Contributors: Breastfeeding Consumer Guide for Mothers Panel | Published: 11 January 2022 | Updated: ~
Few resources exist that talk about the effects a spinal cord injury (SCI) can have on breastfeeding. It is difficult to find information about the unique questions, challenges, or concerns women with SCI experience when planning or trying to breastfeed.
Our team, which includes women with SCI, health care providers, and SCI researchers, came together to create a guide to help address this information gap.
The purpose of this guide is to share with you the most common issues women with SCI experience during breastfeeding. This guide also provides information, practical suggestions, recommendations, and key resources.
General information about breastfeeding is available on the internet, in books, or from your friends and health care providers. We did not plan to repeat or replace general breastfeeding information or medical advice. Rather, we hope this guide adds to this information by sharing facts, tips, and resources specifically related to breastfeeding after SCI.
Breastfeeding in women with SCI is complex and requires a team of health care providers with complementary expertise. Such a team can include: your family physician, obstetrician, physiatrist, neurologist, occupational therapist, physical therapist, lactation consultant, midwife, psychologist, peer counsellor etc. Your team will vary depending on where you live.
We hope that you find this guide helpful.
Key Points
- Breastfeeding has many benefits for babies’ physical, developmental, and emotional health regardless of whether the breastfeeding mother has SCI or not.
- Some women with SCI may experience unique challenges and barriers that can impact how they breastfeed or if they can continue to breastfeed. This can sometimes result in women with SCI feeling alone, lost, or as if they have failed.
- It is important for every woman to feel supported as she explores how best to balance her own unique needs and abilities with the known benefits and risks of the various ways to feed her child (breastfeeding, supplementing, and/or formula feeding).
 It is accepted that breast milk (colostrum, transitional milk and mature milk) is the first choice to help your baby grow and develop. The benefits for your baby include:
It is accepted that breast milk (colostrum, transitional milk and mature milk) is the first choice to help your baby grow and develop. The benefits for your baby include:
- Providing the ideal nutrition (breast milk has the perfect amount of protein, carbohydrates, fat, vitamins, and minerals, and is easy to digest),
- Providing antibodies to protect against illness while baby’s immune system develops,
- Lowering the likelihood of obesity, diabetes, and other diseases developing in childhood,
- Lowering infant mortality.
The benefits for mothers include:
- Increasing bonding and relaxation,
- Reducing costs,
- Having the convenience of breastmilk available,
- Lowering the risk of future breast and ovarian cancers.
If breastfeeding is not possible or not enough breast milk is produced by mothers with SCI, then feeding with formula or donated breast milk from a milk bank is both necessary and encouraged.
Refer to the Public Health Agency of Canada’s 10 Great Reasons to Breastfeed Your Baby and the World Health Organization Infant and Young Child Feeding chapter for more information.
 Women with SCI, just like women without SCI, are encouraged to give breastfeeding a try. By trying, you can then see how it works for both you and for your baby. If breastfeeding does not work well, there are several safe and healthy options available to you to ensure both your needs and your baby’s needs are met.
Women with SCI, just like women without SCI, are encouraged to give breastfeeding a try. By trying, you can then see how it works for both you and for your baby. If breastfeeding does not work well, there are several safe and healthy options available to you to ensure both your needs and your baby’s needs are met.
Many of the main questions and concerns women with SCI have shared with us are outlined in this guide. The information, recommendations, and resources below are intended to help you to gather information, to help guide your breastfeeding planning, to help you to problem solve common challenges or to help you to explore new ways of doing things as you work to find a feeding plan that is the right fit for you and your baby.
Recommendations:
- You are encouraged to try to breastfeed and see how it goes for you and your baby.
- If you have challenges or questions about breastfeeding talk to your health care providers. You may wish to share with them a copy of this resource guide to discuss together.
Everyone is different and it is not possible to predict your ability to produce breast milk and breastfeed your baby. Some challenges during breastfeeding are similar between women with and without SCI. However, it is important to recognize that mothers with SCI face additional concerns during breastfeeding related to SCI.
Depending on their level of injury, women with SCI could have limited milk production, difficulties with positioning and latching their baby, and they may experience episodes of autonomic dysreflexia (AD), an abrupt and often dangerous spike in blood pressure.

