels on the wheelchair are also angled (i.e., there is more camber ) to allow for more swift turning. For those with limited hand function, taping the racquet to your hand is common practice, though it can take some time to find the optimal tension for you. Therefore, people with all levels of ability can play wheelchair tennis.
 Basketball
Basketball
Wheelchair basketball is played on a standard basketball court. The wheelchair used for basketball is one with wheels angled to 15-20 degrees and a single rollerblade used for a caster at the back. In addition, there are many strapping options to promote stability and safety, or to hold the body in a certain position. Commonly strapped body parts include the hips, knees, feet and/or ankles. It is common for wheelchair basketball leagues to include able bodied participants at the local level of competition. This allows for more players and teams for great league play.
Rugby
 Wheelchair rugby was developed specifically for people with tetraplegia and has grown to include people without SCI but with similar functional abilities (e.g., some impaired arm and hand function in addition to impaired leg function). Wheelchair rugby is played with a volleyball. The goal of the game is to carry the ball over the other team’s goal line. Unlike able-bodied rugby, wheelchair rugby is played indoors on a court. Specialized wheelchairs are used to play wheelchair rugby and can be separated into chairs for offensive players and chairs for defensive players. Offensive wheelchairs are set up for speed and mobility and are distinguished with a front bumper to prevent other chairs from hooking them. Often, offensive chairs are used by players with more function. On the other hand, defensive wheelchairs are set up with a bumper to hook and hold onto other players. Defensive chairs are often used by players with less function. Additional equipment used in rugby include straps and gloves. Straps are used on the waist (to compensate for a lack of core muscles), the thighs (to prevent them from falling to the side or from shifting side to side), and the feet (for comfort). Meanwhile, gloves work to protect the skin, add extra grip when pushing the chair, and to making throwing and catching the ball easier.
Wheelchair rugby was developed specifically for people with tetraplegia and has grown to include people without SCI but with similar functional abilities (e.g., some impaired arm and hand function in addition to impaired leg function). Wheelchair rugby is played with a volleyball. The goal of the game is to carry the ball over the other team’s goal line. Unlike able-bodied rugby, wheelchair rugby is played indoors on a court. Specialized wheelchairs are used to play wheelchair rugby and can be separated into chairs for offensive players and chairs for defensive players. Offensive wheelchairs are set up for speed and mobility and are distinguished with a front bumper to prevent other chairs from hooking them. Often, offensive chairs are used by players with more function. On the other hand, defensive wheelchairs are set up with a bumper to hook and hold onto other players. Defensive chairs are often used by players with less function. Additional equipment used in rugby include straps and gloves. Straps are used on the waist (to compensate for a lack of core muscles), the thighs (to prevent them from falling to the side or from shifting side to side), and the feet (for comfort). Meanwhile, gloves work to protect the skin, add extra grip when pushing the chair, and to making throwing and catching the ball easier.
Community Voices: Byron |
Alpine Skiing

 Alpine skiing, also known as downhill skiing, is a sport that individuals with tetraplegia and paraplegia can partake in with the use of sit-skis. In general, sit skis have a bucket-type of seat with an adjustable seat and footrest. To create a smoother ride, sit-skis have additional features such as suspensions and a shock compression system under the seat. The seat and suspension/shock systems are all connected to either a single ski (mono-ski) or a pair of skis (bi-skis). In general, mono-skis require the user to have good upper body strength, and the ability to ski independently. Bi-skis are often used by individuals who may require some assistance. Often, bi-skis are used with an able-bodied individual who skis behind them. Skiers who use a sit-ski can use the typical chairlifts at the mountains and with experience, can access all terrains of ski areas.
Alpine skiing, also known as downhill skiing, is a sport that individuals with tetraplegia and paraplegia can partake in with the use of sit-skis. In general, sit skis have a bucket-type of seat with an adjustable seat and footrest. To create a smoother ride, sit-skis have additional features such as suspensions and a shock compression system under the seat. The seat and suspension/shock systems are all connected to either a single ski (mono-ski) or a pair of skis (bi-skis). In general, mono-skis require the user to have good upper body strength, and the ability to ski independently. Bi-skis are often used by individuals who may require some assistance. Often, bi-skis are used with an able-bodied individual who skis behind them. Skiers who use a sit-ski can use the typical chairlifts at the mountains and with experience, can access all terrains of ski areas.
