Author: SCIRE Community Team | Reviewer: Susan Andrews | Published: 3 November 2017 | Updated: ~
Key Points
- A pressure injury (or pressure ulcer, wound, or sore) is damage to the skin and underlying tissues caused by pressure, friction, or shear. Pressure injuries are common on weight-bearing areas of the body like the sit bones and tailbone.
- Pressure injuries are a common complication of SCI that can have serious consequences including reduced independence and life-threatening infections.
- People with SCI are at greater risk of developing pressure injuries because of changes to the body and how it is used after SCI.
- Preventing pressure injuries is very important and involves checking the skin regularly, pressure relief, staying healthy, and early treatment of potential injuries.
- The most important factor in treating a pressure injury is identifying and removing the cause of the injury.
- Pressure injuries are treated using several treatments, including wound care and dressings, medications, electrical and light stimulation, debridement, and surgery.
A pressure injury (also known as pressure wound, pressure ulcer or bed sore) is a breakdown of the skin and the tissues under the skin that is caused by pressure, friction, or shear.
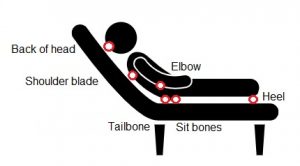
Pressure injuries are a common complication of SCI that happens because of changes to the body and how it is used after the injury. Pressure injuries usually happen on areas of the body that bear weight in sitting or lying, such as the sit bones, tailbone, heels, back of the knees, elbows, and shoulder blades.
Pressure injuries are common
Pressure injuries are common after SCI. They can affect as many as one third of people with SCI each year and almost every person with an SCI experiences at least one pressure injury in their lifetime. The risk of pressure injuries increases over time when living with an SCI long-term.
Pressure injuries can have serious consequences

Pressure injuries can have serious consequences for health, function, and quality of life, including:
- Difficult and lengthy healing
- Infections, including severe infections that lead to a life-threatening condition called sepsis
- Long and costly hospital stays and re-hospitalizations
- Reduced independence and mobility during healing
- Inability to participate in work and school during healing
- Reduced life satisfaction and quality of life
- A greater need for assistance from caregivers and family during healing
Prevention is essential to reduce risk
The best management for pressure injuries is prevention. In fact, many pressure injuries are preventable through a combination of good self-care, staying healthy, and regular check-ins with your health team. It is essential to learn how to recognize, prevent, and treat pressure injuries as soon as possible after SCI to help reduce your risk.
Find out what advice Josh has on pressure sores and routines you can follow to avoid them.
Pressure injuries happen because of many different factors from both inside and outside the body. There are a number of changes to the body after SCI that make pressure injuries more likely. These factors, combined with forces like pressure, friction, and shear, can cause pressure injury.
Pressure
Pressure injuries usually form on weight-bearing areas of the body that are in contact with supporting surfaces. This usually happens when sitting or lying in the same position for a long time or when positioned on a surface that does not support the weight properly (such as a hard chair).
Pressure usually happens in specific areas depending on the position, but most often affects the sit bones (ischial tuberosities), tailbone (sacrum and coccyx), heels, backs of the knees, elbows, back of the head, and shoulder blades.
Too much pressure can prevent blood from reaching the area, which is important for bringing oxygen and nutrients to the tissues. This can lead to skin damage or breakdown. Skin breakdown can happen quite quickly (in even 30 to 60 minutes) on a hard surface without changing positions regularly.
Friction and shear
Pressure injuries can also be caused by friction and shear. Friction can happen when the skin is rubbed on a course surface, such as sitting on an uneven wrinkle of clothing or rough surface. This can cause injury to the surface of the skin which can lead to skin breakdown.
Shear is a type of force where the skin goes one way and the body goes the opposite direction. This usually happens when the skin is caught on a surface while the body is moved. For example, when transferring in bed, the skin might be pulled along the bed while the person shifts positions, which causes shear. Shear strains and injures the tissues close to the bone.
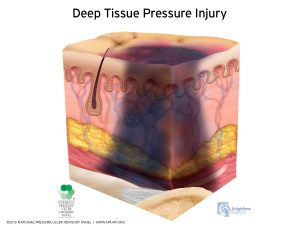
Most pressure injuries result from combinations of pressure, friction, and shear that happen in the deep tissues close to the bone. This leads to deep tissue injury, rather than injury on the skin’s surface.
There are many other factors from both inside and outside the body after SCI that make pressure injuries more likely to develop.
Other factors that contribute to pressure injuries
Changes to the skin
Spinal cord injury can affect the skin in various ways. The skin below the injury may become less elastic and weaker as a result of tissue changes caused by the SCI. In addition, people with injuries above T6 lose the ability to sweat below the injury, which means that body temperature is not regulated very well.
Loss of sensation
Sensation is important because it allows us to recognize discomfort and provides a cue to change position regularly. When sensation is reduced or absent, these cues are not present and we may sit in an uncomfortable position where there is too much pressure for too long.
Loss of movement
Loss of movement also contributes to pressure injuries. People with reduced movement often use a wheelchair as their main method of mobility, which may lead to long periods of sitting in one position. It may also be more difficulty to reposition in sitting or lying so pressure may be placed in one area for too long. As well, when the muscles are not used regularly, they shrink (called muscle atrophy), which means there is less padding between the skin and bone.
Hear Peter speak about his difficulties with not having sensation to his elbows.
Moisture
Moisture makes the skin more vulnerable to injury and bacteria. Moisture may be present because of bladder or bowel problems after an SCI or in warm and humid climates.
Body weight
Changes to body weight, either being too thin or overweight, can increase the risk of pressure injuries. When a person is underweight, there is less padding between the skin and bone. When a person is overweight, the body is heavier, which creates more pressure in weight-bearing and can also make transfers more difficult, which may result in more shearing and friction.
Supporting surfaces
 The characteristics of surfaces that support the body in regular positions are very important for distributing pressure. This includes wheelchair cushions, mattresses, couch cushions, car seats, commode or toilet seats, sports equipment, and any other surface that is regularly used for supporting the body. Hard or unsupportive surfaces can contribute to developing pressure injuries. It is important to also consider surfaces in unfamiliar settings, such as when travelling or when a hospital visit is needed. Airplane seats and hospital stretchers do not often provide enough protection for your skin following SCI and you may need a lightweight travel cushion when travelling or to request a specialized surface if you need to visit a hospital.
The characteristics of surfaces that support the body in regular positions are very important for distributing pressure. This includes wheelchair cushions, mattresses, couch cushions, car seats, commode or toilet seats, sports equipment, and any other surface that is regularly used for supporting the body. Hard or unsupportive surfaces can contribute to developing pressure injuries. It is important to also consider surfaces in unfamiliar settings, such as when travelling or when a hospital visit is needed. Airplane seats and hospital stretchers do not often provide enough protection for your skin following SCI and you may need a lightweight travel cushion when travelling or to request a specialized surface if you need to visit a hospital.
Other factors:
- Reduced ability to fight infections (reduced immune function)
- Other medical conditions like infections, blood clots, spasticity and contractures
- Poor nutrition (especially if there is not enough calories or protein)
- Reduced physical activity
- Smoking
- Long periods of bed rest
- The sit bones (ischial tuberosities) may become flatter over time
- Higher level of injury and complete SCI
- Depression
- Reduced ability to perform behaviours that reduce risk, such as regular pressure relief, good skin care, and skin inspections
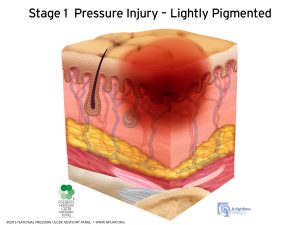
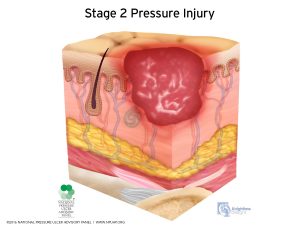
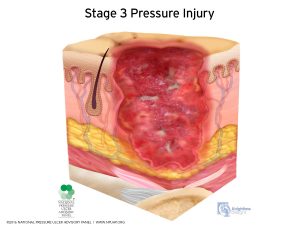
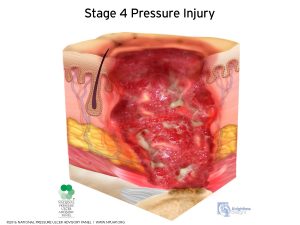
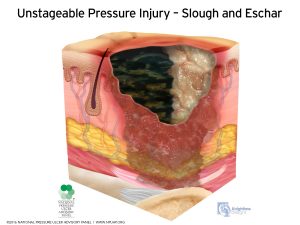
Pressure injuries are classified by how severe they are as “stages” of injury. These stages can range from just a small amount of redness on the skin to a wound that travels all the way down to the bone. Determining which stage a pressure injury is can help you and your health team to measure the extent of wounds and figure out how to treat it.
Stages of Pressure Injury (National Pressure Injury Advisory Panel)2
To identify a pressure injury early you need to check your skin once or twice daily using a mirror or with the help of a care provider.