Watch SCIRE’s video explaining breastfeeding complications after SCI.
Research shows that the higher and more complete the injury, the more likely difficulties will occur. Yet, with the right supports in place, you can define what successful breastfeeding means to you.
Recommendations:
- Talk to your health care providers, including a lactation consultant and a physiatrist for more information on how your SCI may be impeding breastfeeding.
- Review this guide and references for additional information.
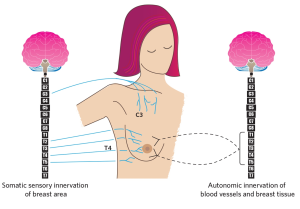
Figure 1. The innervation (control) of the breast by somatic (voluntary) and autonomic (involuntary) nervous systems. The black lines show the autonomic nerves (T1-T5 spinal cord levels) innervating breast tissues and blood vessels. The blue lines show the cervical (C) and thoracic (T) segments of the spinal cord that affect sensory control of the breast and nipple area. Milk production is a result of the coordinated functioning of the somatic and autonomic nervous systems.
The ability to breastfeed could be affected by the level and completeness of your SCI.
First, if your injury is above the first thoracic (T1) spinal cord level the motor functions in your arms/hands could be affected and you could have trouble with positioning and holding your child during breastfeeding. Typically, women with tetraplegia (cervical spinal cord injuries) experience these difficulties (see section on positioning and aids below).
Second, if your injury is above the fifth thoracic (T5 spinal) cord level, this could result in decreased or loss of sensory control of area of the nipple/breast area and affect milk production. These levels of injuries could result also in decrease or loss of body responses that occur during breastfeeding that are important for milk production (physiological reflexes known as “let down reflex”) (See Figure 1)

Watch SCIRE’s video highlighting Sheryl’s experience breastfeeding with a T2-T7 Incomplete SCI.
Recommendation:
Discuss your level of SCI and potential for breastfeeding with medical professionals (such as a physiatrist) and support team before planning a pregnancy or before delivery.
Like all mothers, women with SCI may experience common breastfeeding challenges such as:
- babies who have difficulty latching/feeding due to issues like prematurity, tongue tie, or jaundice
- mothers with inverted nipples, infection (clogged ducts, mastitis) or an overabundance of milk
There are also additional considerations specific to SCI that can cause some challenges in latching such as sensory changes, motor effects, and fatigue.
Be aware that sensory changes in your body caused by SCI could affect your ability to breastfeed. If you have decreased nipple sensation, it may lead to altered let-down reflex and impaired milk production as well as limit the ability to recognize poor latch. Visual signs during latching, feeding, and immediately after the feeding can help mothers identify a good latch. Use a mirror or have someone check the latch during the feeding and the breast for abrasions after feeding. During feeding, you should notice that your baby is changing the rate of sucking and appears to be swallowing. After feeding, you should check the condition of your nipples and if your baby appears to be satisfied.
Be aware that strength and ability to move your upper extremities could impact your ability to breastfeed. Lack of mobility in your arms/hands, spasms, and impaired trunk strength or balance can affect how well the baby is positioned to access the breast, to get and keep a good latch that does not injure your nipples, and to reposition when needed. If you have poor hand function it may be difficult to express your milk for drainage to prevent infection (clogged ducts and mastitis). Ineffective or infrequent feeding can also be a cause of inadequate milk production. See positioning and aids section below for ideas during breastfeeding.
Be aware that fatigue is common in people with SCI and could impact your ability to breastfeed successfully. Having a new baby is intense and requires around the clock attention and care for everyone. For some mothers with SCI, your own requirements for care may conflict with or delay the feeding times of your baby. You may want to create a feeding plan with support from your spouse, partner, family, or aide to assist in the feeding schedule. Make sure you continue to assess the latching, feeding, and breast health for as long as you decide to breastfeed. Remember that there is education and support out there for you if you need it. See section below on community supports.
Recommendations:
- Pay attention to your baby’s quality of latching and swallowing during breastfeeding, particularly if you have decreased sensation in your nipples and breast area.
- Examine your nipples (either on your own or ask a care provider to assist you) before and after breastfeeding to look for nipple distortion.
- Consult with your health care team if you are having a hard time positioning your baby to breastfeed. They may be able to assist or can refer you to a knowledgeable health care provider such as an occupational therapist or physiotherapist to help you explore assistive aids.
