Author: SCIRE Community Team | Reviewer: B. Catharine Craven | Published: 11 October 2017 | Updated: 14 March 2019
Osteoporosis is a condition that affects the bones of the hip and knee regions after spinal cord injury (SCI). This page provides information about osteoporosis after SCI and common treatments used for this condition.
Key Points
- SCI may cause declines in hip and knee region bone mineral density that leads to osteoporosis, and a greater risk of fracture over the person’s lifetime.
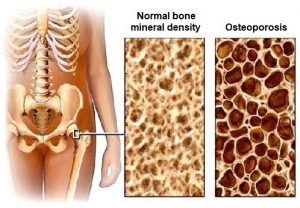
- Osteoporosis is a condition in which the bones become less dense, changing the bone structure and making the bones more likely to break (fracture) following simple activities.
- A bone density test is needed to detect osteoporosis and help you to estimate your fracture risk.
- People living with SCI, low bone density, and high fracture risk need treatment to reduce fractures.
- Common treatments for osteoporosis after SCI include bisphosphonate medications, supplements, and physical treatments (such as standing and functional electrical stimulation).
- The research evidence suggests that bisphosphonate medications are effective for preventing and treating bone loss after SCI and are usually started early after SCI. Physical treatments are not supported by current evidence for treating bone loss after SCI.
Osteoporosis is a condition in which the bones become less dense, changing the bone structure and making the bones more likely to break.
A bone mineral density test helps you and your doctor to measure the density of your bones and estimate how likely you are to get a fracture (broken bone) in the next ten years. Centres with expertise in SCI will ask you to have the density measured of your spine, hip and knee regions.
Healthy bone is constantly being broken down and reformed by the body’s cells in a process called bone remodeling. As a part of this process, the cells that breakdown bone tissue and the cells that create new bone, work to keep or increase the bone’s strength. Bones can adapt and change to the demands placed on them
After SCI, the cells that breakdown bone (osteoclasts) work over time, and the cells which build bone (osteoblasts) cannot keep pace, this results in thinning of the bone cortex and a lower number of bone cross struts and trabeculae. These changes in the bone decrease bone mineral density, usually areas rich in trabelcular bone are affected first and then the bone cortex.
Osteoporosis often affects people with SCI in a unique pattern called sublesional osteoporosis (‘sublesional’ means ‘below the level of injury’). Sublesional osteoporosis is a condition which involves:
Excessive bone resorption below the level of injury
- Low bone mineral density of the hip and or knee regions
- An increased risk of fracture
Bone tissues start to breakdown as early as the first few days after SCI. Among people with motor complete SCI, bone tissue resorption is highest between 3 and 6 months after injury and may continue for years. The rate of decline in bone density is less predictable in people with incomplete or non-traumatic SCI.
Osteoporosis is very common in people living with SCI long-term and increases the risk for fragility fractures.
Fragility fractures are fractures caused by minimal force such as twisting during a transfer or a low speed fall from your wheelchair. Fragility fractures typically happen at the lower part of the femur (thigh bone) just above the knee and the top of the tibia (shin bone) just below the knee. A red or swollen leg should prompt you to have an x-ray to rule out a fracture. Fractures can cause serious medical problems such as blood clots, skin infections, and pressure sores. Fractures above the knee are usually fixed by a surgeon, whereas fractures below the knee are usually casted. After SCI, fractures can be slow or hard to heal.Fragility fractures
Spinal cord injury can affect the body in a number of different ways that contribute to osteoporosis. These changes may include:
Changes to Body systems
Spinal cord injury affects many different systems in the body. Changes in the immune, hormone, circulatory, and nervous systems after SCI contribute to weaker bones after SCI. The role of these factors is not fully understood.
Fewer weight-bearing activities
Weight-bearing activities, like standing and walking, place forces through the bones of the legs and hips that stimulate the bones to become stronger. When a person spends less time standing and more time sitting, the bones experience fewer forces and adapt by becoming less dense and weaker.