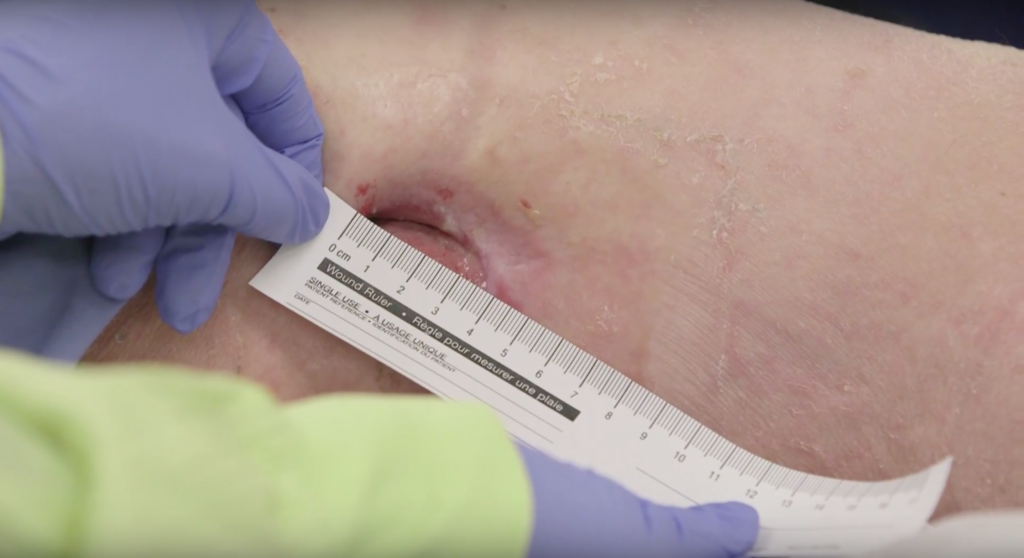
Physical examination
The main way that pressure injuries are diagnosed is with a visual skin check. Checking by feel is not enough, because it only identifies open areas that can be felt. Early pressure injury can be as simple as red or purple discoloration to the skin.
If there is an open wound you may need to be seen by a physician and referred to a nurse for a wound assessment. This may involve starting a treatment plan that should include trying to identify the cause of the pressure injury.
The nurse will observe the wound and take note of its appearance (such as its edges, colour, and shape) and look for signs of inflammation or infection. The nurse may take measurements of the length, width, and depth of the wound. These can help determine the stage of the wound and be used as a comparison as it heals. Sometimes, the nurse may take photos for assessment purposes. A swab of the pressure sore is only taken if infection is suspected. Infection is suspected if there has been increased redness, odour or drainage or if pain has increased if you have sensation.
It is often helpful to have an occupational therapist or physiotherapist involved to help figure out the cause of tissue damage.
Listen to Josh describe his experience of having a pressure sore he wasn’t aware of and how he overcame it with the help of a specialist.
Other testing
- Blood tests may be used to identify if there is an infection.
- Ultrasound is an imaging technique that may be used in some facilities. Ultrasound imaging uses sound waves to detect injuries deep within the skin. It may be used to detect suspected pressure injuries that are not easily seen.
Osteomyelitis (bone infection)
When pressure injuries are severe and reach all the way to the bone (stage 4), there is a risk of developing a serious bone infection called osteomyelitis. If your health team is concerned that you might have osteomyelitis, you may have additional testing such as x-rays, an MRI, or blood tests to diagnose this condition.
The most important part of managing pressure injuries is preventing them from happening in the first place. Many different techniques may be used to prevent pressure injuries. Some of these are a part of self-care and others involve working together with your health team.
Learning how to prevent pressure injuries
Early on in your care, your health providers will speak to you about how to prevent pressure injuries. This may be a part of one-on-one care or as a part of a group education class. Prevention education is a very important part of reducing risk. You will learn how to identify skin concerns early on and the best techniques for you to keep your skin healthy.
Maintaining good skin care
Regular skin care is an important part of preventing pressure injuries. Many of these techniques you will learn as a part of skincare education.
Regular skin checks
Checking the skin for changes in color and texture is important to recognize areas of risk and to identify any changes early. The main areas to check are bony areas, like the sit bones, tail bone, side of the hips, and heels. A mirror or assistance from a caregiver may be needed to check some areas. Any areas of redness, bruising, or injury should be discussed with your health providers immediately. Skin checks are recommended once or twice daily or after activities like prolonged bed rest or trying new equipment.
Listen to Peter describe how he regularly checks his elbows to maintain good skin health.
Keeping the skin healthy
 Regular skin care should be done using a gentle pH-balanced skin cleanser and moisturizer. The skin should always be treated gently and not rubbed or massaged forcefully The skin should be kept dry using loose fitting clothes made of light weight fabrics and protecting the skin from excess moisture. Avoid clothing with thick seams or pockets like denim that can contribute to tissue damage.
Regular skin care should be done using a gentle pH-balanced skin cleanser and moisturizer. The skin should always be treated gently and not rubbed or massaged forcefully The skin should be kept dry using loose fitting clothes made of light weight fabrics and protecting the skin from excess moisture. Avoid clothing with thick seams or pockets like denim that can contribute to tissue damage.
Regular pressure relief
Pressure relief techniques are positions and movements that remove pressure and give the tissues a chance to regain proper blood flow. You should discuss with your health providers about which positions are best for you and how often and for how long they should be done for. Keep in mind that moving into pressure relieving positions should not involve pulling or shearing of the skin while re-positioning.
Depending on your level of injury, some people are able to re-position themselves or need a small amount of assistance. People with higher level SCI can use the functions of their wheelchairs or equipment to weight shift or may rely more on caregivers and family to provide assistance.
Pressure relief techniques
- For power wheelchair users, tilting or reclining the chair backwards for a period of time
- For manual wheelchair users, techniques such as leaning forward and propping the elbows onto the knees, lifting the buttocks off the seat by straightening your arms on the armrests, or leaning to one side
- When in bed, techniques such as turning every 2-3 hours, placing pillows between knees and behind the back when lying on your side, and using a suitable pressure relieving surface
This is not a complete or instructive list of pressure relief techniques. Speak to your health provider for detailed instructions on how to perform pressure relief techniques. How-to instructions for some techniques are illustrated on the Spinal Cord Essentials website.
Pressure relief is usually recommended every 15 to 30 minutes to replenish blood flow to vulnerable areas of the skin and held for at least 1 to 2 minutes.
Pressure mapping
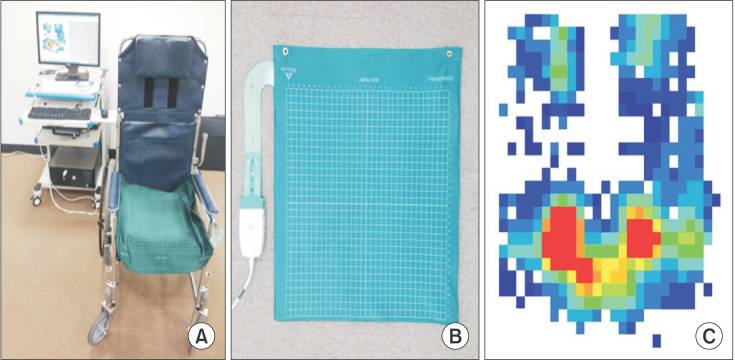
Pressure map placed on a wheelchair (left), flexible pressure map (center), and diagram of pressure of a person’s buttocks in sitting (right). Areas of pressure are indicated from high pressures in red (around the sit bones) to lower pressures in blue.11
Pressure mapping is a technique that involves the use of a pressure-sensitive mat and computer system to identify areas of increased pressure. Pressure mapping may help your health provider make recommendations about reducing pressure, including selecting appropriate equipment and finding out which pressure relief positions work best for you.
Using appropriate equipment and seating
Appropriately fitted equipment like wheelchairs, cushions, and bedding can help to maintain healthy skin. During rehabilitation, you may work with your health providers or attend a special clinic where you receive advice on selecting equipment and the correct use of the equipment.
The team will recommend seat cushions, backrests, commodes, and mattresses to help manage pressure in at-risk areas. Regular check-ins at the clinic may also be needed. Most equipment needs to be reviewed and replaced periodically. For example a padded raised toilet seat that has rips or is worn out can be a cause of a pressure injury.
Keeping a healthy lifestyle
Adopting a healthy diet, exercising regularly, and avoiding smoking are simple steps to help maintain healthy skin.
Nutrition
A healthy diet with enough fluids, calories, and protein provides the nutrients and vitamins needed to maintain healthy skin. It also helps in maintaining a healthy body weight. A dietician can help you learn how to eat well to prevent pressure injuries and can advise you on the nutrition you need for healing should you develop a pressure injury.
Avoiding smoking
 Smoking is a risk factor for pressure injuries because smoking prevents oxygen from reaching the tissues and worsens overall health.
Smoking is a risk factor for pressure injuries because smoking prevents oxygen from reaching the tissues and worsens overall health.
Exercising regularly
Exercise helps to increase circulation (which carries oxygen and nutrients throughout the body) and maintain overall health. Exercise may also help to maintain muscle bulk which creates padding between the skin and bone.
Electrical stimulation
Although it may seem strange, electrical stimulation is a treatment which may help to prevent pressure injuries. Electrical stimulation on its own can help to increase blood flow and oxygen supply to the body tissues. Electrical stimulation during exercise (functional electrical stimulation) may help to maintain muscle mass that pads areas under the skin.
Many people avoid doing regular pressure injury prevention because it can be time-consuming and difficult. If you are having trouble finding the time to fit these techniques in, it may be time to get support. Speak to your health providers about this issue and see if you can work together to come up with ways that you can make pressure relief and skin care a part of your daily activities so you have enough time to participate in everything that is important to you. Some people find the following tips helpful:
- Make skin care a regular part of your routine, just like brushing your teeth – have everything you needs (a mirror, skin care supplies) easily available where you can use them each day and do your routine at the same time every day
- Ask for help from caregivers and family for help with techniques or reminders to maintain good skin care
- Put a timer on your phone or watch to remind you to shift positions regularly.
Peer support
Many places also have peer support programs where people living with SCI can connect and support one another. Peers can offer firsthand knowledge and experience that may help you find the right techniques for your lifestyle. Online support groups and apps may also help you connect with support from people living with SCI.
Organizations that may offer peer support can be found on our Organizations and Foundations Resource page.
Discover how Peter manages pressure sores with his wound care nurse.
Find out how Josh learns how to take care of his pressure sores at home with his wound care nurse.
There are a number of different treatments for pressure injuries. Treatments may be used to reduce pressure or shearing to the wound, keep the wound clean and protected to reduce the risk of infection, and aid circulation and healing. Treatment for pressure sores is the responsibility of the whole health team, so you may work with many different professionals.
