
Author: Kelsey Zhao | Reviewer: Rachel Abel | Published: 26 February 2025 | Updated: ~
Key Points
- A good quality of life (QoL) is not uncommon for people with SCI. There is no relationship between injury level or severity and QoL.
- Involvement in the community through work, school, volunteer work, and social activities is associated with higher QoL.
- Social support from family, friends, peers, and the community is associated with higher QoL.
- The frequency of medical complications and how much they interfere with life reduces QoL.
- QoL can be impacted by the accessibility of the community, work, and home environments.

Quality of life (QoL) measures the different parts of an individual’s life to try and paint a picture of how well they are doing and how satisfied they are with their life. This might include things that an outsider could measure, like housing, income, employment, and health status. This can also include things that are based on an individual’s own values and aspirations, like whether they are satisfied with their current life and whether they feel their wants and needs are fulfilled.
QoL can be difficult to measure since individuals have different values and expectations for life. These values, expectations, and priorities can also change over an individual’s lifetime. Assessments used in research will not always accurately reflect how an individual weights different life components. QoL scores can also be influenced by regional differences in cultural values, access to care, and the accessibility of the surrounding environment.
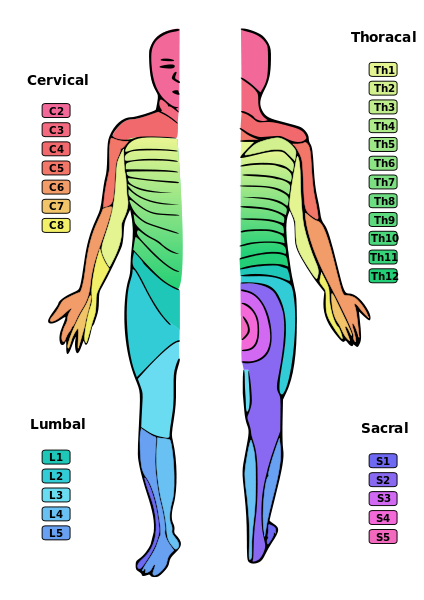
Contrary to popular belief, people with SCI generally have good QoL. On average, people with SCI score lower on QoL tests than the general population. However, a lower average does not mean that all people with SCI see their QoL as low, or that all people with SCI will have a lower score than people who do not have an SCI. In studies of people with cervical SCIs, the majority of participants felt that their QoL is average or better than average.
Most studies find little to no relationship between level of injury, injury severity, and QoL. Rather, higher QoL is limited by the physical and social barriers that prevent people from accessing community, activities, and employment.
 Employment
Employment
Numerous studies show that work is strongly related to higher QoL for people with SCI. This is true whether the person is working full-time, part-time, or in an unpaid position.
In a study that looked at the QoL of people with SCI in six different countries, employment was one of the only factors found to be associated with higher QoL regardless of location. One large study also found that satisfaction with life increased over time for people who were employed or students.
Is it hard to find suitable work with SCI?Differences in age, injury, work experience, and what is defined as work make it hard to pin down an exact number, but research estimates that about 35% of people with SCI are employed. The low rates of employment are likely due to a mix of personal and environmental factors. Physical and health limitationsAfter an SCI, job opportunities can be limited by physical impairments and health. For example, someone might not be able to return to the work they did before their injury because it is too physically demanding. Health complications related to SCI like pain and fatigue, and managing care routines can also limit energy and time, making it more difficult to work. Workplace environmentThat said, people with SCI are often underemployed even when they want to and are able to work. Finding suitable work can be difficult because of issues like lack of transportation, inaccessible workplaces, fear of losing financial or health benefits, and employer discrimination towards people with disabilities. This is extremely concerning because of the connection between work and QoL. There is evidence that workplace support and accommodations increase employment for people with physical disabilities. Local rehabilitation programs or SCI peer programs may have services to help people with SCI reach work and career goals. |
Community involvement
One study found that people with SCI felt they had a greater sense of community than the general population. Community involvement can include recreational activities, hobbies, and positions in community organizations and can contribute to a higher QoL.