Reduced muscle activity
Because muscles are connected to bones by tendons, the repeated pulling of muscles on bones during movement stimulates the bones to become stronger. When muscles become weak or paralyzed, the muscles atrophy and the muscles and bones nearby have fat deposited in them and there are not as many forces applied to the bones.
Lifestyle changes
Physical activity and nutritional habits can also influence the bones. After SCI, rates of physical activity, which can help to strengthen bone, are often lower than in people without SCI. In addition, changes in nutritional habits, such as reduced calcium and vitamin D intake can also contribute to low bone density after SCI.
Fragility fractures are very common after SCI. Individuals with these risk factors are more likely to experience a fracture after SCI. if you have more than 3 of the following fracture risk factors, please discuss them with your health care team.
Risk factors for fractures after SCI:
 Women
Women- Have a motor complete SCI (AIS A or AIS B, no movement of the legs)
- Paraplegia
- SCI for more than 10 years
- People less than 16 years of age at the time of the SCI onset
- People who consume more than 5 servings of alcohol per day
- Long term use of medications; specifically, anticonvulsants, heparin, or opioid medications
- Low weight for one’s height (a Body Mass Index (BMI) of less than 19)
- Low knee region bone mineral density
- Prior fragility fracture
- Family history of fracture
Measuring and monitoring bone mineral density after SCI is an important part of managing bone health. These measurements allow health providers to diagnose osteoporosis, estimate your fracture risk and monitor changes in your bone density over time. There are several methods that are commonly used to measure different aspects of bone health.
A bone density test or DXA (Dual-Energy X-ray Absorptiometry) Test is an imaging modality that uses non-invasive x-ray technology to scan and measure bone mineral density. DXA is the most widely used tool for measuring bone mineral density and diagnosing osteoporosis.
Peripheral Quantitative Computed Tomography is another non-invasive imaging method that can be used to diagnose osteoporosis of the shin region. This type of scan measures cortical thickness and trabecular volumetric bone mineral density. However, it is most often used in research.
Diagnosing osteoporosis
Health care providers will review your medical history, measure your blood chemistry and bone density, and ask you about your risk factors for fracture before diagnosing osteoporosis or estimating your future risk of fracture. After a fracture, you should undergo screening for osteoporosis.
1. Adequate, but not too much Vitamin D intake
Vitamin D is a vitamin that has an essential role in maintaining bone health by increasing the absorption of calcium. After SCI, there are a number of different factors that may contribute to a vitamin D deficiency, including reduced exposure to sunlight, inadequate diet, and side effects from medications metabolized by the liver. Research evidence suggests that vitamin D supplements can help to maintain bone mineral density in the legs after SCI. Your health care team should measure and monitor your vitamin D serum level to ensure it remains in the optimal range.
There are currently no SCI guidelines on vitamin D intake. In Canada, the general recommendation for adults is to consume 600 IU of vitamin D each day or 800 IU each day for those older than 70 years. Osteoporosis Canada recommends that people with osteoporosis, multiple fractures, or conditions affecting vitamin D absorption should aim for 800-2000 IU each day. Intakes greater than 4000 IU per day are not recommended to prevent adverse effects associated with excessive levels of calcium due to its increased absorption by vitamin D.
2. Adequate, but not too much Calcium intake
Calcium is the main mineral in bone and is a common supplement used to treat women with osteoporosis after menopause. Current evidence suggests that calcium supplements alone do not reduce bone loss after SCI. However, calcium and vitamin D are used together to maintain bone density. Additionally, research suggests that high calcium intake achieved by using supplements may be linked to the development of coronary artery calcification (hardening of the heart arteries due to calcium build-up). Increasing calcium intake through food sources instead appeared to decrease this risk. As a result, dietary sources of calcium should be optimized first before considering supplementation.