 Cross Country Skiing
Cross Country Skiing
Cross country skiing (which is a type of Nordic skiing) allows individuals with paraplegia and tetraplegia to explore snowy trails. Like the alpine skis, cross country skis consist of a bucket seat that connects to a metal frame, which clips into the skis. Cross country skiers also often use poles while skiing to propel themselves along flatter terrain. If assistance is required, an able-bodied person can help push the ski forward with their ski-pole using an adaptive add-on.
 Sledge (Ice) Hockey
Sledge (Ice) Hockey
Sledge hockey, or para ice hockey is identical to ice hockey but is played while sitting in sledges as opposed to standing on skates.
A sledge consists of a plastic bucket-shaped seat that is connected to a metal frame. This frame is set on two adjustable skate blades, with the blades aligned on the bottom of the seat. The skate blades may be adjusted so that they are further apart for stability (good for new players) or can be moved closer together to allow for more maneuverability and speed. Straps are available to help keep the feet, knees, and hips in place. Players propel themselves in the sledge using two sticks. These sticks are dual ended: one end has a blade for handling the puck, while the other end has a metal pick in it to help players propel themselves across the ice. Typical hockey pads are used for safety during play.
Sailing
Adapted sailing is a sport that people of all abilities can participate in. Common features of adapted sailboats include handguards along the side of the boats, greater deck space due to removed masts, and customized molded seats with back support and belts that pivot. For individuals with reduced function, other available adaptations include electronic controls (such as the use of a joystick), and sip ‘n’ puff technology to steer the boat with breath. Many sailing clubs have power/mechanical lifts dockside to assist with transfers into boats.
|
Kayaking

 Kayaks are available for people with all levels of SCI. While individuals with a lower level of injury may use non-adapted kayaks, adaptations are available for comfort and to accommodate those with limited function. Some kayaks may have custom seating with side and abdominal support. These supports are cushioned to protect the skin while kayaking. Stabilizing outriggers are available to increase stability of the boat and to reduce the chances of tipping. For those with limited arm/hand function, there are various adaptations for the paddle including:
Kayaks are available for people with all levels of SCI. While individuals with a lower level of injury may use non-adapted kayaks, adaptations are available for comfort and to accommodate those with limited function. Some kayaks may have custom seating with side and abdominal support. These supports are cushioned to protect the skin while kayaking. Stabilizing outriggers are available to increase stability of the boat and to reduce the chances of tipping. For those with limited arm/hand function, there are various adaptations for the paddle including:
- A back of the hand grip, which places more paddling pressure on the arms instead of the hands.
- Wrist cuff adaptation, which allows individuals to connect the paddle to their wrists via a cuff.
There are many benefits to staying physically active after SCI and there is a large variety of sports to participate in. Whether you prefer staying on land, floating on water, or being in the snow, most sports have been adapted in some way or another so that all who want to can participate! Prior to trying a sport, talk with your health providers to ensure that you are in a condition to play.
Evidence for “Why be physically active after SCI” is based on:
Martin KA, Latimer AE, Francoeur C, Hanley H. Sustaining exercise motivation and participation among people with spinal cord injuries – Lessons learned from a 9 month intervention. Palaestra 2002;18(1):38-51.
Hicks AL, Martin KA, Ditor DS, Latimer AE, Craven C, Bugaresti J et al. Long-term exercise training in persons with spinal cord injury: effects on strength, arm ergometry performance and psychological well-being. Spinal Cord 2003;41(1):34-43.
Latimer AE, Ginis KA, Hicks AL, McCartney N. An examination of the mechanisms of exercise- induced change in psychological well-being among people with spinal cord injury. J Rehabil Res Dev 2004;41(5):643-652.
Martin Ginis KA, Latimer AE, McKechnie K, Ditor DS, Hicks AL, Bugaresti J. Using exercise to enhance subjective well-being among people with spinal cord injury: The mediating influences of stress and pain. REHABIL PSYCHOL 2003;48(3):157-164.
Latimer AE, Martin Ginis KA, Hicks AL. Buffering the effects of stress on well-being among individuals with spinal cord injury: A potential role for exercise. Therapeutic Recreation Journal 2005;39(2):131-138.