Dressings
Wound dressings help to protect the wound, absorb drainage from the wound, and prevent bacteria from entering while also allowing it to breathe. There are many different types of dressings that may be used for pressure sores. Your nurse will help to decide which dressings to use and how often they need to be changed.
Medications
 Antibiotics are used as needed to treat infections in the soft tissues or when osteomyelitis (bone infection) is present. Topical antimicrobial treatments are sometimes applied to the wound to reduce bacteria to try to prevent infection and support healing.
Antibiotics are used as needed to treat infections in the soft tissues or when osteomyelitis (bone infection) is present. Topical antimicrobial treatments are sometimes applied to the wound to reduce bacteria to try to prevent infection and support healing.
Energy-based therapies
A number of different energy-based therapies may also be used to treat pressure injuries. These treatments are done to help increase circulation, kill bacteria, and promote healing.
Electrical stimulation
Electrical stimulation may be applied to pressure injuries through electrodes connected to a small device. Studies suggest that electrical stimulation works to help with healing of severe wounds (stage 3 and 4) after SCI.
Ultraviolet C light
Ultraviolet C light may be applied to a wound using special light bulbs and equipment. Ultraviolet C light has antibacterial effects on wounds. Research suggests that Ultraviolet C is effective for helping treat pressure injuries after SCI.
Debridement
Debridement is a method of removing dead tissue and debris from wounds. There are several methods used to debride wounds and your wound care nurse or physician will choose the method that is right for you. Types of debridement may include:
-
Surgical debridement by a surgeon under anesthesia
- Sharp debridement using sterile scissors performed by a wound care nurse
- Maggot therapy, which involves using maggots to selectively remove only the dead tissue
- Enzymatic debridement, which involves using enzymes to help dissolve the dead tissue
- Autolytic debridement, when moisture is added to the wound as needed to help the dead tissue debride from the wound
Debridement is only needed if there is slough or unhealthy yellow black tissue in the wound base and should only be done when there is enough circulation for healing to occur.
Flap reconstruction surgery
Surgery may be an option if the wound does not improve with other treatments. This is typically only used for stage 3 or stage 4 injuries. The procedure for closing these wounds is called flap reconstruction surgery. Flap reconstruction involves removing the wound and surrounding tissue and covering it with other nearby tissues, such as muscles and skin. After this type of surgery, careful procedures must be followed before you can get up and moving safely.
Amputation
Amputation may sometimes be necessary if a wound gets severely infected and the infection moves into nearby tissues. This is more commonly seen in legs and feet.
Negative pressure treatments
Negative pressure wound treatments involve the use of a vacuum which applies suction to a wound that is covered with a wound dressing. This helps to manage drainage and increase circulation. A negative pressure dressing should only be used when the wound is clean and pink healthy tissue and when the cause of the pressure injury has been addressed.
Other pressure injury treatments
There are many other medical, alternative, and physical treatments that may be used in the treatment of pressure injuries. Speak to your wound care team about any treatments you are considering trying.
Pressure injuries are a common and serious complication of SCI. Many pressure injuries are largely preventable through a combination of regular skin care, pressure relief, staying healthy, and early treatment of potential injuries.
Treatment of pressure sores may involves wound care, electrical and light stimulation, prevention and treatment of infections that may occur, and surgery for severe wounds. Speak with your health providers to discuss your prevention and treatment options to find out which ones are best for you.
For a review of how we assess evidence at SCIRE Community and advice on making decisions, please see SCIRE Community Evidence.
Parts of this page have been adapted from the SCIRE Professional “Skin Integrity and Pressure Injuries” Module:
Hsieh J, McIntyre A, Wolfe D, Lala D, Titus L, Campbell K, Teasell R. (2014). Pressure Ulcers Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors. Spinal Cord Injury Rehabilitation Evidence. Version 5.0. 1-90.
Available from: https://scireproject.com/evidence/skin-integrity-and-pressure-injuries/
Adegoke BO, Badmos KA. Acceleration of pressure ulcer healing in spinal cord injured patients using interrupted direct current. Afr J Med Med Sci 2001;30:195-197.
Ahluwalia R, Martin D, Mahoney JL. The operative treatment of pressure wounds: a 10-year experience in flap selection. Int Wound J 2010;7(2):103-106.
Biglari B, Büchler A, Reitzel T, Swing T, Gerner HJ, Ferbert T, Moghaddam A. A retrospective study on flap complications after pressure ulcer surgery in spinal cord-injured patients. Spinal Cord 2014;52:80-83.
Banks, PG, Ho, CH. A novel topical oxygen treatment for chronic and difficult-to-heal wounds: case studies. Journal of Spinal Cord Medicine 2008;31:297-301.
Bauman WA, Spungen AM, Collins JF, Raisch DW, Ho C, Deitrick GA, et al. The effect of oxandrolone on the healing of chronic pressure ulcers in persons with spinal cord injury: a randomized trial. Ann Int Med 2013; 158(10):718-726.
Bergstrom N, Braden BJ, Laguzza A, Holman V. The Braden Scale for Predicting Pressure Sore Risk. Nurs Res 1987;36:205-210.
Bertheuil N, Huguier V, Aillet S, Beuzeboc M, Watier E. Biceps femoris flap for closure of ischial pressure ulcers. Eur J Plast Surg 2013;6(10):639-644.
Biglari B, Büchler A, eitzel T, Swing T, Gerner H J, Ferbert T, et al. Moghaddamspective study on flap complications fter pressure ulcer surgery in spinal cord-injured patients. Spinal cord 2013; 52(1):80-83.
Bogie KM, Ho CH. Pulsatile lavage for pressure ulcer management in spinal cord injury: a retrospective clinical safety review. Ostomy Wound Manage 2013;59(3):35-38.
Bogie KM, Reger SI, Levine SP, Sahgal V. Electrical stimulation for pressure sore prevention and wound healing. Assist Technol 2000;12:50-66.
Bogie KM, Triolo RJ. Effects of regular use of neuromuscular electrical stimulation on tissue health. J Rehabil Res Dev 2003;40:469-475.
Borgognone A, Anniboletti T, De Vita F, Schirosi M, Palombo P. Ischiatic pressure sores: our experience in coupling a split-muscle flap and a fasciocutaneous flap in a ‘criss-cross’ way. Spinal Cord 2010;48(10):770-773.
Brace JA, Schubart JR. A prospective evaluation of a pressure ulcer prevention and management E-learning program for adults with spinal cord injury. Ostomy Wound Management 2010;56(8):40-50.
Brewer S, Desneves K, Pearce L, Mills K, Dunn L, Brown D, et al. Effect of an arginine-containing nutritional supplement on pressure ulcer healing in community spinal patients. J Wound care 2010;19:7:311-316.
Byrne DW, Salzberg CA. Major risk factors for pressure ulcers in the spinal cord disabled: a literature review. Spinal Cord 1996;34:255-263.
Chen W, Jiang B, Zhao J, Wang P. The superior gluteal artery perforator flap for reconstruction of sacral sores. Saudi Med J 2016;37(10):1140-1143.
Coggrave M, West H, Leonard B. Topical negative pressure for pressure ulcer management. Br J Nurs 2002;11(6):29-36.
Consortium for Spinal Cord Medicine. Pressure ulcer prevention and treatment following spinal cord injury: A clinical practice guideline for health care professionals (pp. 1-77). 2000.
Cukjati D, Robnik-Šikonja M, Reberšek S, Kononenko I, Miklavčič D. Prognostic factors in the prediction of chronic wound healing by electrical stimulation. Med and Bio Eng and Comp 2001;39(5):542-550.
de Angelis B, Lucarini L, Agovino A, Migner A, Orlandi F, Floris M, et al. Combined use of super-oxidised solution with negative pressure for the treatment of pressure ulcers: case report. Int Wond J 2013;10(3):36-339.
de Laat EH, van den Boogaard MH, Spauwen PH, van Kppevelt DH, van Goor H, Schoonhoven L. Faster wound healing with topical negative pressure therapy in difficult-to- heal wounds: a prospective randomized control trial. Ann Plast Surg 2011;67(6):626-631.
Erba P, Wettstein R, Schumacher R, Schwenzer-Zimmerer K, Pierer G, Kalbermatten DF. Silicone moulding for pressure sore debridement. J Plast Reconstr Aesthe Surg 2010;63(3):550-553.
Ferguson AC, Keating JF, Delargy MA, Andrews BJ. Reduction of seating pressure using FES in patients with spinal cord injury: a preliminary report. Paraplegia 1992;30(7):474-478.
Fuhrer MJ, Garber SL, Rintala DH, Clearman R, Hart KA. Pressure ulcers in communityresident persons with spinal cord injury: prevalence and risk factors. Arch Phys Med Rehabil 1993;74(11):1172-1177.
Garber SL, Rintala DH, Holmes SA, Rodriguez GP, Friedman J. A structured educational model to improve pressure ulcer prevention knowledge in veterans with spinal cord dysfunction. J Rehab Res Dev 2002;39(5):575-588.
Grassetti L, Scalise A, Lazzeri D, Carle F, Agostini T, Gesuita R, et al. Perforator flaps in late-stage pressure sore treatment: outcome analysis of 11-year-long experience with 143 patients. Ann Plast Surg 2014;73(6):679-685.
Griffin JW, Tooms RE, Mendius RA, Clifft JK, Vander ZR, El Zeky F et al. Efficacy of high voltage pulsed current for healing of pressure ulcers in patients with spinal cord injury. Phys Ther 1991;71:433-444.
Guihan M, Smith BM, LaVela SL, Garber SL. Factors predicting pressure ulcers in veterans with spinal cord injuries. Amer Journ of Phys Med & Rehab 2008;87(9):750-7.
