Authors: Vanessa Mok, Dominik Zbogar | Reviewers: Janet Parker, Gita Joshi | Published: 23 December 2019 | Updated: ~
Adequate fibre intake is important to ensure proper nutrition after spinal cord injury (SCI). This page outlines the current recommendations for dietary fibre and its role in managing conditions such as neurogenic bowel in SCI.
Key Points
- Foods such as vegetables, fruits, legumes, and whole grains are great sources of dietary fibre.
- Research in the general population shows that increasing dietary fibre reduces the risk for heart disease, obesity, diabetes, high blood pressure, and certain cancers.
- Increasing dietary fibre in people with SCI may not have the same result as in the general population. It is important to continuously monitor how an increasing fibre intake affects you.
- Increasing fibre in the diet should be done incrementally and may require increased fluid intake to prevent constipation.
- An increased fibre intake may require a change in your bowel and bladder routine.
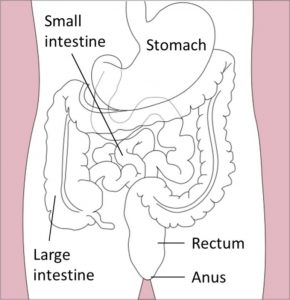
Dietary fibre is a kind of carbohydrate that is difficult for the body to break down, so it is not absorbed in the small intestines. Instead, it passes into the colon. Therefore, fibre supplies little to no calories.
Fibre can be classified into two types: soluble and insoluble. Both types of fibre play an important role in gut health and prevention of various health issues. Soluble fibre mixes with water in the intestine to form a gel-like substance that traps certain body wastes and moves them out of the body. Soluble fibre also decreases cholesterol, helps control blood sugar fluctuations, and feeds the good bacteria in the gut. Insoluble fibre absorbs and holds water, producing bulkier and uniform stool which helps with bowel movements, and it reduces the risk of colon cancer and diverticulitis among other benefits. Whole plant foods and fungi contain both types of fibre in varying amounts while animal food products contain no fibre.
When the spinal cord is injured, some or all of the nerve signals that would normally allow the brain and bowel (intestine or ‘gut’) to communicate are blocked. This can contribute to a number of bowel changes known as neurogenic bowel dysfunction. They include:
- Reduced sensation
- Slowed movement of stool through the bowel
- Loss of bowel control
Depending on whether your injury is above or below T12, you may experience spastic bowel or flaccid bowel, respectively. Spastic bowel is characterized by increased muscle tone in the intestines and sphincters while flaccid bowel is characterized by decreased tone. This difference can play a role in how your body responds to changes in diet including increased fibre intake.
Dietary fibre is an important part of a bowel management program for neurogenic bowel. After a SCI, food moves through the bowels at a much slower pace. Slow movement means that food takes much longer to digest, which can lead to dry, hard stools and constipation. Too little fibre in the diet can worsen constipation, resulting in pain and difficulty when emptying the bowels. Fibre can increase bulk and soften stool. This stimulates bowel movements and makes stool easier to pass. Foods with high fibre content tend to be lower in calories too. As a result, diets that are low in fibre can contribute to uncontrolled weight gain and lead to less stable blood sugar levels after meals.
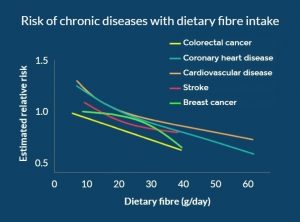
Figure 1. In the general population, with increasing dietary fibre, the risk for various lifestyle diseases decreases in a dose-response manner.8
Research in the general population shows that adequate dietary fibre intake is associated with a decreased risk of developing numerous chronic diseases, including heart disease, high blood pressure, obesity, stroke, type 2 diabetes, and intestinal diseases (e.g. constipation, hemorrhoids).
As people with SCI are more prone to developing these health conditions due to factors including sedentary lifestyle and changes in metabolism, getting enough fibre in the diet may provide long-term health benefits.