Mulroy, S. J., Thompson, L., Kemp, B., Hatchett, P. P., Newsam, C. J., Lupold, D. G., et al. (2011). Strengthening and Optimal Movements for Painful Shoulders (STOMPS) in chronic spinal cord injury: a randomized controlled trial. Physical Therapy, 91, 305—324.
Jacobs, P. L. (2009). Effects of resistance and endurance training in persons with paraplegia. Medicine & Science in Sports & Exercise, 41, 992-997.
De Groot PC, Hjeltnes N, Heijboer AC, Stal W, Birkeland K. Effect of training intensity on physical capacity, lipid profile and insulin sensitivity in early rehabilitation of spinal cord injured individuals. Spinal Cord 2003;41(12):673-679.
de Carvalho DC, Martins CL, Cardoso SD, Cliquet A. Improvement of metabolic and cardiorespiratory responses through treadmill gait training with neuromuscular electrical stimulation in quadriplegic subjects. Artif Organs 2006;30(1):56-63.
Information for “What are adapted sports” is based on:
World Para Athletes. (n.d.). What is classification? https://www.paralympic.org/athletics/classification
Information for “What types of cycling and pushing sports are there?” is based on:
World Para Athletes. (n.d.). Para-athletics explained: Wheelchair racing. https://www.paralympic.org/news/para-athletics-explained-wheelchair-racing
Chair Institute. (2019). Best off road all terrain wheelchairs for outdoors review 2020. https://chairinstitute.com/best-wheelchairs-for-outdoors/
Information for “What adapted court sports are available?” is based on:
BC Wheelchair Sports. (n.d.). Wheelchair Tennis.https://www.bcwheelchairsports.com/sites/default/files/images/BCWSA%20Wheelchair%20Tennis%20First%20Introduction%20Manual%20-%20PRINT%20%281%29.pdf
Wheelchair Basketball Canada. (2021). About the sport. https://www.wheelchairbasketball.ca/the-sport/about-the-sport/
Wheelchair Basketball Canada. (2021). Equipment. https://www.wheelchairbasketball.ca/the-sport/equipment/
Wheelchair Rugby Canada. (2018). Rules and equipment. https://wheelchairrugby.ca/rules-equipment/
Information for “What adapted winter sports are available?” is based on:
Canadian Ski Council. (2018). Skiing is for everyone! https://www.skicanada.org/ready/accessible-skiing-information/
XCSkiResorts. (2016). Nordic adaptive sit-skis bring freedom to mobility impaired persons. https://www.xcskiresorts.com/resort-features/2016/9/12/nordic-adaptive-sit-skis-bring-freedom-to-mobility-impaired-persons
BC Hockey – Saanichton, BC. (2016). Para Hockey Brochure Guide.https://www.bchockey.net/Files/Sledge%20Hockey%20Brochure.pdf
Information for “What water sports are available?” is based on:
Move United. (n.d.). Sailing. https://www.moveunitedsport.org/sport/sailing/
Disabled Sailing Association of British Columbia. (2021). Sip ‘n’ Puff Technology. https://asabc.org/sip-n-puff/
Creating Ability. (2021). Seating systems. https://www.creatingability.com/seating-systems/
Creating Ability. (2021). Paddle adaptations. https://www.creatingability.com/paddle-adaptations/
Image credits
- Man on Arm Erg by SCIRE Community
- BC Wheelchair Rugby Day 1 293©Melissa Nemeth, CC BY-SA 2.0
- Noun Project
- Noun Project
- Noun Project
- Shark ©Sunrise Medical 2021
- Replacement parts for Invacare Top End Handcycles ©RehabMart.com, LLC 1998-2021
- Van Ram Fun2Go Tandem ©Bike-On.com 2020
- Batec Hybrid ©Batec Mobility
- Invacare top end crossfire all terrain wheelchair ©Invacare Corporation 2021
- Top end preliminator youth racing wheelchair – custom version. ©How I Roll Sports, LLC 2018
- Harness Glove ©Harness Designs Wheelchair Gloves
- Wheelchair Tennis ©BC Wheelchair Sports
- Wigan Warthogs Wheelchair Basketball-2 ©Andrew Spillane, CC BY-ND 2.0
- Equipment ©International Wheelchair Rugby Federation 2013-2021
- London 2012 Paralympics Wheelchair Rugby (Murderball) ©Sum_of_Marc, CC BY-NC-ND 2.0
- Monique-1 Mono Ski ©Enabling Technologies 2021
- Dynamique Bi Ski ©Enabling Technologies 2021
- Woman using sit ski – photo by northeast passage ©U.S. Forest Service – Pacific Northwest Region, Public Domain Mark 1.0