Gyawali S, Solis L, Chong SL, Curtis C, Seres P, Kornelsen I, et al. Intermittent electrical stimulation redistributes pressure and promotes tissue oxygenation in loaded muscles of individuals with spinal cord injury. Journ Appl Physiol 2011;110(1):246-255
He J, Xu H, Wang T, Ma S, Dong J. Treatment of complex ischial pressure sores with free partial lateral latissimus dorsi musculocutaneous flaps in paraplegic patients. J Plast Reconstr Aesthet Surg 2012;65(5):634-639.
Ho CH, Bensitel T, Wang X, Bogie KM. Pulsatile lavage for the enhancement of pressure ulcer healing: a randomized controlled trial. Phys Ther 2012;92(1):38-48.
Hollisaz MT, Khedmat H, Yari F. A randomized clinical trial comparing hydrocolloid, phenytoin and simple dressings for the treatment of pressure ulcers [ISRCTN33429693]. BMC Dermatol 2004; 4:18.
Houghton PE, Campbell KE and CPG Panel. Canadian best practice guidelines for the prevention and management of pressure ulcers in people with spinal cord injury: A resource handbook for clinicians. Accessed at http://www.onf.org. 2013.
Houghton PE, Campbell KE, Fraser CH, Harris C, Keast DH, Potter PJ et al. Electrical stimulation therapy increases rate of healing of pressure ulcers in community-dwelling people with spinal cord injury. Arch Phys Med Rehabil 2010;91(5):669-678.
Houlihan BV, Jette A, Friedman AH, Paasche-Orlow M, Ni P, Wierbicky J, et al. A pilot study of a telehealth intervention for persons with spinal cord dysfunction. Spinal Cord 2013;51(9):715– 720.
Jercinovic A, Karba R, Vodovnik L, Stefanovska A, Kroselj P, Turk R, et al. Low frequency pulsed current and pressure ulcer healing. Rehab Eng IEEE Transactions on 1994;2(4):225-233.
Kanno N, Nakamura T, Yamanaka M, Kouda K, Nakamura T, Tajima F. Low-echoic lesions underneath the skin in subjects with spinal-cord injury. Spinal cord 2008;47(3):225-229.
Karba, R., Semrov, D., Vodovnik, L., Benko, H., & Savrin, R. DC electrical stimulation for chronic wound healing enhancement. Part 1. Clinical study and determination of electrical field distribution in the numerical wound model. Bioelectrochemistry and Bioenergetics.1997;43:265-270.
Kaya AZ, Turani N, Akyuz M. The effectiveness of a hydrogel dressing compared with standard management of pressure ulcers. Journal of Wound Care 2005;14:42-44.
Keast DH, Fraser C. Treatment of chronic skin ulcers in individuals with anemia of chronic disease using recombinant human erythropoietin (EPO): a review of four cases. Ostomy Wound Manage 2004;50:64-70.
Kennedy P, Berry C, Coggrave M, Rose L, Hamilton L. The effect of a specialist seating assessment clinic on the skin management of individuals with spinal cord injury. J Tissue Viability 2003;13(3):122-125.
Kierney PC, Cardenas DD, Engrav LH, Grant JH, Rand RP. Limb-salvage in reconstruction of recalcitrant pressure sores using the inferiorly based rectus abdominis myocutaneous flap. Plast Reconstr Surg 1998;102(1):111-116.
Kim JT, Kim YH, Naidu S. Perfecting the design of the gluteus maximus perforator-based island flap for coverage of buttock defects. Plast Reconstr Surg 2010;125(6):1744-1751.
Krause JS. Skin sores after spinal cord injury: relationship to life adjustment. Spinal Cord 1998;36(1):51-56.
Lin H, Hou C, Chen A, Xu Z. Long-term outcome of using posterior-thigh fasciocutaneous flaps for the treatment of ischial pressure sores. J Reconstr Microsurg 2010;26(6):355-358.
Liu X, Meng Q, Song H, Zhao T. A traditional Chinese herbal formula improves pressure ulcers in paraplegic patients: A randomized, parallel-group, retrospective trial. Exp Ther Med 2013;5(6):1693-1696.
Loerakker S, Huisman ES, Seelen HA, Glatz JF, Baaijens FP, Oomens CW, et al. Plasma variations of biomarkers for muscle damage in male nondisabled and spinal cord injured subjects. Journ of Rehab Research and Develop 2012;49(3):361-372.
López de Heredia L, Hauptfleisch J, Hughes R, Graham, A, Meagher TM. Magnetic Resonance Imaging of Pressure Sores in Spinal Cord Injured Patients: Accuracy in Predicting Osteomyelitis. Topics in Spinal Cord Injury Rehab 2012;18(2):146-148.
Lui QL, Nicholson GP, Knight SL, Chelvarajah R, Gall A, Middleton FRI, Ferguson-Pell MW, Craggs MD. Pressure changes under the ischial tuberosities of seated individuals during sacral nerve root stimulation. J Rehabil Res Dev 2006;43:209-218.
Lui QL, Nicholson GP, Knight SL, Chelvarajah R, Gall A, Middleton FRI, Ferguson-Pell MW, Craggs MD. Interface pressure and cutaneous hemoglobin and oxygenation changes under ischial tuberosities during sacral nerve root stimulation in spinal cord injury. J Rehabil Res Dev 2006a;43:553-564.
Mawson AR, Siddiqui FH, Connolly BJ, Sharp CJ, Stewart GW, Summer WR, et al. Effect of high voltage pulsed galvanic stimulation on sacral transcutaneous oxygen tension levels in the spinal cord injured. Paraplegia 1993;31(5):311-319.
May L, Day R, Warren S. Evaluation of patient education in spinal cord injury rehabilitation: Knowledge, problem-solving and perceived importance. Disabil Rehabil, 2006;28(7):405–413.
Mehta A, Baker TA, Shoup M, Brownson K, Amde S, Doren E, et al. Biplanar flap reconstruction for pressure ulcers: experience in patients with immobility from chronic spinal cord injuries. Am J Surg 2012;203(3):303-306.
Mortenson WB, Miller WC. A review of scales for assessing the risk of developing a pressure ulcer in individuals with SCI. Spinal Cord 2008;46(3):168-175.
National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Quick Reference Guide. Emily Haesler (Ed.). Cambridge Media: Osborne Park, Western Australia; 2014.
Nussbaum E, Flett H, McGillivray C. Ultraviolet-C (UVC) improves wound healing in persons with spinal cord injury (SCI). Presented at the International Conference on Spinal Cord Medicine and Rehabilitation in Washington, DC; June 4–8, 2011.
Nussbaum EL, Biemann I, Mustard B. Comparison of ultrasound/ultraviolet-C and laser for treatment of pressure ulcers in patients with spinal cord injury. Phys Ther 1994;74:812-823.
Relander M, Palmer B. Recurrence of surgically treated pressure sores. Scand J Plast Reconstr Surg Hand Surg 1988;22(1):89-92.
Rintala DH, Garber SL, Friedman JD, Holmes SA. Preventing recurrent pressure ulcers in veterans with spinal cord injury: impact of a structured education and follow-up intervention. Arch of Phys Med and Rehab 2008;89(8):1429-1441.
Rintala, D. H., Garber, S. L., Friedman, J. D., & Holmes, S. A. Preventing recurrent pressure ulcers in veterans with spinal cord injury: impact of a structured education and follow-up intervention. Archives of Physical Medicine & Rehabilitation. 2008;89:1429-1441
Salzberg CA, Byrne DW, Cayten CG, van Niewerburgh P, Murphy JG, Viehbeck M. A new pressure ulcer risk assessment scale for individuals with spinal cord injury. Amer Journ Phys Med Rehab 1996;75(2):96-104.
Salzberg CA, Cooper-Vastola SA, Perez F, Viehbeck MG, Byrne DW. The effects of non-thermal pulsed electromagnetic energy on wound healing of pressure ulcers in spinal cord-injured patients: a randomized, double-blind study. Ostomy Wound Manage 1995;41:42-4,46,48.
Scevola S, Nicoletti G, Brenta F, Isernia P, Maestri M, Faga A. Allogenic platelet gel in the treatment of pressure sores: a pilot study. Int Wound J 2010;7(3):184-190.
Schubart J. An E-learning program to prevent pressure ulcers in adults with spinal cord injury: A pre- and post- pilot test among rehabilitation patients following discharge to home. Ostomy Wound Management 2012;58(10):38-49.
Sell SA, Ericksen JJ, Reis TW, Droste LR, Bhuiyan MB, Gater DR. A case report on the use of sustained release platelet-rich plasma for the treatment of chronic pressure ulcers. The Journ of Spinal Cord Med 2011;34(1):122.
Sherman RA, Wyle F, Vulpe M. Maggot therapy for treating pressure ulcers in spinal cord injury patients. J Spinal Cord Med 1995;18:71-74.
Singh R, Singh R, Rohilla RK, Siwach R, Verma V, Kaur K. Surgery for pressure ulcers improves general health and quality of life in patients with spinal cord injury. J Spinal Cord Med 2010;33(4):396-400.
Smit CA, Haverkamp GL, de Groot S, Stolwijk-Swuste JM, Janssen TW. Effects of electrical stimulation-induced gluteal versus gluteal and hamstring muscles activation on sitting pressure distribution in persons with a spinal cord injury. Spinal cord 2012;50(8):590-594.
Smit CA, Legemate KJ, de Koning A, de Groot S, Stolwijk-Swuste JM, Janssen,TW. Prolonged electrical stimulation-induced gluteal and hamstring muscle activation and sitting pressure in spinal cord injury: Effect of duty cycle. Journ of Rehab Res Dev 2013;50(7):1035-1046.
Smit CA, Zwinkels M, van Dijk T, de Groot S, Stolwijk-Swuste JM, Janssen TW. Gluteal blood flow and oxygenation during electrical stimulation-induced muscle activation versus pressure relief movements in wheelchair users with a spinal cord injury. Spinal cord 2013;51(9):694-699.
Srivastava A, Gupta A, Taly AB, Murali T. Surgical management of pressure ulcers during inpatient neurologic rehabilitation: outcomes for patients with spinal cord disease. J Spinal Cord Med 2009;32(2):125-131.