Social support
 Social support refers to one’s relationships with other people, and the interactions, support, and care provided by this network of people, including family members, friends, and peer community. There is consistent evidence that more social support is linked to higher QoL in people with SCI.
Social support refers to one’s relationships with other people, and the interactions, support, and care provided by this network of people, including family members, friends, and peer community. There is consistent evidence that more social support is linked to higher QoL in people with SCI.
Social interaction and participation in social activities are also linked to higher QoL. In some studies, it has the highest positive impact on life satisfaction of all factors. Marriage/having a partner is found to either improve or have no effect on QoL.
Independence
Independence in personal care and transportation is associated with higher QoL. One large study found that life satisfaction increased over the years for people with SCI who lived independently.
Psychological factors
Feeling like you have control over your life was related to higher QoL in several studies. Research has also shown strong associations between symptoms of depression and anxiety and lower quality of life. The connection between QoL and psychological factors highlight the importance of mental health support and treatment in SCI rehabilitation.
Health complications
Having an SCI usually comes with additional health complications over one’s lifetime. These conditions can be directly or indirectly related to the SCI and could include:
- pain,
- urinary tract infections (UTIs),
- pressure ulcers,
- fatigue,
- problematic spasticity,
- bowel problems like constipation, hemorrhoids, etc.,
- bladder problems like leaking, kidney/bladder stones, etc.,
- and mental health conditions like depression, anxiety, and post-traumatic stress disorder.
Read our articles on the areas listed here and many other Topics!
The more health complications disrupt regular life, the greater the impact on QoL. For example, more frequent UTIs are associated with lower QoL as they limit daily activities and increase experiences of spasticity. How much pain interferes with life is also related to QoL. One study found that over a 2-year period, if pain interfered less with life over time, QoL increased, and vice versa. Pain also contributes to higher rates of mental health conditions for people with SCI, which are commonly associated with lower QoL.
Further, the more health conditions one experiences at once, the more QoL decreases. There is some evidence that when there are no health complications, the average QoL for people with SCI is similar to the average QoL of non-SCI populations.
Since community involvement and access to services is so important to QoL for people with SCI, access to the community environment can have a big effect on health and QoL. Many of the factors that hinder access can be improved by changing policies, practices, and the physical environment.

Community Access
Although accessibility features are required in many public places, what is accessible for one person may not be for another. The environment outside and inside can still be inaccessible to people with SCI for many reasons. Things like unmaintained sidewalks; physical barriers in parks, beaches, and swimming pools; a lack of adjustable equipment in a health care centre; and obstacles inside and outside of buildings, can prevent people with SCI from participating in the community and accessing health care. This lack of access to community spaces and resources can have a negative impact on QoL.
Housing Access
Not having suitable housing with adaptations for SCI can have a negative impact on QoL. Living in a home that hinders one’s ability to do daily activities or participate in activities can be very stressful. The inaccessible homes of family and friends can also affect QoL.
Read our article on Housing After SCI for more information!
Transportation Access
A lack of accessible transportation can lower QoL by blocking access to community resources, health care, and activities, especially for people in living in rural or remote areas. Owning a private adapted vehicle may be too expensive, not suited to one’s particular needs, or not available in the area. Public transportation like buses and trains are not always available or equipped to accommodate people with SCI.
Read our article on Adapted Driving for more information!
Regardless of injury level and severity, many people with SCI report that they have a good quality of life. QoL can be difficult to measure because everyone has their own priorities, values, and expectations for what they consider to be a good life.
Involvement in the community through work, school, volunteer work, and social activities are some of the factors that are most strongly related to higher QoL. Social support from family, friends, peers, and the community are also important for QoL.
The disruption caused by frequent and problematic medical complications can lower QoL. Seek medical care from a health professional if pain, fatigue, spasticity, bowel/bladder problems etc. are having a big negative impact on your daily life.
For a review of how we assess evidence at SCIRE Community and advice on making decisions, please see SCIRE Community Evidence.
