Author: SCIRE Community Team | Reviewer: Darryl Caves | Published: 9 April 2018 | Updated: ~
Changes to blood pressure control after spinal cord injury (SCI) may contribute to a condition called orthostatic hypotension. This page provides information about orthostatic hypotension after SCI.
Key Points
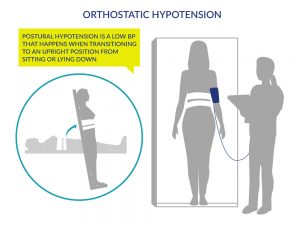
- Orthostatic hypotension is a decrease in blood pressure when moving from a lying or sitting position to an upright position.
- Orthostatic hypotension may be experienced as dizziness, light-headedness, fainting and weakness when getting upright.
- Research suggests that the medication midodrine hydrochloride is effective for treating orthostatic hypotension after SCI.
- A number of other medications and non-drug treatments are also used to treat orthostatic hypotension, including fluid and salt intake, compression garments, electrical stimulation and various forms of physical activity. Further research is needed to determine if these treatments are effective.
Orthostatic hypotension (also called postural hypotension) is a decrease in blood pressure when moving from a sitting or lying position to an upright position.
Orthostatic hypotension is common early after an SCI, but it can also be present long-term or following an illness or period of reduced mobility. Orthostatic hypotension may happen with or without symptoms.
Signs and symptoms of orthostatic hypotension:
- Dizziness
- Light-headedness
- Fainting
- Temporary loss of consciousness (experiencing a ‘black out’)
- Fatigue (tiredness)
- Blurry vision
- Muscle weakness
Orthostatic hypotension is more common early after injury. For some people, orthostatic hypotension gradually goes away as their body adapts to the changes after the injury. However, for others, orthostatic hypotension persists over time and may require treatment to manage their symptoms.
Orthostatic hypotension can happen to anyone after SCI; however certain factors are associated with developing orthostatic hypotension.
People with higher level injuries
Orthostatic hypotension is more common in people with higher levels of SCI, especially with injuries in the cervical and mid to upper thoracic spinal cord (injuries above T6).
People with traumatic injuries
People with traumatic SCI are more likely to develop orthostatic hypotension than those with a non-traumatic SCI.
When the body moves into an upright position, the blood naturally flows downward because of gravity. If the body does not respond in any way to help push the blood back up, it pools in the blood vessels of the lower body, causing a drop in blood pressure in the upper body. If blood pressure is low, not enough blood can reach the heart and brain, which causes symptoms like dizziness, fainting and tiredness.
How is blood pressure controlled when the spinal cord is not injured?
Under normal circumstances, when we move upright, the body’s blood pressure control mechanisms kick in to maintain circulation. The main changes include:
- The blood vessels narrow (called vasoconstriction), to prevent pooling and maintain blood pressure.
- The heart works harder by pumping more quickly to help push blood through circulation.
The combined narrowing of blood vessels and increase in heart rate help maintain blood pressure against the force of gravity in standing. These changes are controlled by the autonomic nervous system.
Orthostatic hypotension is common after SCI, particularly in the early period after injury. There are several reasons that orthostatic hypotension happens after SCI.
Bed rest
During the early phase after injury, bed rest is often required for healing of injuries. However, long periods of bed rest and reduced movement can cause the heart and blood vessels to become less responsive to position changes and changes in blood pressure.
During bed rest, there is a shift in the distribution of fluids within the body which causes a loss of fluid through urination (called diuresis). This leads to reduced blood volume (the volume of blood in circulation), which affects the body’s ability to adapt to changes in blood pressure. This likely contributes to orthostatic hypotension in the early phase after SCI.
The body may also produce more of a chemical called nitric oxide as a result of bed rest following SCI, which causes widening (relaxing) of the blood vessels and further contribute to orthostatic hypotension.