Subbanna, P. K., Margaret Shanti, F. X., George, J., Tharion, G., Neelakantan, N., Durai, S. et al. Topical phenytoin solution for treating pressure ulcers: A prospective, randomized, double-blind clinical trial. Spinal Cord. 2007;45:739-743
Taly AB, Sivaraman Nair KP, Murali T, John A. Efficacy of multiwavelength light therapy in the treatment of pressure ulcers in subjects with disorders of the spinal cord: A randomized double-blind controlled trial. Arch Phys Med Rehabil 2004;85:1657-1661.
Tavakoli K, Rutkowski S, Cope C, Hassall M, Barnett R, Richards M, et al. Recurrence rates of ischial sores in para- and tetraplegics treated with hamstring flaps: an 8-year study. Br J Plast Surg 1999;52(6):476-479.
Tzen YT, Brienza DM, Karg PE, Loughlin PJ. Effectiveness of local cooling for enhancing tissue ischemia tolerance in people with spinal cord injury. The journal of spinal cord medicine, 2013;36(4):357-364.
Unal C, Ozdemir J, Yirmibesoglu O, Yucel E, Agir H. Use of inferior gluteal artery and posterior thigh perforators in management of ischial pressure sores with limited donor sites for flap coverage. Ann Plast Surg 2012;69(1):67-72.
van Londen A, Herwegh M, van der Zee CH, Daffertshofer A, Smit CA, Niezen A, Janssen TW. The effect of surface electric stimulation of the gluteal muscles on the interface pressure in seated people with spinal cord injury. Arch of Phys Med and Rehab 2008;89(9):1724-1732.
Vesmarovich S, Walker T, Hauber RP, Temkin A, Burns R. Use of telerehabilitation to manage pressure ulcers in persons with spinal cord injuries. Adv Wound Care 1999;12(5):264-269.
Wang SY, Wang JN, Lv DC, Diao YP, Zhang Z. Clinical research on the bio-debridement effect of maggot therapy for treatment of chronically infected lesions. Orthop Surg 2010;2(3):201-206.
Image credits:
- Reprinted with permission of the copyright holder, Gordian Medical, Inc. dba American Medical Technologies (courtesy of National Pressure Ulcer Advisory Panel)
- Hospital ©Icons Producer, CC BY 3.0
- Modified from: Man Resting on Long Chair ©Gan Khoon Lay, CC BY 3.0
- Image by SCIRE Community Team
- Image by SCIRE Community Team
- Images of pressure ulcer stages used with permission and copyright NPUAP
- Image by SCIRE Community Team
- Image by SCIRE Community Team
- Sweaty-skin ©Jo Andre Johansen, CC BY-SA 2.0
- Image by SCIRE Community Team
- Image from Cho KH, Beom J, Yuk JH, Ahn SC. The Effects of Body Mass Composition and Cushion Type on Seat-Interface Pressure in Spinal Cord Injured Patients. Ann Rehabil Med. 2015 Dec;39(6):971-9. doi: 10.5535/arm.2015.39.6.971. Epub 2015 Dec 29. Published online 2015 Dec 29. doi: 10.5535/arm.2015.39.6.971 (CC BY-NC 4.0)
- CWSC Panthers ©DSC_0284, CC BY-SA 2.0
- Mirror ©Vectors Market, CC BY 3.0
- Pills ©Sketch2SVG, CC BY 3.0
- MEDRETE 16-2 ©US Army Africa. CC BY 2.0
Author: SCIRE Community Team | Reviewer: Shannon Sproule | Published: 18 October 2017 | Updated: ~
Pressure mapping is a clinical technique that is used to help prevent pressure sores after spinal cord injury (SCI). This page outlines how pressure mapping is used after SCI.
Key Points
- Pressure mapping is a technique that involves the use of a pressure-sensitive mat and computer system to measure the amount of pressure between a person’s body and a supporting surface.
- Pressure mapping is used to help identify areas of excess pressure that may contribute to pressure sores. This can be used to help make decisions about surface options (like wheelchair cushions and bedding) and find out how effective a person’s pressure relief techniques are.
- This technique involves the use of a flexible mat containing pressure sensors that is placed on the surface being tested and then the person is positioned on the mat. The mat is connected to a computer system that creates a color-coded diagram showing areas of pressure.
- Pressure mapping is considered to be a useful tool for making decisions about reducing pressure that is used as a decision-making and educational tool. There is a lack of research on whether pressure mapping directly helps to reduce pressure sores after SCI.
Pressure mapping is a technique that is used to identify areas of pressure between a person’s body and a supporting surface like a cushion or chair. A thin, pressure-sensitive mat and computer system are used to develop a map showing areas of pressure where the body contacts the surface. This technique is most often used to identify areas of high pressure associated with wheelchair seating that could contribute to the development of pressure sores.
See our article on Pressure Sores to learn more!
Pressure mapping is also used on other such as mattresses, toilet seats, car seats, sports equipment, or any other surface a person sits or lies on for periods of time that may influence their skin health.
People with spinal cord injuries have an increased risk of developing skin lesions called pressure sores. Pressure sores occur for many reasons, including increased pressure on vulnerable areas of the skin. Bony areas that come into contact with support surfaces, like the sit bones and tailbone in sitting, are highly vulnerable to increased pressure.
Learn how proper wheelchair seating can reduce the risk of pressure sores.
Pressure mapping is used to determine areas of increased pressure in certain postures on specific surfaces. It may be used to assess areas of pressure on various surfaces, such as chairs, beds, sofas, car seats, and toilet seats. This information can be used to develop strategies to reduce pressure and improve comfort in these situations.
Pressure mapping may be used as a tool to aid decision-making when selecting support surfaces and equipment, such as assessing which wheelchair cushions provide the best pressure relief for you. Pressure mapping is also used to assess the effectiveness of pressure relief techniques like weight-shifting by providing real-time feedback about the pressure during the performance of these techniques.
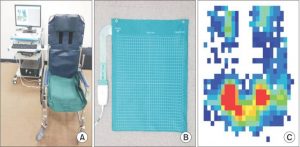
Pressure map placed on a wheelchair (left), flexible pressure map (center), and diagram of pressure of a person’s buttocks in sitting (right). Areas of pressure are indicated from high pressures in red (around the sit bones) to lower pressures in blue.3
A flexible mat containing pressure sensors is placed on the surface to be tested. The person being assessed then sits on the mat. Information about pressure between their body and the seat is picked up by sensors in the mat and sent to a computer, where it is translated into a color coded diagram.
The diagram displays the pressure recorded at each sensor in the mat by number and displays areas of high and low pressure with different colors. A clinician then determines the corresponding areas on the body through a hands-on physical examination. This technique is used together with other assessments of pressure sore risk to make recommendations for reducing areas of high pressure. There may be variation in the procedures used for pressure mapping in different settings.

Pressure mapping can be influenced by many aspects of how the procedure is done. For example, how the person positions themselves at the time of the reading and how long the person sits on the mat before the readings are taken can change the findings. There are also different types of systems that collect information about pressure differently. These factors and other concerns have led to disagreement among experts about how to best understand and interpret the results of pressure mapping for clinical use.
In addition, pressure is just one factor that contributes to pressure sores. Friction, moisture, age, body composition, time spent sitting, and many other factors also contribute to pressure sores. These factors cannot be detected by pressure mapping, which limits the use of pressure mapping as a stand-alone tool.
Pressure mapping also requires special equipment and trained health providers which may not be available in settings outside of major rehabilitation centers.
Pressure mapping is considered by experts to be a useful tool for understanding pressure and making decisions about pressure relief. At this time, most of the research that has been done on whether pressure mapping is effective for preventing pressure sores has been done in populations outside of SCI. We do not know if pressure mapping is effective for preventing of pressure sores in people with SCI.
Pressure mapping is clinical tool that may be used in rehabilitation centers to help assess the risk of pressure sores. It is considered to be a valuable tool for making decisions about reducing pressure as well as a useful educational tool for understanding pressure in different positions. There is a lack of research on whether pressure mapping directly helps to reduce pressure sores after SCI.
Hsieh J, McIntyre A, Wolfe D, Lala D, Titus L, Campbell K, Teasell R. (2014). Pressure Ulcers Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors. Spinal Cord Injury Rehabilitation Evidence. Version 5.0. 1-90.
Available from: https://scireproject.com/evidence/rehabilitation-evidence/skin-integrity-pressure-injuries/
Barnett RI, Shelton FE. Measurement of support surface efficacy: pressure. Adv Wound Care 1997; 10(7):21-9.
Brienza DM, Karg PE, Geyer MJ, Kelsey S, Trefler E. The relationship between pressure ulcer incidence and buttock-seat cushion interface pressure in at-risk elderly wheelchair users. Arch Phys Med Rehabil 2001; 82(4):529-33.
Eitzen I. Pressure mapping in seating: a frequency analysis approach. Arch Phys Med Rehabil 2004; 85(7):1136-40.
Ferguson-Pell M, Cardi MD. Prototype development and comparative evaluation of wheelchair pressure mapping system. Assist Technol 1993; 5(2):78-91.
Hamanami K, Tokuhiro A, Inoue H. Finding the optimal setting of inflated air pressure for a multi-cell air cushion for wheelchair patients with spinal cord injury. Acta Med Okayama 2004; 58(1):37-44.
Hanson D, Langemo D, Anderson J, Hunter S, Thompson P. Pressure mapping: seeing the invisible. Adv Skin Wound Care 2006; 19(8):432-4.
Henderson JL, Price SH, Brandstater ME, Mandac BR. Efficacy of three measures to relieve pressure in seated persons with spinal cord injury. Arch Phys Med 1994;75:535-9.
Jan YK, Brienza DM. Technology for Pressure Ulcer Prevention. Top Spinal Cord Inj Rehabil; 2006; 11(3):30-41.