Parts of this page have been adapted from the SCIRE Professional “Work and Employment” Module:
Escorpizo R, Smith EM, Finger ME, Miller WC (2018). Work and Employment Following Spinal Cord Injury. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, Sproule S, Querée M, Benton B editors. Spinal Cord Injury Rehabilitation Evidence. Version 6.0. p 1- 35.
Available from: scireproject.com/evidence/work-and-employment/
Evidence for “What is quality of life?” is based on:
Hammell, K. W. (2004). Exploring quality of life following high spinal cord injury: a review and critique. Spinal Cord, 42(9), 491–502. https://doi.org/10.1038/sj.sc.3101636
Sakakibara, B. M., Hitzig, S. L., Miller, W. C., & Eng, J. J. (2012). An evidence-based review on the influence of aging with a spinal cord injury on subjective quality of life. Spinal Cord, 50(8), 570–578. https://doi.org/10.1038/sc.2012.19
Theofilou, P. (2013). Quality of Life: Definition and Measurement. Europe’s Journal of Psychology, 9(1), 150–162. https://doi.org/10.5964/ejop.v9i1.337
Tate, D., & Forchheimer, M. (2014). Review of Cross-Cultural Issues Related to Quality of Life After Spinal Cord Injury. Topics in Spinal Cord Injury Rehabilitation, 20(3), 181–190. https://doi.org/10.1310/sci2003-181
Evidence for “Does spinal cord injury impact quality of life?” is based on:
Hill, M. R., Noonan, V. K., Sakakibara, B. M., & Miller, W. C. (2010). Quality of life instruments and definitions in individuals with spinal cord injury: a systematic review. Spinal Cord, 48(6), 438–450. https://doi.org/10.1038/sc.2009.164
Sakakibara, B. M., Hitzig, S. L., Miller, W. C., & Eng, J. J. (2012). An evidence-based review on the influence of aging with a spinal cord injury on subjective quality of life. Spinal Cord, 50(8), 570–578. https://doi.org/10.1038/sc.2012.19
Hammell, K. W. (2004). Exploring quality of life following high spinal cord injury: a review and critique. Spinal Cord, 42(9), 491–502. https://doi.org/10.1038/sj.sc.3101636
McColl, M. A., Arnold, R., Charlifue, S., Glass, C., Savic, G., & Frankel, H. (2003). Aging, spinal cord injury, and quality of life: structural relationships11No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit on the authors or on any organization with which the authors are associated. Archives of Physical Medicine and Rehabilitation, 84(8), 1137–1144. https://doi.org/10.1016/S0003-9993(03)00138-2
Olkin, R. (2022). Conceptualizing disability: Three models of disability. American Psychological Association. https://www.apa.org/ed/precollege/psychology-teacher-network/introductory-psychology/disability-models
Evidence for “What can increase quality of life for people with SCI?” is based on:
Lakhani, A., Parekh, S., Watling, D. P., Grimbeek, P., Duncan, R., Charlifue, S., & Kendall, E. (2022). Access and engagement with places in the community, and the quality of life among people with spinal cord damage. The Journal of Spinal Cord Medicine, 45(4), 522–530. https://doi.org/10.1080/10790268.2020.1860867
Geyh, S., Ballert, C., Sinnott, A., Charlifue, S., Catz, A., D’Andrea Greve, J. M., & Post, M. W. M. (2013). Quality of life after spinal cord injury: a comparison across six countries. Spinal Cord, 51(4), 322–326. https://doi.org/10.1038/sc.2012.128