- Sledge Hockey: Italy/Sweden ©Mariska Richters, CC BY-NC-SA 2.0
- Terry in Matin 16
- Outfitted Kayak ©Creating Ability 2021
- Stabilizing Outriggers ©Creating Ability 2021

 Athlete Classification
Athlete Classification
 Upright cycles
Upright cycles Tandem bikes
Tandem bikes Arm cycle add-ons
Arm cycle add-ons Basketball
Basketball
 Cross Country Skiing
Cross Country Skiing Sledge (Ice) Hockey
Sledge (Ice) Hockey Community Voices: Terry
Community Voices: Terry In the body, there are 2 main types of muscle fibers: slow twitch (type I) and fast twitch (type II). Slow twitch muscles are known as the endurance muscles, as they are able to hold a contraction for a long period of time before getting tired. For example, the muscles that are used to keep your head upright are mostly made up of slow twitch muscle fibers. Type II fibers are known for their short burst of speed or strength. They can generate more strength, but get tired really quickly. Over time with an SCI, the muscles with the endurance type (type I) tend to turn into the more fatigable type (type II). There is some moderate-weak evidence that shows that among those with limited movement in their legs, the use of
In the body, there are 2 main types of muscle fibers: slow twitch (type I) and fast twitch (type II). Slow twitch muscles are known as the endurance muscles, as they are able to hold a contraction for a long period of time before getting tired. For example, the muscles that are used to keep your head upright are mostly made up of slow twitch muscle fibers. Type II fibers are known for their short burst of speed or strength. They can generate more strength, but get tired really quickly. Over time with an SCI, the muscles with the endurance type (type I) tend to turn into the more fatigable type (type II). There is some moderate-weak evidence that shows that among those with limited movement in their legs, the use of  There is strong-moderate evidence that exercising can help individuals of any injury level improve their strength. Among those with
There is strong-moderate evidence that exercising can help individuals of any injury level improve their strength. Among those with 
 Some evidence suggests that exercise can help individuals improve perceptions of well-being. Well-being has been defined as how well an individual feels in their mind, their satisfaction with their health and functioning, and their overall satisfaction in life. Two aspects of well-being that are relatively well-researched are the impact of physical activity on depression and
Some evidence suggests that exercise can help individuals improve perceptions of well-being. Well-being has been defined as how well an individual feels in their mind, their satisfaction with their health and functioning, and their overall satisfaction in life. Two aspects of well-being that are relatively well-researched are the impact of physical activity on depression and 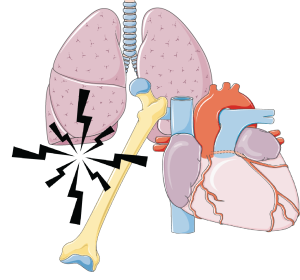 Conditions impacting the heart and blood vessels, by improving the strength of the heart and balancing out the sympathetic (fight or flight; stimulation) and parasympathetic (relax and slowing) nervous systems,
Conditions impacting the heart and blood vessels, by improving the strength of the heart and balancing out the sympathetic (fight or flight; stimulation) and parasympathetic (relax and slowing) nervous systems, There are many ways for you to remain physically active, even after SCI! Strength training can be done at a local community center or private gym, most often with the equipment already there. Strength training can also be done at home with free weights and exercise bands. Some equipment that can be used for strength training include free weights, exercise bands, and pulleys. For aerobic exercise, some alternatives include using an arm ergometer (arm cycle), a rowing machine (if possible), and adaptive rowers, such as the Ski-Erg.