There are currently no SCI guidelines on calcium intake. In Canada, the general recommendation for adults is to consume 1000-1200 mg of calcium each day or 1200 mg each day for those older than 70 years. Intakes greater than 2000-2500 mg per day are not recommended to prevent adverse effects such as bone pain and kidney stones. If you have stones in your bladder or kidney, calcium intake will need to be lower than that of your peers.
3. Drug Therapy
There are two main treatment approaches that can be taken to osteoporosis after SCI, depending on the length of time since the injury:
Early approaches
Bone loss happens at a faster rate during the first year after SCI, so treatments during this time focus on preventing the loss of bone mineral density by slowing the rate of bone loss. Early treatment may involve oral bisphosphonate medications, which are often started within the first 3 months after injury.
Later approaches
If sublesional osteoporosis occurs of the hip and knee regions (usually after the first year), later treatment seeks to keep or increase hip or knee region bone mineral density. Treatments during this period may include bisphosphonate medications, Denosumab, or Recombinant Parathyroid Hormone (PTH), supplements, and physical treatments. These treatments are based on the assumption that regional increases in bone density will result in a lower fracture risk.
 Bisphosphonate medications are a family of drugs used to prevent the loss of bone mineral density. These drugs work by slowing the breakdown of bone or bone resorption. There are several drugs within this group, including Etidronate (Didrocal), Alendronate (Fosamax), Risedronate (Actonel), Clodronate (Bonefos, Clastion), and Tiludronate (Skelid). These drugs may be taken by mouth or through an intravenous (IV) line.
Bisphosphonate medications are a family of drugs used to prevent the loss of bone mineral density. These drugs work by slowing the breakdown of bone or bone resorption. There are several drugs within this group, including Etidronate (Didrocal), Alendronate (Fosamax), Risedronate (Actonel), Clodronate (Bonefos, Clastion), and Tiludronate (Skelid). These drugs may be taken by mouth or through an intravenous (IV) line.
Bisphosphonate medications are often prescribed early after SCI to prevent declines in bone density during the first year. Research evidence has mostly supported that bisphosphonate medications help to reduce bone mineral density loss in the hip and knee regions during the first year after SCI. These medications appear to be more effective when given earlier after SCI.
Bisphosphonates are also used to treat existing bone loss after SCI. One research study has shown that Alendronate is effective for maintaining or increasing bone mineral density later after SCI.
Despite support from research, there are still many things about the use of bisphosphonates after SCI that we do not know, such as their long-term effects and what the best length of treatment is. Bisphosphonate medications may also have side effects (such as heartburn, stomach upset, racing heart, jaw or thigh pain), drug interactions, and specific instructions for use that should be discussed in detail with your health providers before taking the medications.
For more detailed information about bisphosphonate medications, see SCIRE Professional’s module on Bone Heath.
There are a number of physical treatment options that have been proposed for preventing and treating bone loss after SCI, however, the evidence does not support their regular use in treating bone loss after SCI.
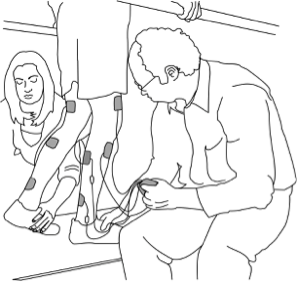
Functional electrical stimulation
Functional electrical stimulation (FES) is a treatment that applies electrical stimulation to the muscles during activities like standing, walking, or cycling. This treatment involves repeated pulling of the muscles on bones, which could help to strengthen the bones.
There is evidence suggesting that functional electrical stimulation cycling does not prevent bone loss in the lower leg early after SCI but may help to increase bone mineral density in stimulated areas of the leg during the later period after SCI. However, the stimulation needs to be ongoing or the benefits will be lost.
SCIRE Community provides additional detailed information about FES following SCI.