Chen, Y., Anderson, C. J., Vogel, L. C., Chlan, K. M., Betz, R. R., & McDonald, C. M. (2008). Change in Life Satisfaction of Adults With Pediatric-Onset Spinal Cord Injury. Archives of Physical Medicine and Rehabilitation, 89(12), 2285–2292. https://doi.org/10.1016/j.apmr.2008.06.008
Nevala, N., Pehkonen, I., Koskela, I., Ruusuvuori, J., & Anttila, H. (2015). Workplace Accommodation Among Persons with Disabilities: A Systematic Review of Its Effectiveness and Barriers or Facilitators. Journal of Occupational Rehabilitation, 25(2), 432–448. https://doi.org/10.1007/s10926-014-9548-z
Ottomanelli, L., & Lind, L. (2009). Review of Critical Factors Related to Employment After Spinal Cord Injury: Implications for Research and Vocational Services. The Journal of Spinal Cord Medicine, 32(5), 503–531. https://doi.org/10.1080/10790268.2009.11754553
Trenaman, L., Miller, W. C., Querée, M., & Escorpizo, R. (2015). Modifiable and non-modifiable factors associated with employment outcomes following spinal cord injury: A systematic review. The Journal of Spinal Cord Medicine, 38(4), 422–431. https://doi.org/10.1179/2045772315Y.0000000031
Migliorini, C. E., New, P. W., & Tonge, B. J. (2011). Quality of life in adults with spinal cord injury living in the community. Spinal Cord, 49(3), 365–370. https://doi.org/10.1038/sc.2010.102
Helgeson, V. S. (2003). Social support and quality of life. Quality of Life Research, 12(1suppl), 25–31. https://doi.org/10.1023/A:1023509117524
Kashif, M., Jones, S., Darain, H., Iram, H., Raqib, A., & Butt, A. A. (2019). Factors influencing the community integration of patients following traumatic spinal cord injury: a systematic review. JPMA. The Journal of the Pakistan Medical Association, 69(9), 1337–1343.
Müller, R., Peter, C., Cieza, A., & Geyh, S. (2012). The role of social support and social skills in people with spinal cord injury—a systematic review of the literature. Spinal Cord, 50(2), 94–106. https://doi.org/10.1038/sc.2011.116
Chang, F.-H., Wang, Y.-H., Jang, Y., & Wang, C.-W. (2012). Factors Associated With Quality of Life Among People With Spinal Cord Injury: Application of the International Classification of Functioning, Disability and Health Model. Archives of Physical Medicine and Rehabilitation, 93(12), 2264–2270. https://doi.org/10.1016/j.apmr.2012.06.008
Jörgensen, S., Iwarsson, S., & Lexell, J. (2017). Secondary Health Conditions, Activity Limitations, and Life Satisfaction in Older Adults With Long‐Term Spinal Cord Injury. PM&R, 9(4), 356–366. https://doi.org/10.1016/j.pmrj.2016.09.004
van Leeuwen, C. M. C., Kraaijeveld, S., Lindeman, E., & Post, M. W. M. (2012). Associations between psychological factors and quality of life ratings in persons with spinal cord injury: a systematic review. Spinal Cord, 50(3), 174–187. https://doi.org/10.1038/sc.2011.120
García-Rudolph, A., Cegarra, B., Opisso, E., Tormos, J. M., & Saurí, J. (2021). Relationships Between Functionality, Depression, and Anxiety With Community Integration and Quality of Life in Chronic Traumatic Spinal Cord Injury. American Journal of Physical Medicine & Rehabilitation, 100(9), 840–850. https://doi.org/10.1097/PHM.0000000000001773
Parker, M. A., Ichikawa, J. K., Bombardier, C. H., & Hammond, F. M. (2022). Association Between Anxiety Symptoms, Depression Symptoms, and Life Satisfaction Among Individuals 1 Year After Spinal Cord Injury: Findings From the SCIRehab Project. Archives of Rehabilitation Research and Clinical Translation, 4(3), 100211. https://doi.org/10.1016/j.arrct.2022.100211