Changes to the autonomic nervous system
The main reason that orthostatic hypotension happens after SCI is because of altered control of the autonomic nervous system.
The autonomic nervous system
The autonomic nervous system controls largely unconscious bodily processes such as blood pressure, heart rate, breathing rate, body temperature, digestion, bladder, bowel and sexual function. It has two divisions:
- The sympathetic nervous system prepares the body for stressful or emergency situations. It is often called the ‘fight or flight’ system, because it prepares the body for action. For example, it increases heart rate and constricts blood vessels.
- The parasympathetic nervous system prepares the body for normal, non-emergency situations. It is often called the ‘rest and digest’ system, because it allows the body to restore itself. For example, it slows heart rate and relaxes blood vessels.
The sympathetic and parasympathetic systems have different (and often opposite) effects on the organs and work together to control bodily functions according to the situation.
Most of the nerves that control the sympathetic nervous system arise from the thoracic spinal cord. Because the sympathetic nerves are responsible for narrowing (constricting) the blood vessels and increasing heart rate when changing positions, SCI in these areas can affect blood pressure control. Without the sympathetic nervous system, the blood vessels and heart rate do not respond appropriately to changes in position and blood can pool in the legs and abdomen, leading to orthostatic hypotension.
Reduced muscle activity
Loss of muscle activity in the legs and trunk after SCI may also contribute to orthostatic hypotension. Normally, when the muscles tense, they act like small pumps that squeeze the blood vessels to help push blood back up to the heart. Muscle activity in the legs and abdomen helps to maintain blood pressure in standing. This is sometimes called the skeletal muscle pump.
If there is paralysis in the leg muscles, the muscles do not help to pump blood back up to the heart, which can lead to blood pooling and orthostatic hypotension. This is why sometimes just sitting for a long time after a position change to upright can lead to symptoms of orthostatic hypotension. The effects of the loss of muscle activity seem to have a greater impact earlier after injury, before the body develops strategies to compensate for blood pressure changes.
Cardiovascular deconditioning
 During the early phase after injury, bed rest is often required for healing of injuries. However, long periods of bed rest and reduced movement can cause the heart and blood vessels to become less responsive to position changes and changes in blood pressure. This likely contributes to orthostatic hypotension in the early phase after SCI.
During the early phase after injury, bed rest is often required for healing of injuries. However, long periods of bed rest and reduced movement can cause the heart and blood vessels to become less responsive to position changes and changes in blood pressure. This likely contributes to orthostatic hypotension in the early phase after SCI.
The body may also produce more of a chemical called nitric oxide as a result of bed rest following SCI, which causes widening (relaxing) of the blood vessels and further contributes to orthostatic hypotension.
Low blood volume and salt levels in the blood
The body regulates blood volume (the amount of blood in circulation) through water and salt levels in the blood. Spinal cord injury can disrupt this balance and lead to low blood volume, low blood pressure and orthostatic hypotension. Low salt levels in the blood are also common after SCI, which can also contribute to orthostatic hypotension. A diet that is low in salt or fluids can also contribute to orthostatic hypotension.
Other factors that may contribute to orthostatic hypotension after SCI
Heat exposure
Warm environments can increase the likelihood of experiencing orthostatic hypotension. The body responds to heat by widening the blood vessels, which lowers blood pressure. Excessive sweating in warm environments may also lead to dehydration, which further contributes to orthostatic hypotension.
 Medications
Medications
Many medications can trigger orthostatic hypotension. These include medications used to treat conditions such as high blood pressure, heart disease and erectile dysfunction.
Alcohol and caffeine
Consuming alcohol and caffeine can worsen orthostatic hypotension by affecting the constriction of blood vessels during position changes and contributing to dehydration.
After eating meals
After eating, more blood is sent to the intestines for digestion, which may lower blood pressure. Postprandial hypotension is a form of orthostatic hypotension experienced after eating large meals. It is more common among older people.