Electrical stimulation
Electrical stimulation to the muscles without functional activities may also be used. There is evidence suggesting that electrical stimulation can maintain or increase bone density over the stimulated areas. However, other studies have shown that the effects of electrical stimulation may return to baseline density within a few months after the treatment has ended.
Weight-bearing activities (standing and walking)
Weight-bearing activities are activities where the weight of the body is supported through the bones. Weight-bearing has long been considered to have an important role in bone health because it causes compression of the bones that may stimulate bone strengthening.
Weight-bearing treatments after SCI may include a variety of standing and walking activities, such as standing frames, braces, standing with functional electrical stimulation, and treadmill training.
Current evidence for weight-bearing activities for maintaining or improving bone health after SCI is inconclusive and needs further study.
Physical Activity
Physical activity is thought to improve bone health through a variety of processes that cause an increase in bone density. However, there is currently no evidence to support physical activity as a treatment for low bone density after SCI.
Therapies have been found to be ineffective:
Therapeutic ultrasound
Therapeutic ultrasound is a treatment that uses ultrasonic waves to provide energy to tissues deep within the body. Scientists have studied whether this treatment could provide stimulation to the bones to help prevent bone loss after SCI. However, current evidence suggests that therapeutic ultrasound is not effective for preventing bone loss after SCI.
Vibration exercise
Vibration exercise is a treatment that involves mechanical vibration of the body during resistance exercises. Current evidence suggests that vibration training is not effective for treating bone loss in the arms after SCI.
After SCI, low bone density implies an increased fracture risk. All of the current therapies are aimed at increasing bone mass and reducing your future risk of fracture.
Bisphosphonate medications are effective for preventing and treating bone loss after SCI and are usually started early after SCI onset. Non-drug physical treatments are not supported by current evidence for treating bone loss after SCI.
It is important to discuss any questions of concerns that you have about your treatment options in detail with your health providers to find the best management options for you. For a review of how we assess evidence at SCIRE Community and advice on making decisions, please see SCIRE Community Evidence.
Parts of this page have been adapted from the SCIRE Professional “Bone Health” Module:
Craven C, Lynch CL, Eng JJ (2014). Bone Health Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors. Spinal Cord Injury Rehabilitation Evidence. Version 5.0. Vancouver: p 1- 37.
Available from: https://scireproject.com/evidence/bone-health/
Astorino TA, Harness ET and Witzke KA. Effect of chronic activity-based therapy on bone mineral density and bone turnover in persons with spinal cord injury. Eur J Appl Physiol 2013; 113: 3027- 3037.
Bauman WA, Spungen AM. Disorders of carbohydrate and lipid metabolism in veterans with paraplegia or quadriplegia: A model of premature aging. Metabolism. 1994;43:749-56.
Bauman WA, Spungen AM. Coronary heart disease in individuals with spinal cord injury. Spinal Cord 2008;46:466-76.
Bauman WA, Morrison NG, Spungen AM. Vitamin D replacement therapy in persons with spinal cord injury. J Spinal Cord Med 2005;28:203-7.
Bauman WA, Spungen AM, Adkins RH, Kemp BJ. Metabolic and endocrine changes in persons aging with spinal cord injury. Assist Technol 1999c;11(2):88-96.
Bauman WA, Spungen AM, Zhong YG, Mobbs CV. Plasma leptin is directly related to body adiposity in subjects with spinal cord injury. Horm Metab Res 1997;28:732-6.
Bauman WA, Zhong YG, Schwartz E. Vitamin D deficiency in veterans with chronic spinal cord injury. Metabolism 1995;44:1612-6.
Bauman WA, Spungen AM, Raza M, Tothstein J, Zhang RL, Zhong YG, et al. Coronary artery disease: metabolic risk factors and latent disease in individuals with paraplegia. Mt Sinai J Med 1992;59:163-8.
Belanger M, Stein RB, Wheeler GD, Gordon T, Leduc B. Electrical stimulation: can it increase muscle strength and reverse osteopenia in spinal cord injured individuals? Arch Phys Med Rehabil 2000;8:1090-1098.