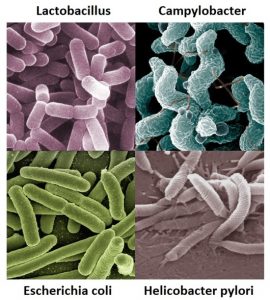
There is emerging evidence suggesting that an imbalance of bacteria in the gut is linked to the progression of chronic conditions including diabetes, obesity, pain, and neurogenic bowel dysfunction. Additionally, recent studies have demonstrated that imbalances to the bacterial composition in the gut may result following SCI. Since fibre supports the growth of healthy bacteria in the gut, a fibre-rich diet may help to decrease these health risks in people with SCI.
Refer to our article on the Microbiome in SCI for more information!
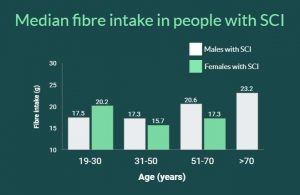
A detailed look at fibre in the diet of individuals with SCI shows similarity between countries:
- Canada (see the graph to the right): little variation between males and females or with age with values ranging from 15-23 g/day
- Switzerland: people with acute SCI average 14.4 g/day and those with chronic SCI get 15.6 g/day
- United States: 17.1 g/day
- Iran:17.9 g/day
| Individuals with SCI should not uniformly follow high fibre diets. For individuals with SCI, fibre should be increased slowly to avoid side effects and to assess tolerance. If symptoms of intolerance arise such as bloating or cramping, then one should try reducing or changing the type of fiber. |
 It is important to recognize that after a spinal cord injury, fibre can affect people differently and there is no agreed upon ideal amount of fibre for individuals with SCI. However, based on expert opinion, an initial diet containing no less than 15 g/day of fiber is recommended. One study (weak evidence) found that increasing dietary fibre from 25 g/day to 31 g/day with the addition of 40 g of “Kellogg’s All Bran” cereal a day to the diet worsened bowel function in 11 individuals with SCI. In fact, the higher fibre intake increased the time needed for food to move through the colon from 28 hours to 42 hours! While the Canadian recommendation for the general population is 25-38 grams per day, this study shows that individuals with SCI may respond differently to fibre. Further research is required on the effects of different types of fibre, as well as fluid intake on bowel function after an SCI.
It is important to recognize that after a spinal cord injury, fibre can affect people differently and there is no agreed upon ideal amount of fibre for individuals with SCI. However, based on expert opinion, an initial diet containing no less than 15 g/day of fiber is recommended. One study (weak evidence) found that increasing dietary fibre from 25 g/day to 31 g/day with the addition of 40 g of “Kellogg’s All Bran” cereal a day to the diet worsened bowel function in 11 individuals with SCI. In fact, the higher fibre intake increased the time needed for food to move through the colon from 28 hours to 42 hours! While the Canadian recommendation for the general population is 25-38 grams per day, this study shows that individuals with SCI may respond differently to fibre. Further research is required on the effects of different types of fibre, as well as fluid intake on bowel function after an SCI.
Increase fibre and increase water
 Drinking enough water during the day is important for your health and may help prevent complications such as urinary tract infections. There is a temptation to keep water intake low to reduce catheterization frequency or other disruptions to your bladder/bowel routine. But, when you increase fibre intake it is important to also increase fluid intake to compensate. Fibre sources such as fruits and vegetables naturally contain lots of water with all the fibre they provide. However, fibre supplements, cereals, or dried fruit, nuts, ground flax seed, and the like should be accompanied by increased water consumption. It is important to strike a balance between increased fluid intake, increased fibre, and the potential impacts on your bowel and bladder routine.
Drinking enough water during the day is important for your health and may help prevent complications such as urinary tract infections. There is a temptation to keep water intake low to reduce catheterization frequency or other disruptions to your bladder/bowel routine. But, when you increase fibre intake it is important to also increase fluid intake to compensate. Fibre sources such as fruits and vegetables naturally contain lots of water with all the fibre they provide. However, fibre supplements, cereals, or dried fruit, nuts, ground flax seed, and the like should be accompanied by increased water consumption. It is important to strike a balance between increased fluid intake, increased fibre, and the potential impacts on your bowel and bladder routine.