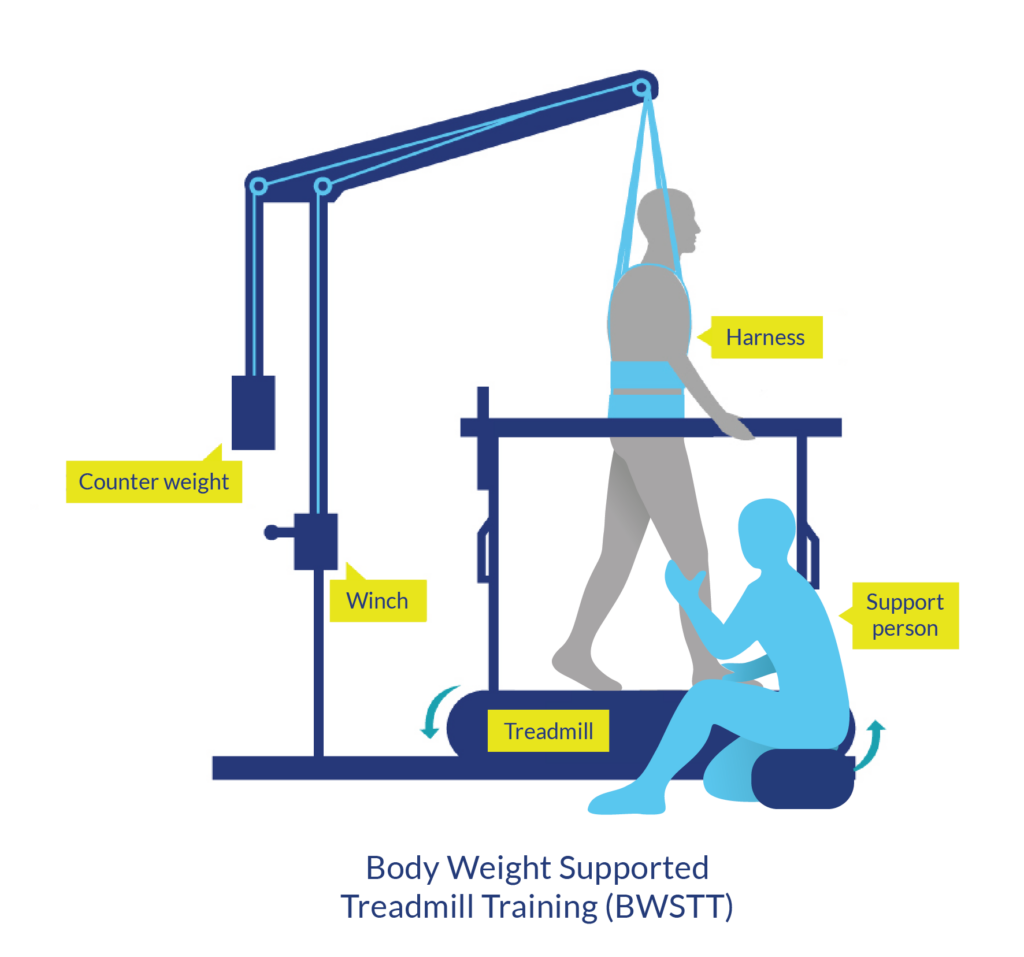
There are many ways for you to remain physically active, even after SCI! Strength training can be done at a local community center or private gym, most often with the equipment already there. Strength training can also be done at home with free weights and exercise bands. Some equipment that can be used for strength training include free weights, exercise bands, and pulleys. For aerobic exercise, some alternatives include using an arm ergometer (arm cycle), a rowing machine (if possible), and adaptive rowers, such as the Ski-Erg. Alternatively, specialty equipment is available to help facilitate exercise after SCI. However, this equipment is more commonly used in rehabilitation settings, as they are very expensive and additional assistance is often required. A Functional Electrical Stimulation (FES) bike can be used to simulate the legs while cycling, and has been shown improve strength and endurance. Body-weight Support Treadmills are specialized treadmills with a sling attached. This type of treadmill allows an individual to move their legs on the treadmill, while having their bodyweight supported by a sling. Some models are available to allow users to control how much of their bodyweight they feel while in the treadmill, which can alter the challenge of walking.