- If you are experiencing fatigue that interferes with your activities and breastfeeding, ask for the support of health care provider (e.g., occupational therapist) for suggestions and energy saving recommendations.
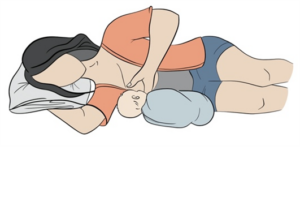
There are many things to consider in choosing a position for breastfeeding and skin-to-skin contact with baby. Your level of injury, fatigue, spasticity, hand function, trunk stability, and time of day can influence if you choose to be in bed, in your wheelchair, or in a different chair to breastfeed. It may also be necessary to have someone else pick up your baby and position them for feeding. The figure below shows the most used positions during breastfeeding by women with SCI.
Figure 2. Alternative breastfeeding positions that may be adapted for women with SCI.

Watch SCIRE’s video explaining ways you can breastfeed with assistive aids.
Recommendations:
- If you are having difficulties with positioning your baby during breastfeeding ask for the support from your health care providers (e.g., occupational therapists, physical therapists).
- Wheelchair modifications may be required to provide additional trunk support to increase stability while lifting and holding your baby. Adjusting the seat slope or backrest angle can change centre of gravity and improve stability. A backrest with deeper lateral trunk support or the use of a chest strap may also add stability. Changing the position of sideguards or widening the chair can allow for more room for baby’s body and legs when held in football or cross cradle positions.
- Wedges can provide support for sitting upright in a bed (providing support for the back, belly or the infant after birth), or be used as leg support to reduce spasms and improve blood pressure.
- Carriers (harnesses, wraps, ring slings) can be used during breastfeeding and thereafter. They may be useful in positioning your baby when bottle-feeding or using a supplementary nursing system and can help to keep them upright after a feed to reduce spit-up/reflux.
- Breastfeeding pillows are available in a variety of shapes, weights and stiffness (firm versus lighter and more flexible). Some mothers find that their own regular pillows work well if the breastfeeding pillows do not provide enough support.
Adding a long waist strap to a breastfeeding pillow or infant carrier that also wraps around the wheelchair backrest, can give added security, and reduce the tendency for the pillow to slide forward or for you to lean forward while holding the weight of the infant in front.

Watch SCIRE’s video highlighting Nicole’s breastfeeding experience.
Many mothers worry about low breastmilk supply and that their baby will not get enough milk. If you have low milk supply, there are a few different options you could consider. You may wish to supplement your baby with breast milk (your own or donated), or formula by bottle or by using supplementary nursing system (SNS). This system works by placing one end of a very thin flexible tube into a formula bottle, taping the tube to your breast, and slipping the other end of the tube into the baby’s mouth once they have latched.
Refer to the Sikana Health video covering “How to use a Supplemental Nursing System” for more information.
Recommendations:
 Talk to your health care providers, including lactation consultant and paediatrician about the most safe and effective options for feeding your baby, as well as medications for you and your baby.
Talk to your health care providers, including lactation consultant and paediatrician about the most safe and effective options for feeding your baby, as well as medications for you and your baby.- If you have enough hand function, you can express milk directly into your baby’s mouth. Additionally, a breast pump can be used to express the milk into a bottle and then to feed your baby.
- If you have low milk supply, you can start by feeding your baby from your breast then switching to a bottle after a specific amount of time or once the milk is gone from the breast.
- You can feed your baby at the breast with additional formula by using a supplementary nursing system.
Many women experience clogged milk ducts or even lactation mastitis (an inflammation of breast tissue that may or may not involve an infection, but causes breast pain, swelling, warmth, fever, or chills) during their breastfeeding experience. Breast lumps are not uncommon.
Depending on the level of injury and hand function women with SCI could be more likely to experience clogged ducts during breastfeeding. This happens when the breast is not fully emptied of milk at each feeding due to incomplete latching and suckling.
Breast health may also be compromised if the baby is not held well to the breast due to limited hand and arm function or muscle fatigue. Limited hand function may also lead to poor milk expression and limit the ability to perform self-lymphatic drainage and massage, which can contribute to the development of clogged ducts and mastitis.