Evidence for “What can decrease quality of life for people with SCI?” is based on:
Andresen, S. R., Biering-Sørensen, F., Hagen, E. M., Nielsen, J. F., Bach, F. W., & Finnerup, N. B. (2016). Pain, spasticity and quality of life in individuals with traumatic spinal cord injury in Denmark. Spinal Cord, 54(11), 973–979. https://doi.org/10.1038/sc.2016.46
Ataoğlu, E., Tiftik, T., Kara, M., Tunç, H., Ersöz, M., & Akkuş, S. (2013). Effects of chronic pain on quality of life and depression in patients with spinal cord injury. Spinal Cord, 51(1), 23–26. https://doi.org/10.1038/sc.2012.51
Kemp, B., Tsukerman, D., Kahan, J., & Adkins, R. (2014). Predicting Psychosocial Outcomes Using a Brief Measure of Quality of Life in a Sample of People with Spinal Cord Injury. Topics in Spinal Cord Injury Rehabilitation, 20(3), 191–196. https://doi.org/10.1310/sci2003-191
Putzke, J. D., Richards, S. J., Hicken, B. L., & DeVivo, M. J. (2002). Interference due to pain following spinal cord injury: important predictors and impact on quality of life. Pain, 100(3), 231–242. https://doi.org/10.1016/S0304-3959(02)00069-6
Vogel, L. C., Krajci, K. A., & Anderson, C. J. (2002). Adults With Pediatric-Onset Spinal Cord Injury: Part 2: Musculoskeletal And Neurological Complications. The Journal of Spinal Cord Medicine, 25(2), 117–123. https://doi.org/10.1080/10790268.2002.11753611
Theisen, K. M., Mann, R., Roth, J. D., Pariser, J. J., Stoffel, J. T., Lenherr, S. M., Myers, J. B., Welk, B., & Elliott, S. P. (2020). Frequency of patient-reported UTIs is associated with poor quality of life after spinal cord injury: a prospective observational study. Spinal Cord, 58(12), 1274–1281. https://doi.org/10.1038/s41393-020-0481-z
Piatt, J. A., Nagata, S., Zahl, M., Li, J., & Rosenbluth, J. P. (2016). Problematic secondary health conditions among adults with spinal cord injury and its impact on social participation and daily life. The Journal of Spinal Cord Medicine, 39(6), 693–698. https://doi.org/10.1080/10790268.2015.1123845
Wijesuriya, N., Tran, Y., Middleton, J., & Craig, A. (2012). Impact of Fatigue on the Health-Related Quality of Life in Persons With Spinal Cord Injury. Archives of Physical Medicine and Rehabilitation, 93(2), 319–324. https://doi.org/10.1016/j.apmr.2011.09.008
Peterson, M. D., Meade, M. A., Lin, P., Kamdar, N., Rodriguez, G., Krause, J. S., & Mahmoudi, E. (2022). Psychological morbidity following spinal cord injury and among those without spinal cord injury: the impact of chronic centralized and neuropathic pain. Spinal Cord, 60(2), 163–169. https://doi.org/10.1038/s41393-021-00731-4
Wollaars, M. M., Post, M. W. M., van Asbeck, F. W. A., & Brand, N. (2007). Spinal Cord Injury Pain: The Influence of Psychologic Factors and Impact on Quality of Life. The Clinical Journal of Pain, 23(5), 383–391. https://doi.org/10.1097/AJP.0b013e31804463e5