Alternatively, specialty equipment is available to help facilitate exercise after SCI. However, this equipment is more commonly used in rehabilitation settings, as they are very expensive and additional assistance is often required. A Functional Electrical Stimulation (FES) bike can be used to simulate the legs while cycling, and has been shown improve strength and endurance. Body-weight Support Treadmills are specialized treadmills with a sling attached. This type of treadmill allows an individual to move their legs on the treadmill, while having their bodyweight supported by a sling. Some models are available to allow users to control how much of their bodyweight they feel while in the treadmill, which can alter the challenge of walking.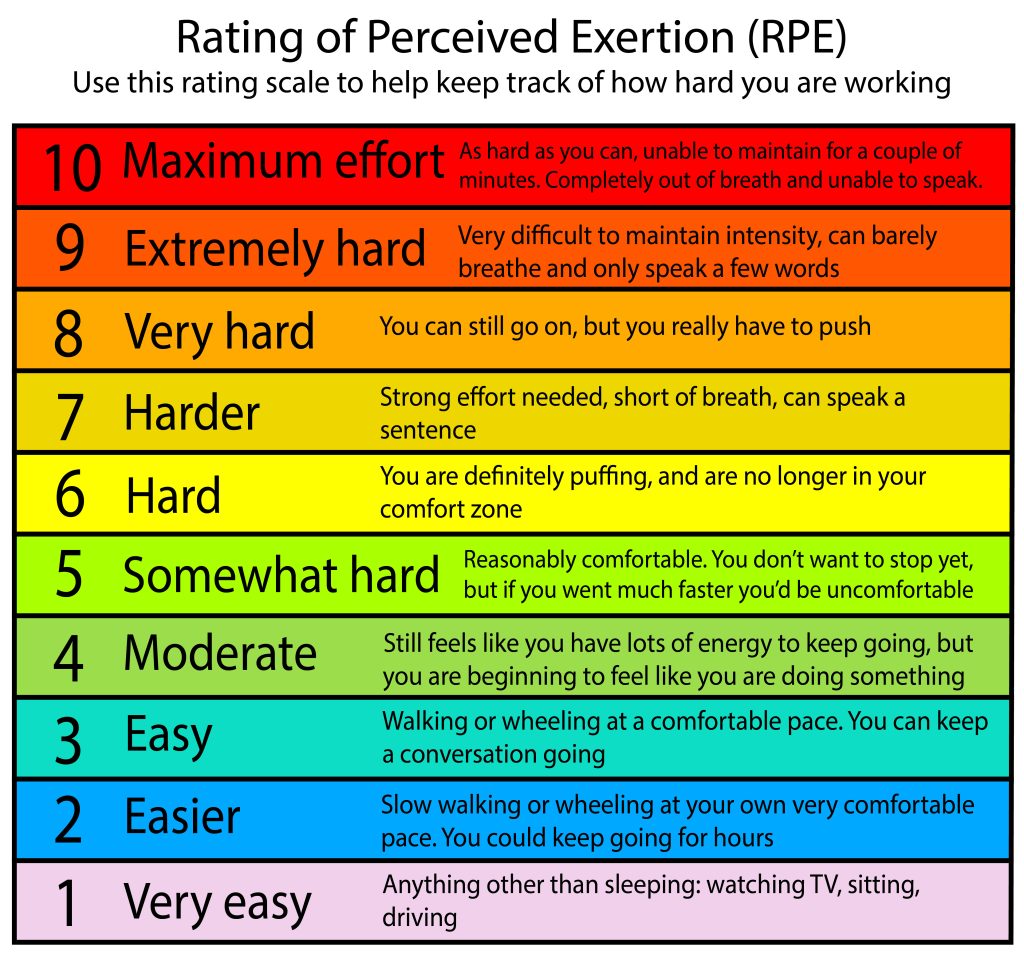 The advance level provides guidelines for additional fitness and health benefits, such as reducing your risk for diabetes. It is recommended to get at least 30 minutes of moderate to vigorous intensity aerobic exercise at least 3 times a week, in addition to the 3 sets of strength exercises twice a week.
The advance level provides guidelines for additional fitness and health benefits, such as reducing your risk for diabetes. It is recommended to get at least 30 minutes of moderate to vigorous intensity aerobic exercise at least 3 times a week, in addition to the 3 sets of strength exercises twice a week.




 When you first start exercising, it is common to possibly feel some nausea, or like you might pass out. This is a result of exercise-induced (exertional) hypotension, or a sudden drop in blood pressure due to exercise. One way to overcome this is to build up your exercise routine. When doing aerobic exercises, try a discontinuous approach: exercise for 2-3 minutes, then take a break. The idea is to slowly increase the length of exercising before you require a break, working your way up to 20-30 minutes of exercise. Once you are able to continuously exercise for 20-30 minutes, then you may consider increasing the resistance.