Recommendations:
- Wear a supportive bra (even at night) but avoid restrictive clothing.
- Change damp or soiled breast pads often.
- Shower daily and wash nipples with clear water only (no soap).
- Eat a healthy diet and stay well hydrated.
- Use gentle breast massage (If hand function is limited, a massaging device could be used, or assistance requested from partner or caregiver).
- Alternate use of hot and cold compresses may be helpful if your breasts are engorged.
- If you have mastitis, check with your health care provider how you can safely continue to breastfeed your baby.
- Be aware that pain from breastfeeding and mastitis could cause AD.
Refer to the Penn Medicine article on General Breast Health as well as the Cleveland Clinic article on Care for Mastitis for more information!
The common medications used in women with SCI could go through the blood milk barrier into the milk, and many effects of medication on breastfeeding babies are not known. Speak with your health care team as each drug will need to be assessed of its risks compared to its benefits for you and for your baby.
The American Pediatric Association has suggested some medication tips around breastfeeding for all women, which we have quoted below:
Breastfeeding and Medication Tips
 Many effects of medications on breastfeeding babies simply are not known. Due to this, only take a medication when absolutely needed, at the lowest dose, and for the shortest time possible.
Many effects of medications on breastfeeding babies simply are not known. Due to this, only take a medication when absolutely needed, at the lowest dose, and for the shortest time possible.- When possible, take medications that are given only once a day right after a feeding when your baby will have the longest period without nursing; for many women this is the last feeding of the night before the baby’s bedtime.
- Watch your baby for side effects such as sleepiness, irritability, other potential or known reactions of the medication.
- Avoid long-acting, extended-release, and combination forms of medications when possible. Shorter-acting medications are removed from your body more quickly, and single medications give you greater flexibility in dosing.
- Only water-soluble cream or gel products should be applied to the breast because ointments may expose the baby to high levels of mineral paraffins via licking.
- Special precautions may be needed in preterm (premature) babies, due to their size and organ systems that are even less developed than a regular term baby.
- Ask your doctor about the risks and benefits of any medication prescribed while you are breastfeeding, or any medication you choose from over-the-counter options that do not require a prescription.
- When more than one medication or a combination medication is used, follow the breastfeeding recommendations for the most problematic medication.
Recommendation:
Consult your health care team for advice about what medications to use, adjust, or discontinue while breastfeeding.
Refer to LactMed, a database containing information on drugs and other chemicals which breastfeeding mothers may be exposed to, as well as Drugs.com for information on safe medications during breastfeeding.

Watch SCIRE’s video explaining Kristen’s experience of blood pressure drops while breastfeeding her daughter.
AD is identified by uncontrolled and potentially life-threatening spikes in arterial blood pressure, which may reach as high as 300 mmHg systolic blood pressure. It is common for people with SCI at or above the T6 spinal cord segment to experience episodes of AD that can be caused by painful or non-painful stimuli below the injury level. Episodes of AD have been documented in several studies of breastfeeding by women with higher level injuries. In women with SCI at or above the fourth thoracic segment (T4, level of sensory innervation of nipples),
episodes of AD could be specifically triggered by stimuli from the nipples/breast area during breastfeeding. You should be aware that an episode of AD could be accompanied by severe headaches, sweating, and heart palpitations or you could experience AD without any symptoms at all.
Breastfeeding-related AD may be caused by breastfeeding itself as well as mastitis, nipple fissures or other painful processes originating from the breast. Episodes of AD caused by breastfeeding may be much more common than we know. Recent research shows that one quarter of women with SCI experience AD while breastfeeding, and this number is higher in women with high level SCI (almost 40%).
Frequent and uncontrolled episodes of AD could result not only in discomfort, but also significant negative health consequences, including damage to blood vessels and heart, stroke, seizures, and even death. It is vital to prevent and manage AD in a timely manner. Unfortunately, this topic is not commonly discussed in postpartum care, but it is vital to recognize and address.
Recommendations:
- Be sure to discuss with your medical practitioner (physiatrist/ family physician/nurse) your blood pressure management and potential for development of AD.
- Be aware that women with SCI at or above T6 are at higher risk for the development of AD triggered by breastfeeding, clogged ducts/mastitis.