Interestingly, little to no attention is given in guidelines to how the source of fibre may affect the bowel. In one study in the general population, it was shown that doubling stool output could be accomplished with 10 g of grain or vegetable fibre while such a doubling required 25 g of fruit fibre. The interaction of different types of dietary fibre in SCI requires investigation.
The effect of increased fibre in individuals with SCI may differ depending on whether one has spastic or flaccid bowel. One study (weak evidence) interviewing individuals about their bowel routines noted that more individuals with flaccid bowel reported benefits by modifying their diet with high fibre foods than those with spastic bowel.
Given the benefits of dietary fibre in reducing a number of diseases, it makes sense to want to increase how much you get in your diet. Individuals with SCI should increase fibre in their diet slowly to avoid side effects. In addition, for some people, high amounts of fibre may not be tolerated and fibre should be reduced if it worsens their bowel function.
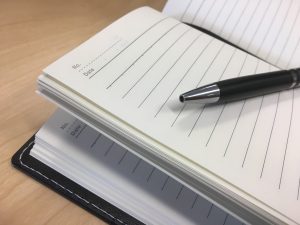
Assess how much dietary fibre you currently eat
- Take a week-long diet history by writing down what and how much you eat and drink every day for a week. You can then calculate your fibre based on the foods you have eaten using an online fibre calculator.
- At the same time, also record the effects of your current fibre intake on stool consistency (see the Bristol Stool Scale), frequency and duration of bowel movements.
- With this information, you will know how much fibre you are currently getting and how it affects your bowel routine. Then, you may decide to stay where you are or to increase your fibre intake.
Increase dietary fibre slowly and continue to monitor your diet
- If you decide to increase your fibre intake, proceed gradually and obtain fibre from a wide variety of sources as described in the beginning of this article.
- Make one or two changes a week such as adding a daily serving of fruit or switching to whole grain pasta and continue to keep track of stool consistency, frequency of bowel movements, as well as any symptoms of intolerance. Keep track of how your body responds to more fibre, different sources of fibre-containing foods and more fluids to help you make informed decisions.
- Recognize that some foods may not agree with you. These may be spicy foods that disrupt the digestive system or certain foods that cause more gas. Beans and cruciferous vegetables (like broccoli and Brussel sprouts) have a reputation for increasing flatulence, but this is usually temporary and your body adapts. Start off with small amounts of these foods and increase gradually. Recognize that you can develop a tolerance to certain foods.
- Should symptoms of intolerance occur (e.g., bloating, cramping, and gas), reduce your dietary fibre intake or try a different source of fibre.
- Balance the amount of water needed for optimal stool consistency with that needed for bladder management. Based on expert opinion, people with SCI should aim for a daily fluid intake of 500 mL more than the general population. This can be calculated by using the formula: 40 mL x body weight in kg + 500 mL.
Read our article on Bowel Changes After SCI for more information!
Incorporating higher dietary fibre intake into your life
- It is likely that increased dietary fibre and increased water in your diet will affect your bowel and bladder routine. Bowel movements may be required on a daily basis as opposed to every other day or less and more catheterizations may be required for the bladder.
- These consequences of increased dietary fibre intake need to be weighed by you and your caregivers. If the changes are not acceptable, a new balance must be reached that works for your lifestyle.
The main way to increase fibre is to make vegetables, fruit, whole grains, and plant-based protein foods the cornerstone of your diet, as per Canada’s Food Guide.
Eating a whole food plant-based diet to meet your fibre needs instead of supplements is preferred as whole foods provide nutritional benefits that fibre supplements do not. Indeed, studies which reduced the risk of disease with fibre used food and not supplements. It is not clear if fibre from supplements brings similar benefits. However, there may be situations where a fibre supplement is the best solution.