When you first start exercising, it is common to possibly feel some nausea, or like you might pass out. This is a result of exercise-induced (exertional) hypotension, or a sudden drop in blood pressure due to exercise. One way to overcome this is to build up your exercise routine. When doing aerobic exercises, try a discontinuous approach: exercise for 2-3 minutes, then take a break. The idea is to slowly increase the length of exercising before you require a break, working your way up to 20-30 minutes of exercise. Once you are able to continuously exercise for 20-30 minutes, then you may consider increasing the resistance.
 With a high level injury, temperature dysregulation, the body’s inability to control temperature, may be influenced. The ability to produce sweat can be compromised with higher levels of injury, resulting in an inability to cool down the body. In colder environments, it may be harder to warm up.
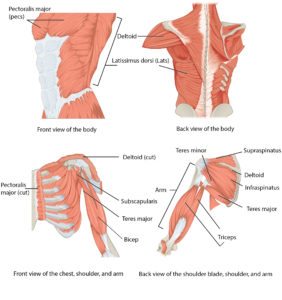
With a high level injury, temperature dysregulation, the body’s inability to control temperature, may be influenced. The ability to produce sweat can be compromised with higher levels of injury, resulting in an inability to cool down the body. In colder environments, it may be harder to warm up. Overuse injuries occur when you exercise muscles that are already often used on a daily/frequent basis. An example of this is the shoulders, as it is used for pushing a wheelchair. To prevent overuse injury, make sure you have the correct posture when performing exercises. When working on the shoulder, try to consider alternatives to pushing your wheelchair as exercise, if possible. For example, the use of an arm bike could be an alternative to get around as they require less demand on your shoulders and arms. In addition, try to balance aerobic exercise and strength training in muscle groups prone to overuse injuries.
Overuse injuries occur when you exercise muscles that are already often used on a daily/frequent basis. An example of this is the shoulders, as it is used for pushing a wheelchair. To prevent overuse injury, make sure you have the correct posture when performing exercises. When working on the shoulder, try to consider alternatives to pushing your wheelchair as exercise, if possible. For example, the use of an arm bike could be an alternative to get around as they require less demand on your shoulders and arms. In addition, try to balance aerobic exercise and strength training in muscle groups prone to overuse injuries.


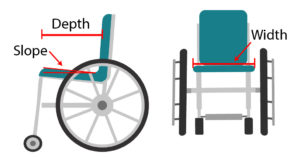
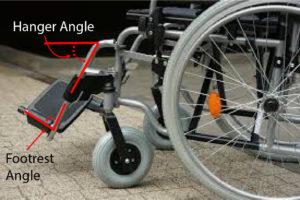
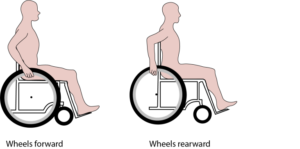
 Folding wheelchairs are designed to be folded vertically and take up minimal storage space. This allows for easy portability (such as fitting the wheelchair into a car). However, these wheelchairs also have many moving parts that may break down or loosen over time, and are heavier than rigid wheelchairs. Folding wheelchair often have flip up, swing away or swing in footrests so they may be used by individuals that do not use the wheelchair full time, can stand or take some steps, or by those who foot propel.
Folding wheelchairs are designed to be folded vertically and take up minimal storage space. This allows for easy portability (such as fitting the wheelchair into a car). However, these wheelchairs also have many moving parts that may break down or loosen over time, and are heavier than rigid wheelchairs. Folding wheelchair often have flip up, swing away or swing in footrests so they may be used by individuals that do not use the wheelchair full time, can stand or take some steps, or by those who foot propel.


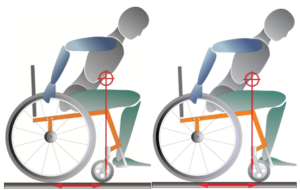



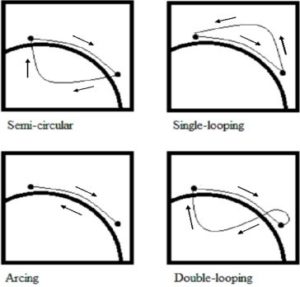 Propulsion pattern: the pattern you push your wheelchair with (e.g., where do your hands go when you push and after you’re done pushing) may also have an influence on your risk of injury. Some weak evidence suggests that using the semi-circular and double-loop-over may reduce the risk of nerve injury and are the most optimal ways to push your wheelchair. Further evidence (weak) has indicated that arcing may be more efficient for short bouts of high intensity pushing (like when going uphill).