Kernozek TW, Lewin JE. Seat interface pressures of individuals with paraplegia: influence of dynamic wheelchair locomotion compared with static seated measurements. Arch Phys Med Rehabil 1998; 79(3):313-6.
Rondorf-Klym LM, Langemo D. Relationship between body weight, body position, support surface, and tissue interface pressure at the sacrum. Decubitus 1993; 6(1):22-30.
Shelton F, Barnett R, Meyer E. Full-body interface pressure testing as a method for performance evaluation of clinical support surfaces. Appl Ergon 1998; 29(6):491-7.
Stinson MD, Porter-Armstrong A. Seating and pressure support needs of people with cancer in the cervix or rectum: a case series on the clinical usefulness of pressure mapping assessment. Euro J Cancer Care 2007; 17:298-305.
Stinson MD, Porter-Armstrong A, Eakin P. Seat-interface pressure: a pilot study of the relationship to gender, body mass index, and seating position. Arch Phys Med Rehabil 2003; 84(3):405-9.
Sonenblum SE, Sprigle SH. The impact of tilting on blood flow and localized tissue loading. J Tissue Variability 2011;20:3-13.
Taule T, Bergfjord EE, Lunde T, Stokke BH, Storlind H, Sorheim MV et al. Factors influencing optimal seating pressure after spinal cord injury. Spinal Cord 2013;51:273-7.
Image credits
- Veterans wheelchair games 2009 ©U.S. Air Force photo/Staff Sgt. Desiree N. Palacios, CC0 1.0
- Reprinted with permission of the copyright holder, Gordian Medical, Inc. dba American Medical Technologies (courtesy of National Pressure Ulcer Advisory Panel).
- Image ©Cho KH, Beom J, Yuk JH, Ahn SC, CC BY-NC 4.0
- Sit ©Rudez Studio, CC BY 3.0 US
Author: SCIRE Community Team | Reviewer: Shannon Sproule | Published: 10 October 2017 | Updated: ~
Functional electrical stimulation is a treatment that activates muscles below the spinal cord injury (SCI) during exercise and activity. This page outlines basic information about functional electrical stimulation and its use for movement and strength after SCI.
Key Points
- Electrical stimulation can be used to activate muscles that are weak or paralyzed after an SCI.
- Functional electrical stimulation (FES) involves stimulating the muscles during an activity like exercise or movement.
- FES is relatively safe and widely available treatment option for improving muscle strength and fitness after SCI.
- Overall, the research evidence suggests that FES is most likely effective for improving muscle strength after SCI. It may also improve fitness, walking skills, bone density and other symptoms, although more high quality research is needed to confirm.
Functional electrical stimulation (FES) is a type of neuromodulation where electrical stimulation is applied to the nerves located outside the spinal cord and brain. This stimulation causes the muscles to contract and can assist with purposeful or functional movement in weak or paralyzed muscles.
FES is delivered using a variety of handheld or specialized commercial electrical therapy machines connected to electrodes that are placed on the skin’s surface. Systems are also available with implanted electrodes in the muscles, although this is very specialized and not widely available.
Muscle stimulation is used for several reasons after SCI:
To promote movement and strength in weak or paralyzed muscles: Muscle stimulation is used early in rehabilitation to promote movement in muscles that are not moving or only producing a flicker of movement. It may promote recovery of movement function by assisting with normal movements and with repetition of movements.
To improve fitness and health: When FES is used as part of a rhythmic exercise like cycling, walking, or rowing, it can help to maintain health of the heart, lungs, and circulation. It may also help to maintain healthy bones.
To assist with functional movement activities like stepping, getting up to standing, and grasping: FES can be used to assist with purposeful movements by improving muscle contractions (for weakened muscles), mobility or range of movement as well as possibly decreasing spasticity.
To maintain muscle mass below the SCI: Regular use of FES may help to prevent muscle loss that happens when the muscles that are paralyzed are not used. Unless neurological return occurs this improvement will stop if the FES is discontinued.
To control the muscles of breathing and bladder function: This includes the use of surgically implanted diaphragmatic pacers (FES systems that create muscle contractions in the diaphragm to stimulate regular breaths) and bladder control systems (FES systems that stimulate the muscles of urination). However, this page will focus on FES used for movement and strength after SCI.
Watch our YouTube video about FES!
Other names for FES of muscles
You may hear other names for FES such as “neuromuscular electrical stimulation” (NMES) or simply “electrical stimulation” (ES). These terms are often used to refer to electrical stimulation of the muscles during more passive activities (like lying down or sitting), while ”FES” usually describes stimulation during purposeful activities like cycling or walking. However, in practice these terms are often used interchangeably to describe similar or related treatments and the goals of all are to promote strength, movement and function and decrease pain and spasticity.
There are a number of other neuromodulation techniques that are used for various purposes in SCI, including transcutaneous electrical nerve stimulation, sacral nerve stimulation, and intrathecal Baclofen, described in other SCIRE Community articles.
It is important to speak with a health provider about using FES to make sure it is safe and suitable for you and to learn how to use the equipment correctly.
FES is usually applied through electrodes that are placed on the surface of the skin, although electrodes can also be implanted into the muscles. Electrodes are placed over nerves or part of the muscles below the SCI that respond well to electrical stimulation. The electrodes are then attached to an adjustable machine that generates the stimulation. Your health provider will determine the settings that are used for the treatment and how long it will last.
The electrical stimulation is then gradually turned up until the muscles begin to tense or contract. Depending on your sensation, as the machine is turned up, you may feel pins and needles or other unusual sensations, which may take some time to get used to. The aim is to create a forceful but tolerable muscle contraction.

FES is applied through electrodes on the leg muscles during assisted walking.2
If the electrical stimulation goes well, it is then combined with a movement task. This may be as simple as lifting a wrist or ankle or more complex such as cycling on a stationary bike, rowing on a rowing machine, grasping, or stepping in parallel bars or a body weight support treadmill system.
The length of each session will vary depending on the goals of the treatment. Time may be required to enable your muscles to tolerate longer sessions as the muscles may fatigue quickly. Sessions are usually done several times per week for several weeks to gain training benefits.
Your health provider will monitor your response to the treatment and inspect the skin for any redness or irritation after the treatment has ended. Once you have learned to use FES safely, you may be able to use it on your own.
Our bodies naturally use electrical signals as part of the nervous system. When we move, the brain generates and sends electrical impulses along the spinal cord and nerves to tell the muscles to move.
Spinal cord injury can interrupt this pathway, preventing electrical impulses from passing through the spinal cord to reach the muscles. However, if the nerves and muscles below the injury are not damaged, they can still respond to electrical signals.

FES electrodes are placed over nerves or over electrically-sensitive parts of the muscles below the SCI. The specific type of electrical stimulation used with FES can trigger the nerve cells of movement (motor neurons) to send signals that cause muscle movement. An intact peripheral nerve and healthy muscle tissue are required to enable the external source of electricity to facilitate muscle contraction.
FES does not work for nerve injuries outside the spinal cord
FES can only be used for muscle weakness or paralysis caused by injuries to the spinal cord, but not injuries to the conus medullaris, cauda equina, or the nerves outside of the spinal cord. The nerve cells in these structures (called lower motor neurons) must to be intact for FES to work.
Like exercise, regular treatment with FES is usually needed to maintain the effects of the treatment. For people with complete injuries, when FES treatments are stopped, the treatment effects will usually go away over time. For people with incomplete injuries, the goal is for some carryover of strength and movement be retained after the treatment is stopped.
 There are some situations in which FES may be unsafe to use. This not a complete list, speak to a health provider about your health history and whether FES is safe for you.
There are some situations in which FES may be unsafe to use. This not a complete list, speak to a health provider about your health history and whether FES is safe for you.
FES should not be used in the following situations:
- Near implanted medical devices like heart pacemakers
- On areas of active cancer, or by people with bleeding disorders or other major medical conditions
- On areas with blood clots, bleeding, damaged skin, infection, or poor circulation
- By pregnant women
- Electrodes should not be placed over the eyes, through the head, through the chest or abdomen, or on the front of the neck or genitals
- By people with recent broken bones
- By people with damage to the nerves or muscles near the area where FES is used
FES should be used with caution in the following situations:
FES is often used with the following conditions after SCI but should be monitored closely. Speak to your health provider for more information.
- By people who have had seizures
- By people prone to severe autonomic dysreflexia (people with cervical and thoracic injuries)
- By people with uncontrolled spasticity
- By people with severe osteoporosis
- In areas where heterotopic ossification causes restricted movement
- In areas with reduced or absent sensation (below the level of injury)
- By people who are unable to follow instructions or provide accurate feedback
FES is generally well tolerated by people who can use it safely (see above for when FES may be unsafe). Serious medical complications from FES are rare. However, there are risks and side effects that should be discussed with a health provider before using FES.
More common risks and side effects of FES include:
- Discomfort or pain
- Skin redness or irritation
- Nausea, light-headedness, or autonomic dysreflexia
Other less common risks and side effects of FES include:
- Mild electrical burns near the electrodes
- Skin breakdown near the electrodes
- Fainting
- Worsening of muscle spasms (spasticity)
- Muscle and joint injuries, such as joint swelling or muscle strains
- Broken bones
- Mild electrical shocks (from improper use or faulty equipment)
In some cases, risks and side effects may be caused by improper use of the equipment. It is essential to learn to use the equipment from a health provider and to only use FES according to their direction and with the settings that they recommend.
For some people, side effects of FES may be stronger at first, but as their body gets used to FES with repeated treatments, their physical reactions may reduce over time.
Several studies have shown that FES helps to improve strength and fitness after SCI.
Strength
 Studies have shown that both FES arm exercise and FES cycling helps to maintain or improve strength after SCI. However, FES cycling may be more effective for maintaining strength after injury than improving strength that has already been lost. This is supported by moderate evidence from five studies.
Studies have shown that both FES arm exercise and FES cycling helps to maintain or improve strength after SCI. However, FES cycling may be more effective for maintaining strength after injury than improving strength that has already been lost. This is supported by moderate evidence from five studies.