Exercise (in people with high levels of SCI)
People with complete cervical SCI may experience orthostatic hypotension during and after exercise, even if they are well-hydrated and have taken steps to avoid overheating. This happens because the heart and blood vessels do not respond adequately to compensate for the increased blood flow to the muscles. This can cause symptoms like dizziness or nausea while exercising. To adjust for this, individuals may start their exercise programs with a slow progression or may need to use other strategies to enable them to exercise safely.
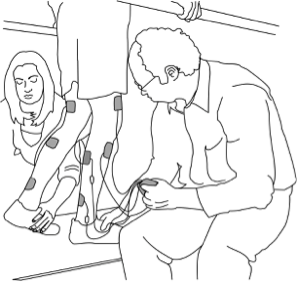
To diagnose orthostatic hypotension, blood pressure is first measured while in a lying or sitting position and then again in an upright or standing position. The two blood pressure readings are compared to see if there is a drop in blood pressure. Other times, severe symptoms alone (such as fainting) may be used to diagnose orthostatic hypotension.
Since many people with SCI cannot stand, blood pressure can be assessed based on a lying then sitting position instead. A tilt table or other supportive device can be used to assist with getting upright.
How to interpret blood pressure readings
The heart contracts and relaxes as it pumps blood throughout the body. A blood pressure reading usually shows up with two numbers:
- The systolic blood pressure is the blood pressure when the heart contracts. It is usually the first of the two numbers (i.e. ‘120’ when someone says ‘120 over 80’).
- The diastolic blood pressure is the blood pressure when the heart relaxes. It is usually the second of the two numbers (i.e. ‘80’ when someone says ‘120 over 80’).
Orthostatic hypotension is diagnosed when there is a decrease of at least 20 mmHg in systolic blood pressure or a decrease of at least 10 mmHg in diastolic blood pressure after moving from lying or sitting to standing.
Currently, midodrine hydrochloride (midodrine) is the only medication recommended for managing orthostatic hypotension after SCI. There is not enough evidence to support the use of other medications. However, medications intended to help treat orthostatic hypotension may also have other unwanted effects on blood pressure after SCI, so should be discussed in detail with your health team for more information.
Midodrine hydrochloride (midrodrine, ProAmatine) is a medication that causes the blood vessels to tighten (constrict). When this occurs, more blood flow travels to the heart and blood pressure increases to prevent blood pressure from dropping in standing. Midodrine is taken by mouth in the form of tablets. Regular blood pressure monitoring done by you or your caregiver will be required to ensure the medication is working properly.
There is moderate evidence that midodrine is effective for treating orthostatic hypotension after SCI and may improve exercise performance by decreasing symptoms of low blood pressure.
There are a number of other medications that have been suggested for reducing orthostatic hypotension, but are ineffective or the evidence is inconclusive. These include:
- Fludrocortisone
- Dihydroergotamine or ergotamine
- Ephedrine
- Droxidopa or L-DOPS
- Nitro-L-arginine methyl ester or L-NAME
Several other treatment options may be used to treat orthostatic hypotension. Although there is limited evidence to determine whether these treatments are effective, they may be used in addition to drug treatments to help manage orthostatic hypotension after SCI.
Fluids and salt
Adequate fluid and salt intake may help to increase blood volume and maintain blood pressure. There is weak evidence that fluid and salt intake combined with medications may be effective for treating orthostatic hypotension after SCI. However, no research studies have been done using fluid and salt alone.
Compression garments
Blood pooling happens when gravity causes blood to collect in the abdomen and legs. This limits blood flow to other areas of the body and contributes to orthostatic hypotension. Compression garments are devices that apply pressure to these areas of the body to help blood circulate back up toward the heart. Compression garments used after SCI include:
- Abdominal binders are devices that are placed around the lower torso to apply pressure to the abdomen. Most abdominal binders are elastic wraps with Velcro closures that are fitted around the waist.