Propulsion pattern: the pattern you push your wheelchair with (e.g., where do your hands go when you push and after you’re done pushing) may also have an influence on your risk of injury. Some weak evidence suggests that using the semi-circular and double-loop-over may reduce the risk of nerve injury and are the most optimal ways to push your wheelchair. Further evidence (weak) has indicated that arcing may be more efficient for short bouts of high intensity pushing (like when going uphill).
 Dutch
Dutch English
English German
German Indonesian
Indonesian Italian
Italian Korean
Korean Persian
Persian Spanish
Spanish Swedish
Swedish
 A group led by Dr. Kathleen Martin Ginis at the University of British Columbia and Dr. Victoria Goosey-Tolfrey at Loughborough University, UK developed international guidelines on exercise after SCI. The process of developing these guidelines involved a systematic review of relevant literature, consensus meetings, stakeholder feedback, and a formal audit of the process.
A group led by Dr. Kathleen Martin Ginis at the University of British Columbia and Dr. Victoria Goosey-Tolfrey at Loughborough University, UK developed international guidelines on exercise after SCI. The process of developing these guidelines involved a systematic review of relevant literature, consensus meetings, stakeholder feedback, and a formal audit of the process.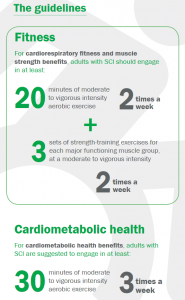

 If you are not already exercising, it is okay to start with smaller amounts of exercise and gradually increase duration, frequency, and intensity, as a progression toward meeting the guidelines. Doing exercise below the recommended levels may or may not bring small changes in fitness or cardiometabolic health.
If you are not already exercising, it is okay to start with smaller amounts of exercise and gradually increase duration, frequency, and intensity, as a progression toward meeting the guidelines. Doing exercise below the recommended levels may or may not bring small changes in fitness or cardiometabolic health. Exceeding these exercise guidelines would be expected to yield additional cardiorespiratory fitness and muscle strength and cardiometabolic health benefits. However, there are insufficient data to comment on the risks associated with a person with SCI exceeding these guidelines.
Exceeding these exercise guidelines would be expected to yield additional cardiorespiratory fitness and muscle strength and cardiometabolic health benefits. However, there are insufficient data to comment on the risks associated with a person with SCI exceeding these guidelines.











 There are some situations in which
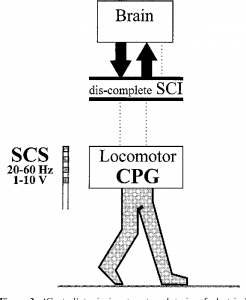
There are some situations in which  Studies have shown that both FES arm exercise and FES cycling helps to maintain or improve strength after SCI. However, FES cycling may be more effective for maintaining strength after injury than improving strength that has already been lost. This is supported by
Studies have shown that both FES arm exercise and FES cycling helps to maintain or improve strength after SCI. However, FES cycling may be more effective for maintaining strength after injury than improving strength that has already been lost. This is supported by  Fifteen studies have looked at FES for improving many different aspects of fitness after SCI. Taken altogether, these studies provide
Fifteen studies have looked at FES for improving many different aspects of fitness after SCI. Taken altogether, these studies provide  Although it is commonly thought that increased muscle bulk from FES will reduce the risk of pressure sores, there are not very many studies which have looked at whether this actually happens. One study provides
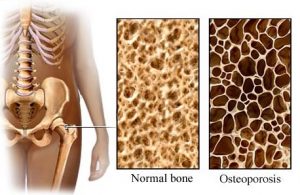
Although it is commonly thought that increased muscle bulk from FES will reduce the risk of pressure sores, there are not very many studies which have looked at whether this actually happens. One study provides  Research studies show that FES cycling does not prevent bone loss after SCI (
Research studies show that FES cycling does not prevent bone loss after SCI (