Cardiovascular fitness
 Fifteen studies have looked at FES for improving many different aspects of fitness after SCI. Taken altogether, these studies provide weak evidence that FES training done at least 3 days per week for 2 months helps to improve many aspects of cardiovascular fitness after SCI.
Fifteen studies have looked at FES for improving many different aspects of fitness after SCI. Taken altogether, these studies provide weak evidence that FES training done at least 3 days per week for 2 months helps to improve many aspects of cardiovascular fitness after SCI.
Walking
 Studies show that FES improves walking speed and distance in people with both incomplete and complete SCI. Some of these studies also showed that regular use of FES carried over to improve walking even without FES. This is supported by weak evidence from eight studies.
Studies show that FES improves walking speed and distance in people with both incomplete and complete SCI. Some of these studies also showed that regular use of FES carried over to improve walking even without FES. This is supported by weak evidence from eight studies.
The effects of FES treatment may also help to prevent complications of SCI like pressure sores, bone loss, spasticity, and orthostatic hypotension. These benefits may accompany gains in strength or fitness related to FES treatment.
Pressure sores
 Although it is commonly thought that increased muscle bulk from FES will reduce the risk of pressure sores, there are not very many studies which have looked at whether this actually happens. One study provides weak evidence that FES cycling for 2 years reduced the number of pressure ulcers that occurred after SCI. Another study showed that regular FES cycling showed a trend toward reducing seat pressures.
Although it is commonly thought that increased muscle bulk from FES will reduce the risk of pressure sores, there are not very many studies which have looked at whether this actually happens. One study provides weak evidence that FES cycling for 2 years reduced the number of pressure ulcers that occurred after SCI. Another study showed that regular FES cycling showed a trend toward reducing seat pressures.
Bone health
 Research studies show that FES cycling does not prevent bone loss after SCI (moderate evidence from two studies). However, it may help to increase bone density that has already been lost, although the evidence for this is conflicting (based on six studies). It is not clear whether any gains in bone density last long-term or if continued FES treatment is needed for them to be maintained.
Research studies show that FES cycling does not prevent bone loss after SCI (moderate evidence from two studies). However, it may help to increase bone density that has already been lost, although the evidence for this is conflicting (based on six studies). It is not clear whether any gains in bone density last long-term or if continued FES treatment is needed for them to be maintained.
For more information on bone density, read our article about Osteoporosis.
Spasticity
It is not clear what effects FES has on spasticity after SCI. There is conflicting evidence from three studies about whether FES cycling can help to reduce spasticity after SCI.
Click here for our article on Spasticity.
Orthostatic hypotension
Three studies provide moderate evidence that FES of the legs during a single change in position reduced orthostatic hypotension. However, this only shows that FES prevents orthostatic hypotension while it is applied, and further research is needed to look at what benefits this could have to people living with SCI.
Overall, the research evidence suggests that FES is most likely effective for improving muscle strength after SCI. It may also have effects on fitness, walking skills, bone density, skin health, spasticity, and orthostatic hypotension, although more high quality research is needed to confirm. FES appears to be safe when used appropriately and is widely available in most rehabilitation settings. Discuss this treatment with your health providers to find out if it is a suitable treatment option for you.
For a review of how we assess evidence at SCIRE Community and advice on making decisions, please see SCIRE Community Evidence.
Parts of this page have been adapted from the SCIRE Professional “Lower Limb”, “Upper Limb”, “Bone Health”, “Cardiovascular Health and Exercise”, “Orthostatic Hypotension”, “Pressure Ulcers”, and “Spasticity” chapters:
Lam T, Wolfe DL, Domingo A, Eng JJ, Sproule S (2014). Lower Limb Rehabilitation Following Spinal Cord Injury. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors. Spinal Cord Injury Rehabilitation Evidence. Version 5.0. Vancouver: p 1-74.
Available from: http://scireproject.com/evidence/lower-limb/
Connolly SJ, McIntyre A, Mehta, S, Foulon BL, Teasell RW. (2014). Upper Limb Rehabilitation Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors. Spinal Cord Injury Rehabilitation Evidence. Version 5.0: p 1-77.
Available from: http://scireproject.com/evidence/upper-limb/
Craven C, Lynch CL, Eng JJ (2014). Bone Health Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors. Spinal Cord Injury Rehabilitation Evidence. Version 5.0. Vancouver: p 1- 37.
Available from: https://scireproject.com/evidence/bone-health/
Warburton DER, Krassioukov A, Sproule S, Eng JJ (2014). Cardiovascular Health and Exercise Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors. Spinal Cord Injury Rehabilitation Evidence. Version 5.0. Vancouver: p. 1-48.
Available from: https://scireproject.com/evidence/cardiovascular-health-and-exercise/
Krassioukov A, Wecht JM, Teasell RW, Eng JJ (2014). Orthostatic Hypotension Following Spinal Cord Injury. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors. Spinal Cord Injury Rehabilitation Evidence. Version 5.0. Vancouver: p. 1-26.
Available from: https://scireproject.com/evidence/orthostatic-hypotension/
Hsieh J, McIntyre A, Wolfe D, Lala D, Titus L, Campbell K, Teasell R. (2014). Pressure Ulcers Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors. Spinal Cord Injury Rehabilitation Evidence. Version 5.0. 1-90.
Available from: https://scireproject.com/evidence/skin-integrity-and-pressure-injuries/
Hsieh JTC, Connolly SJ, McIntyre A, Townson AF, Short C, Mills P, Vu V, Benton B, Wolfe DL (2016). Spasticity Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Curt A, Mehta S, Sakakibara BM, editors. Spinal Cord Injury Rehabilitation Evidence. Version 6.0.
Available from: https://scireproject.com/evidence/spasticity/
Evidence for “Strength” is based on the following studies:
[1] Baldi JC, Jackson RD, Moraille R, and Mysiw WJ. Muscle atrophy is prevented in patients with acute spinal cord injury using functional electrical stimulation. Spinal Cord 1998;36:463-469.
[2] Scremin AM, Kurta L, Gentili A, Wiseman B, Perell K, Kunkel C, and Scremin OU. Increasing muscle mass in spinal cord injured persons with a functional electrical stimulation exercise program. Arch Phys Med Rehabil 1999;80:1531-1536.
[3] Crameri RM, Weston A, Climstein M, Davis GM, and Sutton JR. Effects of electrical stimulation-induced leg training on skeletal muscle adaptability in spinal cord injury. Scand J Med Sci Sports 2002;12:316-322.
[4] Gerrits HL, de Haan A, Sargeant AJ, Dallmeijer A, and Hopman MT. Altered contractile properties of the quadriceps muscle in people with spinal cord injury following functional electrical stimulated cycle training. Spinal Cord 2000;38:214-223.
[5] Needham-Shropshire BM, Broton JG, Cameron TL, Klose J. Improved motor function in tetraplegics following neuromuscular stimulation-assisted arm ergometry. J Spinal Cord Med 1997;20:49-55.
[6] Cameron T, Broton JG, Needham-Shropshire B, Klose KJ. An upper body exercise system incorporating resistive exercise and neuromuscular electrical stimulation (nms). J Spinal Cord Med 1998;21:1-6.
Evidence for “Cardiovascular Fitness” based on:
[1] Berry HR, Kakebeeke TH, Donaldson N, Perret C, Hunt KJ. Energetics of paraplegic cycling: adaptation to 12 months of high volume training. Technology and Health Care 2012; 20: 73-84.
[2] Griffin L, Decker MJ, Hwang JY, Wang B, Kitchen K, Ding Z, et al. Functional electrical stimulation cycling improves body composition, metabolic and neural factors in persons with spinal cord injury. J Electromyogr Kinesiol 2009;19(4):614-22.
[3] Zbogar D, Eng JJ, Krassioukov AV, Scott JM, Esch BT, Warburton DE. The effects of functional electrical stimulation leg cycle ergometry training on arterial compliance in individuals with spinal cord injury. Spinal Cord 2008;46(11):722-6.
[4] Crameri RM, Cooper P, Sinclair PJ, Bryant G, Weston A. Effect of load during electrical stimulation training in spinal cord injury. Muscle Nerve 2004;29(1):104-11.
[5] Hjeltnes N, Aksnes AK, Birkeland KI, Johansen J, Lannem A, Wallberg-Henriksson H. Improved body composition after 8 wk of electrically stimulated leg cycling in tetraplegic patients. Am J Physiol 1997;273(3 Pt 2):R1072-9.
[6] Mohr T, Andersen JL, Biering-Sorensen F, Galbo H, Bangsbo J, Wagner A, et al. Long-term adaptation to electrically induced cycle training in severe spinal cord injured individuals. Spinal Cord 1997;35(1):1-16.
[7] Barstow TJ, Scremin AM, Mutton DL, Kunkel CF, Cagle TG, Whipp BJ. Changes in gas exchange kinetics with training in patients with spinal cord injury. Med Sci Sports Exerc 1996;28(10):1221-8.
[8] Faghri PD, Glaser RM, Figoni SF. Functional electrical stimulation leg cycle ergometer exercise: training effects on cardiorespiratory responses of spinal cord injured subjects at rest and during submaximal exercise. Arch Phys Med Rehabil 1992;73(11):1085-93.
[9] Hooker SP, Figoni SF, Rodgers MM, Glaser RM, Mathews T, Suryaprasad AG, et al. Physiologic effects of electrical stimulation leg cycle exercise training in spinal cord injured persons. Arch Phys Med Rehabil 1992;73(5):470-6.
[10] Gerrits HL, de Haan A, Sargeant AJ, van Langen H, Hopman MT. Peripheral vascular changes after electrically stimulated cycle training in people with spinal cord injury. Arch Phys Med Rehabil 2001;82(6):832-9.
[11] Ragnarsson KT, Pollack S, O’Daniel W, Jr., Edgar R, Petrofsky J, Nash MS. Clinical evaluation of computerized functional electrical stimulation after spinal cord injury: a multicenter pilot study. Arch Phys Med Rehabil 1988;69(9):672-7.