- If you experience symptoms of AD, you should stop breastfeeding and measure your blood pressure if you can. Be sure that you are in seated position with your legs lowered. Wait until symptoms subside and your blood pressure goes down close to normal before you resume breastfeeding.
- Be aware that prolong seating while breastfeeding may cause a decrease in your blood pressure (orthostatic hypotension), that could result in light-headedness and dizziness. If this will occur, elevate your legs, or change your position to horizontal.
- Have a wallet information card on AD in case of admission to an emergency room.
Refer to the ABC’s of Autonomic Dysreflexia and the Fact Sheet on AD by Spinal Cord Model System for more information.
To download a Automatic Dysreflexia wallet card, click here.
 Bonding, or what is often called ‘attachment’ or the ‘caring connection’ between a child and parent, is an important part of a child’s physical and emotional development. Some parents report immediately feeling a strong connection with their child during pregnancy or soon after the birth. Other parents report they did not feel an instant connection. Both feelings are okay and normal.
Bonding, or what is often called ‘attachment’ or the ‘caring connection’ between a child and parent, is an important part of a child’s physical and emotional development. Some parents report immediately feeling a strong connection with their child during pregnancy or soon after the birth. Other parents report they did not feel an instant connection. Both feelings are okay and normal.
Bonding and attachment can sometimes happen right away and can sometimes take weeks or months of getting to know and understand your baby to find what works best for you and your child and each of your unique needs.
Breastfeeding is not the only way to nurture or bond with your child. There are many other important ways to build connection and attachment between you and your baby.
Recommendations:
- Find times to hold your baby against your bare skin. There are many positive benefits including body temperature regulation, breathing and heart rate regulation, hormone release for both you and the child, calming, and improved sleep.
- Cuddle with your child. Ensure you have the chance to hold, rock, or carry your child during times that are not only related to feeding, bathing, diaper changes or consoling. Sometimes those quiet moments are really important moments of connection and affection.
- Respond to your baby when they cry. This may be by gently touching their skin, picking them up or by using your voice. Let your baby know you are nearby and aware of their needs.
- Talk to your baby throughout the day. It might feel awkward at first but tell stories, describe people and the world around them, talk about what you are doing, or sing to your child.
- Look into your newborn’s eyes while you feed or care for your child. This helps your newborn to connect your face with your sounds and actions.
- Find ways to soothe yourself as well as your child. Take a few deep breaths. Listen to music you enjoy. Visit with friends you feel comfortable with. Look at a picture of a place where you like to spend time. Babies pick up on adults’ feelings of tension and anxiety but also soak up their feelings of calm and comfort.
 Why am I feeling so sad or anxious?
Why am I feeling so sad or anxious?
The first few weeks after birth are exciting and challenging. It is a time of big changes as you bring your infant home, get to know them, learn how to feed, bathe, and carry them. You also need to adjust to disrupted sleep patterns, manage your physical recovery after the birth, and try to find time for your own daily living and self-care needs (such as eating, dressing, toileting, bathing, etc.). Breastfeeding when you have a SCI can sometimes make some, or all, of these
activities feel more challenging.
You may feel joy and excitement, but also feel sad, worried, or just be overwhelmed. This is understandable in the first few weeks after birth for any mother. This roller coaster of emotions is sometimes called “baby blues” and typically lasts a few days or up to a week or two. However, if the difficult feelings last longer and begin to impact your ability to participate in day-to-day activities, this can be a sign of what is called Postpartum Depression. Postpartum Depression can involve feeling sad, down, or crying easily but it can also sometimes feel like being worried, agitated, anxious, or an overwhelming fear that something awful is about to happen. Women with SCI are at higher risk for Postpartum Depression and anxiety due to several factors including:
- Mental health concerns prior to pregnancy,
- The stress of coping with multiple physical challenges during pregnancy and/or after the birth,
- Worry about other peoples’ opinions or judgments,
- Struggling with pre-existing fatigue related to SCI and the extra energy required to complete routine tasks as well as new onset fatigue due to baby caregiving needs,
- Limited access to knowledgeable caregivers or peers who understand the unique joys and challenges of parenting with a SCI,
- Possible other factors we do not yet know or understand.