Rivers, C. S., Fallah, N., Noonan, V. K., Whitehurst, D. G., Schwartz, C. E., Finkelstein, J. A., Craven, B. C., Ethans, K., O’Connell, C., Truchon, B. C., Ho, C., Linassi, A. G., Short, C., Tsai, E., Drew, B., Ahn, H., Dvorak, M. F., Paquet, J., Fehlings, M. G., & Noreau, L. (2018). Health Conditions: Effect on Function, Health-Related Quality of Life, and Life Satisfaction After Traumatic Spinal Cord Injury. A Prospective Observational Registry Cohort Study. Archives of Physical Medicine and Rehabilitation, 99(3), 443–451. https://doi.org/10.1016/j.apmr.2017.06.012
Burke, D., Lennon, O., & Fullen, B. M. (2018). Quality of life after spinal cord injury: The impact of pain. European Journal of Pain, 22(9), 1662–1672. https://doi.org/10.1002/ejp.1248
Evidence for “How does accessibility impact quality of life?” is based on:
Gurung, S., Jenkins, H.-T., Chaudhury, H., & Ben Mortenson, W. (2023). Modifiable Sociostructural and Environmental Factors That Impact the Health and Quality of Life of People With Spinal Cord Injury: A Scoping Review. Topics in Spinal Cord Injury Rehabilitation, 29(1), 42–53. https://doi.org/10.46292/sci21-00056
Image credits
- Two people sitting outside ©SCIRE, CC BY-NC 4.0
- Sam Sullivan https://samsullivan.ca/photo-gallery/
- Mother in wheelchair with child ©SCIRE, CC BY-NC 4.0
- Elderly man in wheelchair cityscape ©SCIRE, CC BY-NC 4.0

 Employment
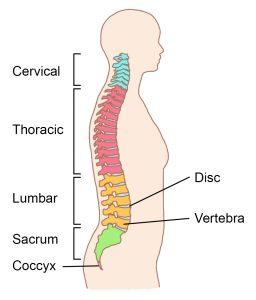
Employment Congenital NTSCIs are developmental defects, malformations, and abnormalities affecting the spinal cord which are present at birth. An infant can have one congenital condition, or multiple conditions at the same time. For example, Type 2 Chiari malformations almost always occurs in association with myelomeningocele, a severe form of spina bifida
Congenital NTSCIs are developmental defects, malformations, and abnormalities affecting the spinal cord which are present at birth. An infant can have one congenital condition, or multiple conditions at the same time. For example, Type 2 Chiari malformations almost always occurs in association with myelomeningocele, a severe form of spina bifida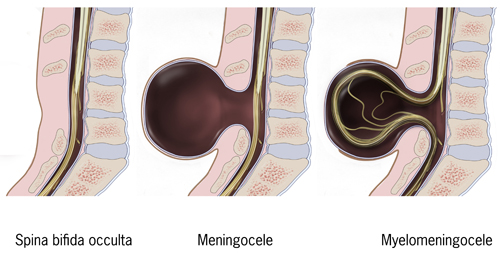

 An estimated 20.6 million individuals live with SCI globally. It appears that the incidence of NTSCI is increasing due to the ageing population in many countries. Indeed, in some countries the incidence of NTSCI is now higher than that of traumatic SCI.
An estimated 20.6 million individuals live with SCI globally. It appears that the incidence of NTSCI is increasing due to the ageing population in many countries. Indeed, in some countries the incidence of NTSCI is now higher than that of traumatic SCI.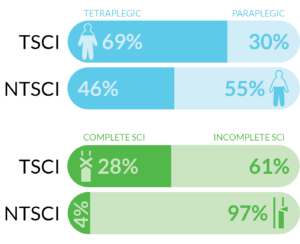

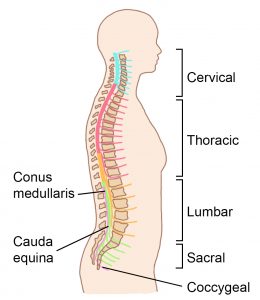

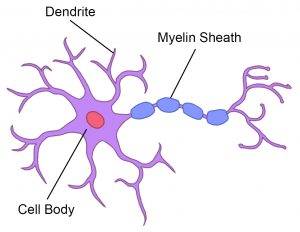
 The spinal cord provides a pathway for movement commands to travel from the brain to the muscles. This is called motor function. Neurons that send movement commands are called motor neurons.
The spinal cord provides a pathway for movement commands to travel from the brain to the muscles. This is called motor function. Neurons that send movement commands are called motor neurons.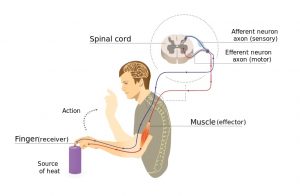
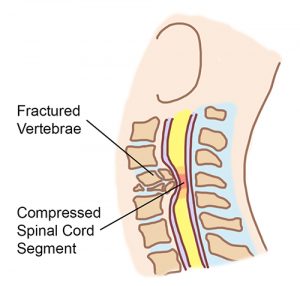
 Spinal shock happens right after injury and causes the muscles below the injury to be floppy and unmoving (called flaccid paralysis). This happens because the spinal reflexes below the injury are temporarily impaired in response to the injury. Spinal shock often happens together with neurogenic shock.