- Compression stockings are long socks that apply pressure to the calves.
Compression garments are commonly used for orthostatic hypotension after SCI because they are inexpensive and unlikely to cause side effects. However, there is conflicting evidence about whether they are effective to reduce orthostatic hypotension after SCI.
Click here to read more about Abdominal Binders.
Gradual progression toward moving upright
After a prolonged period of bed rest (such as very early after an SCI) it may take time for the body to adjust to getting upright. Health providers will usually gradually progress a person towards getting upright to help adjust the body to the new position slowly.
This may be done by dangling the legs on the edge of the bed for a period of time before slowly raising the head and getting into a wheelchair. It may also be done by gradually increasing the degree of incline of a tilt table while being mindful of symptoms.
Gradual progression towards moving upright is commonly used in the management of orthostatic hypotension, however, it has not been investigated in research studies.
Exercise
Regular exercise improves blood flow and may enhance the body’s ability to adapt to changes in posture. However, after an SCI, there are many different ways that the body responds to exercise, depending on the characteristics of the injury itself. People who have complete injuries in the cervical spinal cord can actually sometimes cause a drop in blood pressure (see above).
There is moderate evidence that arm exercise is not beneficial for reducing orthostatic hypotension in people with SCI.
- There is weak evidence that body weight-supported treadmill training does not significantly improve orthostatic hypotension in people with SCI.
- There is weak evidence suggesting that two hours of daily exercise twice a week for a period of at least two years may help reduce orthostatic hypotension in individuals with SCI.
Standing
Standing treatments, especially those that involve some type of stimulation to the leg muscles, are thought to stimulate the nervous system and potentially improve blood pressure responses to standing. There is weak evidence that standing with a harness and assistance from health providers may help to increase resting blood pressure and improve orthostatic hypotension in people with cervical SCI.
See our article on Supported Standing for more information!
Functional electrical stimulation (FES)
Functional electrical stimulation (FES) is a treatment where electrical stimulation is applied to the nerves and muscles to cause muscle contractions during an activity. Functional electrical stimulation stimulates the nerves and produces muscular contractions, which may help pump blood back to the heart. There is moderate evidence that functional electrical stimulation can help stabilize blood pressure during changes in position and may be used to supplement other forms of orthostatic hypotension treatment after SCI.
See our article on FES for more information!
Vibration
Whole-body vibration is a primarily experimental treatment that involves exercising on a vibrating platform. This treatment is thought to cause muscle contractions which may help improve blood flow. There is strong evidence that whole-body vibration can increase blood pressure in people with SCI, but the direct effects of vibration on orthostatic hypotension after SCI has not been studied. Currently, whole-body vibration is not usually available outside of research settings.
Orthostatic hypotension is a common condition after SCI, in which blood pressure drops when moving from a lying or sitting position to an upright position. For some, orthostatic hypotension gradually goes away over time. For others, it may persist long-term and require medical treatment.
While research evidence supports the use of the medication midodrine for treating orthostatic hypotension following SCI, there is little evidence to support the use of other medications for this purpose.
Many non-drug treatments also exist that are commonly used. However, for the most part, there is a lack of research on whether these treatments are effective. Functional electrical stimulation may be effective in reducing orthostatic hypotension after SCI.
It is important to discuss these treatment options with your health providers to determine which ones are suitable options for you.
For a review of how we assess evidence at SCIRE Community and advice on making decisions, please see SCIRE Community Evidence.
Parts of this page have been adapted from the SCIRE Professional “Orthostatic Hypotension” Module:
Krassioukov A, Wecht JM, Teasell RW, Eng JJ (2014). Orthostatic Hypotension Following Spinal Cord Injury. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors. Spinal Cord Injury Rehabilitation Evidence. Version 5.0. Vancouver: p. 1-26.