Whatever you are feeling, you are not alone. You are important and valued. Help is available. Talk to your partner, loved ones, or health care providers about your feelings and worries. If needed, immediate help is available 24/7 from local crisis phone lines, Urgent Care Centres or Emergency Departments. With support, many women soon begin to feel their mood improve, their anxiety lessen, feel more attached to their baby, and begin to experience many more positive moments of parenting as they learn tools to help cope with the hard times.
Recommendations:
- Learn about the signs, symptoms, and resources related to postpartum depression and anxiety, so you, your partner, your family, and your care aides will recognize when extra assistance may be necessary.
- Talk to your health care providers, seek out information from trusted websites online or connect with local community groups that support new parents.
- Share this information with your partner, a friend or a family member, or a health care provider during your pregnancy or after baby has arrived. Sometimes we need a bit of help to reach out for the services we need when we are feeling sad or anxious.
- Watch your mood during pregnancy and after birth and notice any changes in feelings of sadness or worry. Are these feelings improving or getting worse? Are they lasting longer than they did in the past?
- Know that feelings of sadness or anxiety happen to lots of people. You are not a failure and you are not alone.
- Help is available 24/7. Accessing help can relieve pressure and often make a big difference in how you are feeling.
There are plenty of books on pregnancy, birth, and all the challenges with motherhood, but there is much less information for pregnant women and new mothers that have a SCI. Just like experiencing and learning about changes to your body during pregnancy, it is important to educate and advocate for yourself about being a mother and breastfeeding with a SCI.
Recommendations:
- Look to your healthcare team: Your healthcare team involved in your pregnancy and birth is your primary trusted resource. Physiatrists have the medical knowledge to address concerns related to your SCI. Lactation consultants, midwives and staff of public health agencies have knowledge about pregnancy, birth and breastfeeding. These professionals, working together with you can address your specific concerns.
- Look online for resources: In addition to information provided in this guide and if you don’t have services locally, look for reputable and accredited sources. Check your local or national Spinal Cord Injury organizations. There are many dedicated websites in the medical community. Do an online internet search with some key words like “mom SCI and breastfeeding”. Online videos, articles and peers’ stories provide opportunities for learning and connections among a growing population of moms with a SCI all around the world.
- Connect with other moms: Peer support is important for all new moms, including moms with SCI. Social media platforms like Facebook have many groups you could join and are a popular place to share questions and concerns and learn about equipment or adaptations ideas.
- Stay connected: We also know there is a risk of isolation. Currently, there is no way to fully prevent depression or anxiety postpartum but knowing what signs to watch for can be helpful. It’s important to stay connected and not isolated. First, you’re a new mom and that means you share a lot of the same emotions, concerns, and challenges as every new mother. Reach out to other moms in your community or online for advice, support and joint activities, especially nature and outdoor; there are more things in common with able-bodied moms once issues around your SCI are addressed.
Image credits
- Smiling Mother Playing With Her Baby Lying On The Floor ©Jacob Lund Photography from NounProject.com
- Newborn Being Breast-fed At Home ©Paulo Sousa from NounProject.com
- Complications ©SCIRE
- Kristen’s breastfeeding story ©SCIRE
- Breastfeeding innervation © The Krassioukov Lab
- Sheryl’s breastfeeding story ©SCIRE
- Breastfeeding Lying down ©SCIRE
- Breastfeeding positions ©The Krassioukov Lab
- Assistive Aids ©SCIRE
- Nicole’s breastfeeding story ©SCIRE
- Woman Bottle Feeds A Newborn ©Paulo Sousa from NounProject.com
- Medication © Kiran Shastry from Noun Project
- Close Up Of Smiling Mother And Baby Daughter ©Noun Project from NounProject.com
- Mother Taking Rest Sleeping On A Couch With Her Baby On Her Chest ©Jacob Lund Photography from NounProject.com
Panel Members