[12] Taylor JA, Picard G, Widrick JJ. Aerobic capacity with hybrid FES rowing in spinal cord injury: comparison with arms-only exercise and preliminary findings with regular training. PM R 2011;3(9):817-24.
[13] Kahn NN, Feldman SP, Bauman WA. Lower-extremity functional electrical stimulation decreases platelet aggregation and blood coagulation in persons with chronic spinal cord injury: a pilot study. J Spinal Cord Med 2010;33(2): 150-8.
[14] Hakansson NA, Hull ML. Can the efficacy of electrically stimulating pedaling using a commercially available ergometer be improved by minimizing the muscle stress-time integral? Muscle Nerve 2012; 45:393-402.
Evidence for “Walking” is based on the following studies:
[1] Thrasher TA, Flett HM, and Popovic MR. Gait training regimen for incomplete spinal cord injury using functional electrical stimulation. Spinal Cord 2006;44:357-361.
[2] Ladouceur M, and Barbeau H. Functional electrical stimulation-assisted walking for persons with incomplete spinal injuries: changes in the kinematics and physiological cost of overground walking. Scand J Rehabil Med 2000a;32:72-79.
[3] Ladouceur M, and Barbeau H. Functional electrical stimulation-assisted walking for persons with incomplete spinal injuries: longitudinal changes in maximal overground walking speed. Scand J Rehabil Med 2000b;32:28-36.
[4] Wieler M, Stein RB, Ladouceur M, Whittaker M, Smith AW, Naaman S, Barbeau H, Bugaresti J, and Aimone E. Multicenter evaluation of electrical stimulation systems for walking. Arch Phys Med Rehabil 1999;80:495-500.
[5] Klose KJ, Jacobs PL, Broton JG, Guest RS, Needham-Shropshire BM, Lebwohl N, Nash MS, and Green BA. Evaluation of a training program for persons with SCI paraplegia using the Parastep 1 ambulation system: part 1. Ambulation performance and anthropometric measures. Arch Phys Med Rehabil 1997;78:789-793.
[6] Granat MH, Ferguson AC, Andrews BJ, and Delargy M. The role of functional electrical stimulation in the rehabilitation of patients with incomplete spinal cord injury–observed benefits during gait studies. Paraplegia 1993;31:207-215.
[7] Stein RB, Belanger M, Wheeler G, Wieler M, Popovic DB, Prochazka A, and Davis LA. Electrical systems for improving locomotion after incomplete spinal cord injury: an assessment. Arch Phys Med Rehabil 1993;74:954-959.
[8] Granat M, Keating JF, Smith AC, Delargy M, and Andrews BJ. The use of functional electrical stimulation to assist gait in patients with incomplete spinal cord injury. Disabil Rehabil 1992;14:93-97.
Evidence for “Bone health” is based on the following studies:
[1] Eser P, de Bruin ED, Telley I, Lechner HE, Knecht H, Stussi E. Effect of electrical stimulation-induced cycling on bone mineral density in spinal cord-injured patients. Eur J Clin Invest 2003;33:412-419.
[2] Lai CH, Chang WHS, Chan WP, Peng CW, Shen LK, Chen JJJ, Chen SC. Effects of Functional Electrical Stimulation Cycling Exercise on Bone Mineral Density Loss in the Early Stages of Spinal Cord Injury. J Rehabil Med 2010; 42:150-154.
[3] Mohr T, Podenphant J, Biering-Sorensen F, Galbo H, Thamsborg G, Kjaer M. Increased bone mineral density after prolonged electrically induced cycle training of paralyzed limbs in spinal cord injured man. Calcif Tissue Int 1997;61:22-25.
[4] Chen SC, Lai CH, Chan WP, Huang MH, Tsai HW, Chen JJ. Increases in bone mineral density after functional electrical stimulation cycling exercises in spinal cord injured patients. Disabil Rehabil 2005;27:1337-1341.
[5] Frotzler A, Coupaud S, Perret C, Kakebeeke TH, Hunt KJ, Donaldson Nde N, Eser P. High-volume FES-cycling partially reverses bone loss in people with chronic spinal cord injury. Bone. 2008 Jul;43(1):169-76. Epub 2008 Mar 20.
[6] Pacy PJ, Hesp R, Halliday DA, Katz D, Cameron G, Reeve J. Muscle and bone in paraplegic patients, and the effect of functional electrical stimulation. Clin Sci (Lond) 1988;75:481-487.
[7] Leeds EM, Klose J, Ganz W, Serafini A, Green BA. Bone mineral density after bicycle ergometry training. Archives of Physical Medicine and Rehabilitation 1990;71:207-9.
[8] BeDell KK, Scremin AM, Perell KL, Kunkel CF. Effects of functional electrical stimulation-induced lower extremity cycling on bone density of spinal cord-injured patients. Am J Phys Med Rehabil 1996;75:29-34.
Evidence for “Pressure Ulcers” is based on the following studies:
[1] Dolbow DR, Gorgey AS, Dolbow JD, Gater DR. Seat pressure changes after eight weeks of functional electrical stimulation cycling: a pilot study. Top Spinal Cord Inj Rehabil. 2013 Summer;19(3):222-8.
[2] Petrofsky JS. Functional electrical stimulation, a two year study. J Rehabil. 1992;58(3):29–34
Evidence for “Spasticity” is based on the following studies:
[1] Kapadia N, Masani K, Craven B, et al. A randomized trial of functional electrical stimulation for walking in incomplete spinal cord injury: Effects on walking competency. J Spinal Cord Med 2014;37:511-24.
[2] Manella K & Field-Fote E. Modulatory effects of locomotor training on extensor spasticity in individuals with motor-incomplete spinal cord injury. Restor Neurol Neurosci 2013;31:633-46.
[3] Ralston K, Harvey L, Batty J, et al. Functional electrical stimulation cycling has no clear effect on urine output, lower limb swelling, and spasticity in people with spinal cord injury: A randomised cross-over trial. J Physiother 2013;59:237-43.
[4] Kuhn D, Leichtfried V, Schobersberger W. Four weeks of functional electrical stimulated cycling after spinal cord injury: a clinical cohort study. Inter J Rehabil Res 2014;37:243-50.
[5] Mazzoleni S, Stampacchia G, Gerini A, Tombini T, Carrozza M. FES-cycling training in spinal cord injured patients. Eng Med Biol Soc 2013:5339-41.
[6] Sadowsky C, Hammond E, Strohl A, et al. Lower extremity functional electrical stimulation cycling promotes physical and functional recovery in chronic spinal cord injury. J Spinal Cord Med 2013;36:623-31.
[7] Reichenfelser W, Hackl H, Hufgard J, Kastner J, Gstaltner K, Gföhler M. Monitoring of spasticity and functional ability in individuals with incomplete spinal cord injury with a functional electrical stimulation cycling system. J Rehabil Med 2012;44:444-9.
[8] Krause P, Szecsi J, Straube A. Changes in spastic muscle tone increase in patients with spinal cord injury using functional electrical stimulation and passive leg movements. Clin Rehabil 2008;22:627-34.
[9] Mirbagheri M, Ladouceur M, Barbeau H, Kearney R. The effects of long-term FES-assisted walking on intrinsic and reflex dynamic stiffness in spastic spinal-cord-injured
[10] Granat M, Ferguson A, Andrews B, Delargy M. The role of functional electrical stimulation in the rehabilitation of patients with incomplete spinal cord injury–observed benefits during gait studies. Paraplegia 1993;31:207-15.
[11] Thoumie P, Le C, Beillot J, Dassonville J, Chevalier T, Perrouin-Verbe B et al. Restoration of functional gait in paraplegic patients with the RGO-II hybrid orthosis. A multicenter controlled study. II: Physiological evaluation. Paraplegia 1995;33:654-9.
Evidence for “Orthostatic Hypotension” is based on the following studies:
[1] Faghri PD, Yount J. Electrically induced and voluntary activation of physiologic muscle pump: a comparison between spinal cord-injured and able-bodied individuals. Clin Rehabil 2002;16:878-885.
[2] Elokda AS, Nielsen DH, Shields RK. Effect of functional neuromuscular stimulation on postural related orthostatic stress in individuals with acute spinal cord injury. J Rehabil Res Dev 2000;37:535-542.
[3] Sampson EE, Burnham RS, Andrews BJ. Functional electrical stimulation effect on orthostatic hypotension after spinal cord injury. Arch Phys Med Rehabil 2000; 81: 139-143.
Other references:
Electrophysical Agents – Contraindications And Precautions: An Evidence-Based Approach To Clinical Decision Making In Physical Therapy. Physiother Can. 2010 Fall;62(5):1-80.
Gibbons RS, Shave RE, Gall A, Andrews BJ. FES-rowing in tetraplegia: a preliminary report. Spinal Cord. 2014 Dec;52(12):880-6.
Martin R, Sadowsky C, Obst K, Meyer B, McDonald J. Functional electrical stimulation in spinal cord injury: from theory to practice. Top Spinal Cord Inj Rehabil. 2012 Winter;18(1):28-33.
Warms CA, Backus D, Rajan S, Bombardier CH, Schomer KG, Burns SP. Adverse events in cardiovascular-related training programs in people with spinal cord injury: a systematic review. J Spinal Cord Med. 2014 Nov;37(6):672-92.
Image credits
- E-Stim Therapy ©Rankn Jordan, CC BY-NC-SA 2.0
- Functional electrical stimulation ©MilosRPopovic, CC BY-SA 4.0
- Image by SCIRE Community Team
- Checklist ©lastspark,CC BY 3.0 US
- Muscle © Smalllike, CC BY 3.0 US
- cardio ©emma Mitchell, CC BY 3.0 US
- Image by SCIRE Team.
- Image by SCIRE Team.
- fracture ©fahmionline, CC BY 3.0 US