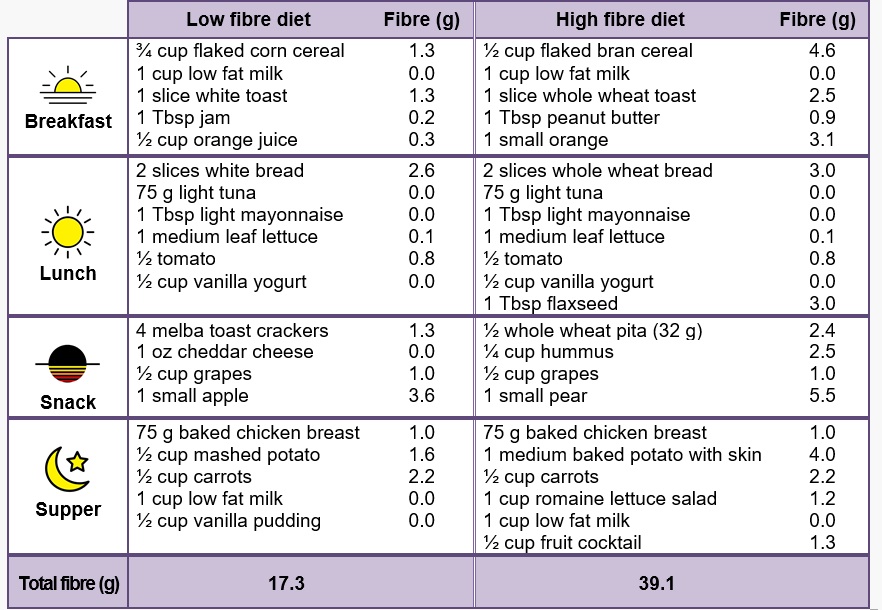
Below is an example from Dietitians of Canada of how a low fibre diet can be modified into a high fibre diet.
Other simple ways to increase fibre in your diet include:
- Choose whole fruit over fruit juices
- Try a fruit or vegetable you’ve never heard of
- Avoid peeling vegetables and fruits where appropriate
- Add legumes such as lentils, beans, and peas to soups, salads, and other dishes
- Add seaweed to soup
- Switch white for 100% % whole grain bread, pasta and rice
- Eat nuts and seeds as snacks or toppings to salads
- Use whole grain flour when baking
- Add ground flax seed to your morning oatmeal or smoothie
- Read food nutrition labels and choose foods containing more fibre
 Calculating the percent daily value for fibre
Calculating the percent daily value for fibre
The percent daily value (% DV) is a guideline to help you make informed food choices.
According to Canada’s Food Guide, food with 5% DV or less per serving size is considered little of a nutrient. On the other hand, food with 15% DV or more per serving size is considered a lot of a nutrient. To help reach the recommended amount of fibre in your diet, aim for food containing 15% DV or greater.
In Canada, the DV of fibre is 25 g/day. The box of crackers in the picture indicates that each serving size provides 2 g of fibre. The % DV would be calculated to be (2 g ÷ 25 g) x 100 = 8% DV.
Dietary fibre is an important part of a healthy bowel routine. Based on expert opinion, an initial diet containing at least 15 g/day of fiber is recommended in people with SCI. Increases in fibre should be individualized and done gradually. General population fibre guidelines may not be appropriate for people after SCI, and in some cases may worsen their bowel function.
Research in the general population shows that increasing fibre in the diet reduces the risk of many lifestyle diseases that individuals with SCI are at a higher risk of developing. If you are interested in increasing your dietary fibre, adding fibre requires an individualized approach.
The recommended individualized approach is to track your diet for a week before and then during the process of increasing fibre. With the information in the food journal, you can see out how much fibre and fluids you are getting on an average day and how increased fibre and fluids affect your bowel and bladder routine. Increases in dietary fibre should be progressed slowly and monitored closely by the individual and their health care provider.
For a review of how we assess evidence at SCIRE Community and advice on making decisions, please see SCIRE Community Evidence.
Coggrave M, Mills P, Williams R, Eng JJ, (2014). Bowel Dysfunction and Management Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors. Spinal Cord Injury Rehabilitation Evidence. Version 5.0. Vancouver: p 1-48.