Andrei Krassioukov, MD, PhD, FRCPC
Physiatrist
GF Strong Rehabilitation Centre
Professor of Medicine
Division of Physical Medicine & Rehabilitation
University of British Columbia
Vancouver, British Columbia, Canada
Stacy Elliott, MD
Sexual Medicine Physician
Clinical Professor
Departments of Psychiatry and Urologic Sciences
University of British Columbia
Vancouver, British Columbia, Canada
Shea Hocaloski, RN, BTechN
Sexual Health Clinician
GF Strong Rehabilitation Centre
Vancouver, British Columbia, Canada
Olga Krassioukov-Enns, MD
Independent Living Consultant
Principal Researcher, “Axioms of Inclusion”
Winnipeg, Manitoba, Canada
Karen Hodge, MSW, RCSW
Clinical Social Worker, Mother with SCI
Sunny Hill Health Centre/
Adaptability Counselling and Consultation
Vancouver, British Columbia, Canada
Stephanie Gillespie, RN, IBCLC
Lactation Consultant
BC Women’s Hospital
Vancouver, British Columbia, Canada
Sherry Caves
Consumer Consultant
Vancouver, British Columbia, Canada
Teri Thorson
Consumer Consultant
Vancouver, British Columbia, Canada
Marina Green, RN, MSN, IBCLC
Lactation Consultant
BC Children’s and Women’s Health Centre
Vancouver, British Columbia, Canada
Lindsay Alford, BSc OT
Occupational Therapist
GF Strong Rehabilitation Centre
Vancouver, British Columbia, Canada
Melanie Basso, RN MSN PNC(C)
Senior Practice Leader Perinatal at BC Women’s
Vancouver, British Columbia, Canada
Laura McCracken, MSc
Clinical Research Coordinator
International Collaboration on Repair Discoveries
The University of British Columbia
Vancouver, British Columbia, Canada
International Contributors
Kim Anderson, MD
Director
Northeast Ohio Regional SCI Model System, MetroHealth Rehabilitation Institute Professor Department of Physical Medicine and Rehabilitation, MetroHealth Medical Center and Case Western Reserve University School of Medicine, Cleveland, United States
Elena Andretta, MD
Urologist – highly specialized in neuro-urology and bladder dysfunctions
Department of Urology, Dolo Hospital, Venice, Italy
Harvinder Singh Chhabra, MD
Chief of Spine Service & Medical Director
Indian Spinal Injuries Centre, New Delhi, India
Claes Hultling, MD, PhD
Associate Professor, Karolinska Institutet
CEO, Spinalis Foundation, Stockholm, Sweden
Christina-Anastasia Rapidi, MD, PhD
Head of Physical & Rehabilitation Medicine Department
General Hospital “G.Gennimatas”, Athens, Greece
Fin-Biering Sørensen, MD
Clinical Professor, University of Copenhagen Senior consultant, Clinic for Spinal Cord Injuries, Rigshospitalet, Denmark
Ineta Zobina, MD
Specialty doctor in spinal rehabilitation, Welsh Spinal Cord Injury Rehabilitation Centre (WSCIRC), Cardiff, United Kingdom
Francois Theron, MD
Medical Director, Muelmed Rehabilitation Centre: Orthopedic surgeon and lecturer, Department of Orthopedic Surgery, University of Pretoria, Pretoria, South Africa
International Reviewers
Allison Kessler, MD, MSc
Assistant Professor Department of PM&R Northwestern University Feinberg School of Medicine and Section Chief, Renée Crown Center for Spinal Cord Innovation, Chicago, IL, USA
Frederique Courtois PhD
Professor, Department of Sexology, Universite du Québec à Montréal, Montreal, QC, Canada
Maryam Berri, MD
Clinical Assistant Professor in the Department of Physical Medicine and Rehabilitation at the University of Michigan Medical School, Ann Arbor, MI, USA
This work was supported by the Craig Neilson Foundation Creating Opportunity and Independence Grant through “Breastfeeding and Spinal Cord Injury: Establishing Guidelines for Health professionals and Consumers” project lead by Dr. Andrei Krassioukov, ICORD, UBC.
We also would like to recognize the expertise and assistance of the panel members, reviewers, project participants and staff, whose contribution was integral to the development of this document.





 Talk to your health care providers, including lactation consultant and paediatrician about the most safe and effective options for feeding your baby, as well as medications for you and your baby.
Talk to your health care providers, including lactation consultant and paediatrician about the most safe and effective options for feeding your baby, as well as medications for you and your baby. Many effects of medications on breastfeeding babies simply are not known. Due to this, only take a medication when absolutely needed, at the lowest dose, and for the shortest time possible.
Many effects of medications on breastfeeding babies simply are not known. Due to this, only take a medication when absolutely needed, at the lowest dose, and for the shortest time possible.