Available from: scireproject.com/evidence/orthostatic-hypotension/
Evidence for “What medications are used to treat orthostatic hypotension?” is based on the following studies:
Midodrine:
[1] Nieshoff EC, Birk TJ, Birk CA, Hinderer SR, Yavuzer G. Double-blinded, placebo-controlled trial of midodrine for exercise performance enhancement in tetraplegia: a pilot study. J Spinal Cord Med 2004;27:219-225.
[2] Wecht JM, Rosado-Rivera D, Handrakis JP, Radulovic M, Bauman WA. Effects of midodrine hydrochloride on blood pressure and cerebral blood flow during orthostasis in persons with chronic tetraplegia. Arch Phys Med Rehabil 2010; 91: 1429-1435.
Other medications:
[1] Barber DB, Rogers SJ, Fredrickson MD, Able AC. Midodrine hydrochloride and the treatment of orthostatic hypotension in tetraplegia: two cases and a review of the literature. Spinal Cord 2000;38:109-111.
[2] Groomes TE, Huang CT. Orthostatic hypotension after spinal cord injury: treatment with fludrocortisone and ergotamine. Arch Phys Med Rehabil 1991;72:56-58.
[3] Frisbie JH, Steele DJ. Postural hypotension and abnormalities of salt and water metabolism in myelopathy patients. Spinal Cord 1997;35:303-307.
[4] Wecht JM, Rosado-Rivera D, Weir JP, Ivan A, Yen C, Bauman WA. Hemodynamic effects of L-Threo-3,4-dihydroxyphenylserine (droxidopa) in hypotensive individuals with spinal cord injury. Arch Phys Med Rehabil 2013; 94: 2006-2012.
[5] Muneta S, Iwata T, Hiwada K, Murakami E, Sato Y, Imamura Y. Effect of L-threo-3, 4-dihydroxyphenylserine on orthostatic hypotension in a patient with spinal cord injury. Jpn Circ J 1992;56:243-247.
[6] Wecht JM, Radulovic M, Rosado-Rivera D, Zhang RL, La Fountaine MF, Bauman WA. Orthostatic effects of midodrine versus L-NAME on cerebral blood flow and the renin-angiotensin-aldosterone system in tetraplegia. Arch Phys Med Rehabil 2011; 92: 1789-1795.
[7] Wecht JM, Weir JP, Goldstein DS, Krothe-Petroff A, Spungen AM, Holmes C, et al. Direct and reflexive effects of nitric oxide synthase inhibition on blood pressure. Am J Physiol Heart Circ Physiol 2008;294:H190-197.
[8] Wecht JM, Radulovic M, La Fountaine M, Rosado-Rivera D, Zhang RL, Bauman W. Orthostatic responses to nitric oxide synthase inhibition in persons with tetraplegia. Arch Phys Med Rehabil; 2009:1428-1434.
[9] Wecht JM, Weir JP, Krothe AH, Spungen AM, Bauman WA. Normalization of supine blood pressure after nitric oxide synthase inhibition in persons with tetraplegia. J Spinal Cord Med 2007; 30: 5-9.
Evidence for “What other treatment options are there?” is based on the following studies:
[1] Yarar-Fisher C, Pascoe DD, Gladden LB, Quindry JC, Hudson J, Sefton J. Acute physiological effects of whole body vibration (WBV) on central hemodynamics, muscle oxygenation and oxygen consumption in individuals with chronic spinal cord injury. Disabil Rehabil 2013; early online: 1-10.
[2] Faghri PD, Yount J. Electrically induced and voluntary activation of physiologic muscle pump: a comparison between spinal cord-injured and able-bodied individuals. Clin Rehabil 2002;16:878-885.
[3] Elokda AS, Nielsen DH, Shields RK. Effect of functional neuromuscular stimulation on postural related orthostatic stress in individuals with acute spinal cord injury. J Rehabil Res Dev 2000;37:535-542.