Available from: https://scireproject.com/evidence/bowel-dysfunction-and-management/
Evidence for “Why is fibre important in spinal cord injury?” is based on:
Lockyer, S., Spiro, A., & Stanner, S. (2016). Dietary fibre and the prevention of chronic disease – should health professionals be doing more to raise awareness? Nutrition Bulletin, 41(3), 214–231. https://doi.org/10.1111/nbu.12212
Slavin, J. L. (2008). Position of the American Dietetic Association: health implications of dietary fiber. Journal of the American Dietetic Association, 108(10), 1716–1731. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/18953766
Gungor, B., Adiguzel, E., Gursel, I., Yilmaz, B., & Gursel, M. (2016). Intestinal Microbiota in Patients with Spinal Cord Injury. PLOS ONE, 11(1), e0145878. https://doi.org/10.1371/journal.pone.0145878
Zhang, C., Zhang, W., Zhang, J., Jing, Y., Yang, M., Du, L., … Li, J. (2018). Gut microbiota dysbiosis in male patients with chronic traumatic complete spinal cord injury. Journal of Translational Medicine, 16(1), 353. https://doi.org/10.1186/s12967-018-1735-9
Data for Figure 1 “Risk of chronic diseases with dietary fibre intake” is based on:
Aune, D., Chan, D. S. M., Lau, R., Vieira, R., Greenwood, D. C., Kampman, E., & Norat, T. (2011). Dietary fibre, whole grains, and risk of colorectal cancer: Systematic review and dose-response meta-analysis of prospective studies. BMJ (Online). http://doi.org/10.1136/bmj.d6617
Threapleton, D. E., Greenwood, D. C., Evans, C. E. L., Cleghorn, C. L., Nykjaer, C., Woodhead, C., … Burley, V. J. (2013). Dietary fibre intake and risk of cardiovascular disease: systematic review and meta-analysis. BMJ (Clinical Research Ed.), 347, f6879. http://doi.org/10.1136/bmj.f6879
Threapleton, D. E., Greenwood, D. C., Evans, C. E. L., Cleghorn, C. L., Nykjaer, C., Woodhead, C., … Burley, V. J. (2013). Dietary Fiber Intake and Risk of First Stroke. Stroke, 44(5), 1360–1368. http://doi.org/10.1161/STROKEAHA.111.000151
Aune, D., Chan, D. S. M., Greenwood, D. C., Vieira, A. R., Navarro Rosenblatt, D. A., Vieira, R., & Norat, T. (2012). Dietary fiber and breast cancer risk: A systematic review and meta-analysis of prospective studies. Annals of Oncology. http://doi.org/10.1093/annonc/mdr589
Evidence for “How much fibre do we get?” is based on:
Walters, J. L., Buchholz, A. C., Martin Ginis, K. A., & SHAPE-SCI Research Group. (2009). Evidence of dietary inadequacy in adults with chronic spinal cord injury. Spinal Cord, 47(4), 318–322. https://doi.org/10.1038/sc.2008.134
Perret, C., & Stoffel-Kurt, N. (2011). Comparison of nutritional intake between individuals with acute and chronic spinal cord injury. The Journal of Spinal Cord Medicine, 34(6), 569–575. https://doi.org/10.1179/2045772311Y.0000000026
Tomey, K. M., Chen, D. M., Wang, X., & Braunschweig, C. L. (2005). Dietary intake and nutritional status of urban community-dwelling men with paraplegia. Archives of Physical Medicine and Rehabilitation, 86(4), 664–671. https://doi.org/10.1016/j.apmr.2004.10.023
Sabour, H., Javidan, A. N., Vafa, M. R., Shidfar, F., Nazari, M., Saberi, H., … Emami Razavi, H. (2012). Calorie and macronutrients intake in people with spinal cord injuries: An analysis by sex and injury-related variables. Nutrition, 28(2), 143–147. https://doi.org/10.1016/j.nut.2011.04.007
Data for Figure 2 “Median fibre intake in people with SCI” is based on:
Walters, J. L., Buchholz, A. C., Martin Ginis, K. A., & SHAPE-SCI Research Group. (2009). Evidence of dietary inadequacy in adults with chronic spinal cord injury. Spinal Cord, 47(4), 318–322. https://doi.org/10.1038/sc.2008.134
Evidence for “How much fibre should you get?” is based on:
Health Canada. (2019). Fibre. Retrieved January 2, 2019, from https://www.canada.ca/en/health-canada/services/nutrients/fibre.html
Consortium for Spinal Cord Medicine. (1998). Clinical practice guidelines: Neurogenic bowel management in adults with spinal cord injury. Retrieved from http://www.pva.org/media/pdf/cpg_neurogenic bowel.pdf
Cameron, K. J., Nyulasi, I. B., Collier, G. R., & Brown, D. J. (1996). Assessment of the effect of increased dietary fibre intake on bowel function in patients with spinal cord injury. Spinal Cord, 34(5), 277–283. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8963975
de Vries, J., Birkett, A., Hulshof, T., Verbeke, K., & Gibes, K. (2016). Effects of Cereal, Fruit and Vegetable Fibers on Human Fecal Weight and Transit Time: A Comprehensive Review of Intervention Trials. Nutrients, 8(3), 130. https://doi.org/10.3390/nu8030130
Yim, S. Y., Yoon, S. H. S., Lee, I. Y., Rah, E. W., & Moon, H. W. (2001). A comparison of bowel care patterns in patients with spinal cord injury: Upper motor neuron bowel vs lower motor neuron bowel. Spinal Cord, 39(4), 204–207. https://doi.org/10.1038/sj.sc.3101131
Evidence for “How do you choose the right foods?” is based on:
Threapleton, D. E., Greenwood, D. C., Evans, C. E. L., Cleghorn, C. L., Nykjaer, C., Woodhead, C., … Burley, V. J. (2013). Dietary fibre intake and risk of cardiovascular disease: systematic review and meta-analysis. BMJ (Clinical Research Ed.), 347, f6879. https://doi.org/10.1136/bmj.f6879
Hartley, L., May, M. D., Loveman, E., Colquitt, J. L., & Rees, K. (2016). Dietary fibre for the primary prevention of cardiovascular disease. Cochrane Database of Systematic Reviews, (1), CD011472. https://doi.org/10.1002/14651858.CD011472.pub2
Dietitians of Canada. (2014). Healthy Eating Guidelines for Increasing your Fibre Intake. Retrieved from www.dietitians.ca
Health Canada. (2019). Percent daily value. Retrieved January 31, 2019, from https://www.canada.ca/en/health-canada/services/understanding-food-labels/percent-daily-value.html
Image credits
- Top view walnuts texture horizontal ©8photo, CC BY 2.0
- Almond almonds brazil nut ©David Stewart, CC BY 2.0
- Mr Beans ©Kenneth Leung, CC BY 2.0
- Vegan Nine Grain Whole Wheat Bread ©Veganbaking.net, CC BY-SA 2.0
- Banana © kimwang yip, CC0 1.0
- IMG_8230 1 ©Dennis Amith, CC BY-NC 2.0
- Modified from: Stomach Colon Rectum Diagram ©William Crochot, CC BY-SA 4.0
- Image ©SCIRE
- Modified from: Lactobacillus casei ©AJC1, CC BY-SA 2.0
- Modified from: Campylobacter bacteria ©Microbe World, CC BY-NC-SA 2.0
- Modified from: Koli Bacteria ©geralt geralt / 18959 images, CC0 1.0
- Modified from: jpg ©Lamiot, CC0 1.0
- Image ©SCIRE
- Kellogg’s Cereals #2 ©Like_the_Grand_Canyon, CC BY-NC 2.0
- Water ©rawpixel, CC0 1.0
- Image ©SCIRE
- Canada’s Food Guide ©Health Canada. All Rights Reserved. Adapted and reproduced with permission from the Minister of Health, 2019.
- sun ©Maxim Kulikov, CC BY 3.0 US
- sun ©johartcamp, CC BY 3.0 US
- sunset ©ruliani, CC BY 3.0 US
- Moon ©Three Six Five, CC BY 3.0 US
- Kombu ©Alice Wiegand, CC BY-SA 3.0
- Modified from: Ground flax seed ©Veganbaking.net, CC BY-SA 2.0
- Image ©SCIRE
- Daily Value meter ©Health Canada. All Rights Reserved. Adapted and reproduced with permission from the Minister of Health, 2019.