Spinal shock happens right after injury and causes the muscles below the injury to be floppy and unmoving (called flaccid paralysis). This happens because the spinal reflexes below the injury are temporarily impaired in response to the injury. Spinal shock often happens together with neurogenic shock.

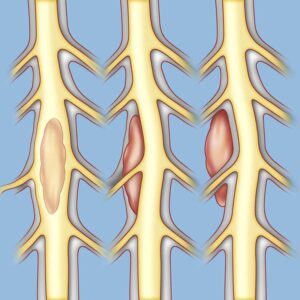
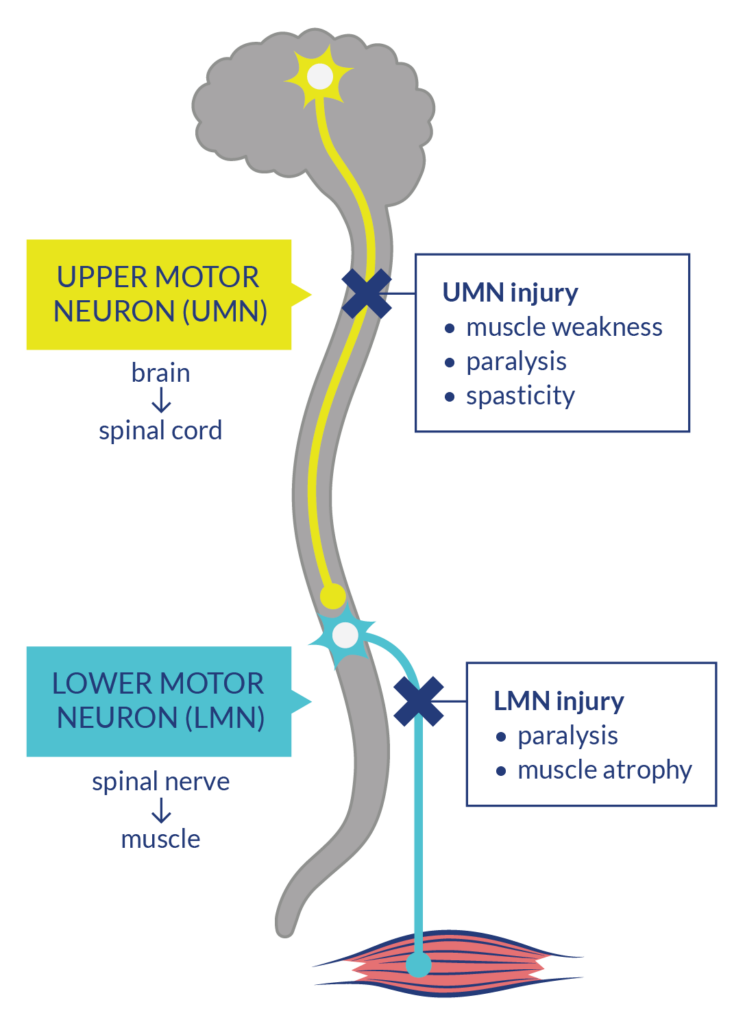 Nerve pathways that send movement commands from the brain to the muscles are made up of two types of neurons: upper motor neurons (UMNs) which start in the brain and go down the spinal cord, and lower motor neurons (LMNs) which connect to the UMN in the spinal and go out to the muscles.
Nerve pathways that send movement commands from the brain to the muscles are made up of two types of neurons: upper motor neurons (UMNs) which start in the brain and go down the spinal cord, and lower motor neurons (LMNs) which connect to the UMN in the spinal and go out to the muscles.
 Although not specifically describing level of injury, tetraplegia and paraplegia are terms used to describe the extent of a spinal cord injury’s effects on the body.
Although not specifically describing level of injury, tetraplegia and paraplegia are terms used to describe the extent of a spinal cord injury’s effects on the body.