[4] Sampson EE, Burnham RS, Andrews BJ. Functional electrical stimulation effect on orthostatic hypotension after spinal cord injury. Arch Phys Med Rehabil 2000; 81: 139-143.
[5] Lopes P, Figoni SF, Perkash I. Upper limb exercise effect on tilt tolerance during orthostatic training of patients with spinal cord injury. Arch Phys Med Rehabil 1984;65:251-253.
[6] Ditor DS, Macdonald MJ, Kamath MV, Bugaresti J, Adams M, McCartney N, Hicks AL. The effects of body-weight supported treadmill training on cardiovascular regulation in individuals with motor-complete SCI. Spinal Cord 2005;43:664-673.
[7] Otsuka Y, Shima N, Moritani T, Okuda K, Yabe K. Orthostatic influence on heart rate and blood pressure variability in trained persons with tetraplegia. Eur J Appl Physiol 2008;104:75-78.
[8] Harkema SJ, Ferreira CK, van den Brand RJ, Krassioukov AV. Improvements in orthostatic instability with stand locomotor training in individuals with spinal cord injury. J Neurotrauma 2008;25:1467-1475.
Other references:
Claydon VE, Steeves JD, Krassioukov A. Orthostatic hypotension following spinal cord injury: understanding clinical pathophysiology. Spinal Cord 2006;44:341-351.
Hopman MT, Groothuis JT, Flendrie M, Gerrits KH, Houtman S. Increased vascular resistance in paralyzed legs after spinal cord injury is reversible by training. J Appl Physiol 2002;93:1966-1972.
McKinley WO, Jackson AB, Cardenas DD, DeVivo MJ. Long-term medical complications after traumatic spinal cord injury: a regional model systems analysis. Arch Phys Med Rehabil 1999;80:1402-1410.
Munakata M, Kameyama J, Kanazawa M, Nunokawa T, Moriai N, Yoshinaga K. Circadian blood pressure rhythm in patients with higher and lower spinal cord injury: simultaneous evaluation of autonomic nervous activity and physical activity. J Hypertens 1997;15:1745-1749.
Narkiewicz K, Cooley RL, Somers VK. Alcohol potentiates orthostatic hypotension: Implications for alcohol-related syncope. Circulation 2000; 101: 398-402.
Vaziri ND. Nitric oxide in microgravity-induced orthostatic intolerance: relevance to spinal cord injury. J Spinal Cord Med 2003;26:5-11.
Wecht JM, Bauman WA. Implication of altered autonomic control for orthostatic tolerance in SCI. Auton Neurosci. 2018 Jan;209:51-58.
Wecht JM, De Meersman RE, Weir JP, Spungen AM, Bauman WA. Cardiac autonomic responses to progressive head-up tilt in individuals with paraplegia. Clin Auton Res 2003; 13: 433-438.
Image credits:
- Blurry Downtown ©Dru Kelly, CC BY-ND 2.0
- Illustration by SCIRE Community Team
- Lung ©mungang kim, CC BY 3.0 US
- Heart ©Laymik, CC BY 3.0 US
- Digestive System ©Design Science, CC0 1.0
- Excretory system ©Olena Panasovska, CC BY 3.0 US
- Patient ©David, CC BY 3.0 US
- Assorted Medications ©NIAID, CC BY 2.0
- Blood pressure monitor robe materiel medical ©CHONION ANTOINE, CC BY-SA 4.0
- Multicare Pharmacist measuring Blood Pressure ©Woonjiawei, CC BY-SA 4.0
- Glass of water ©Maria Zamchy, CC BY 3.0 US
- Salt ©J Ray Rivera F, CC BY 3.0 US
- Stretch ©Claire Jones, CC BY 3.0 US
- Army Trials at Fort Bliss 160306-A-QR477-037 ©Adasia Ortiz, CC0 1.0
- Functional Electrical Stimulation Therapy for walking ©MilosRPopovic, CC BY-SA 4.0