Cantorna MT, Vitamin D and its role in immunology: multiple sclerosis, and inflammatory bowel disease. Prog Biophys Mol Biol 2006;92:60-4.
Chain A, Koury JC, and Bezerra FF. Physical activity benefits bone density and bone-related hormones in adult men with cervical spinal cord injury. Eur J Appl Physiol 2012; 112: 3179-3186
Chen SC, Lai CH, Chan WP, Huang MH, Tsai HW, Chen JJ. Increases in bone mineral density after functional electrical stimulation cycling exercises in spinal cord injured patients. Disabil Rehabil 2005;27:1337-1341.
Cherniak EP, Levis S, Troen BR. Hypovitaminosis D: A stealthy epidemic that requires treatment. Geriatrics 2008;63:24-30.
Craven BC Robertson LA, McGillivray CF , and Adachi JD . Detection and treatment of sublesional osteoporosis after people with spinal cord injury Topics in SCI Rehabil 2009: 14(4):1-22.
Dudley-Javoroski S, Saha PK, Liang G, Li C, Gao Z, and Shields RK. High dose compressive loads attenuate bone mineral loss in humans with spinal cord injury. Osteoporos Int 2012; 23:2335- 2346.
Dudley-Javoroski S, and Shields RK. Active-resisted stance modulates regional bone mineral density in humans with spinal cord injury. Journal of Spinal Cord Medicine 2013; 36: 191-199.
Dudley-Javoroski S, and Shields RK. Asymmetric bone adaptations to soleus mechanical loading after spinal cord injury. J Musculoskelet Neuronal Interact. 2008;8:227-38.
Dudley-Javoroski S, and Shields RK. Does estimation and surveillance of mechanical loading interventions for bone loss after spinal cord injury. Phys Ther 2008; 88: 387-96.
Eser P, de Bruin ED, Telley I, Lechner HE, Knecht H, Stussi E. Effect of electrical stimulation-induced cycling on bone mineral density in spinal cord-injured patients. Eur J Clin Invest 2003;33:412-419.
Eser P, Frotzler A, Zehnder Y, Denoth J. Fracture threshold in the femur and tibia of people with spinal cord injury as determined by peripheral quantitative computed tomography. Arch Phys Med Rehabil. 2005;86:498-504.
Eser P, Schiessl H, Willnecker J. Bone loss and steady state after spinal cord injury: a cross-sectional study using pQCT. Journal of Musculoskeletal Neuronal Interactions 2004;4:197-198
Ford ES, Ajani UA, McGuire LC, Liu S. Concentrations of serum vitamin D and the metabolic syndrome among U.S. adults. Diabetes Care 2005;28:1228-30.
Frotzler A, Coupaud S, Perret C, Kakebeeke TH, Hunt KJ, Eser P. Effect of detraining on bone and muscle tissue in subjects with chronic spinal cord injury after a period of electrically-stimulated cycling: A small cohort study. Journal of Rehabilitation Medicine 2009; 41: 282-285.
Giangregorio LM, Hicks AL, Webber CE, Phillips SM, Craven BC, Bugaresti JM, et al. Body weight supported treadmill training in acute spinal cord injury: impact on muscle and bone. Spinal Cord 2005;43:649-657.
Giangregorio LM, Webber CE, Phillips SM, Hicks AL, Craven BC, Bugaresti JM, et al. Can body weight supported treadmill training increase bone mass and reverse muscle atrophy in individuals with chronic incomplete spinal cord injury? Appl Physiol Nutr Metab. 2006;31:283-291.
Heaney RP. Lessons for nutritional science from vitamin D. Am J Clin Nutr 1999;69:825-6
Holick MF. Vitamin D: Important for prevention of osteoporosis, cardiovascular heart disease, type I diabetes, autoimmune diseases, and some cancers. South Med J 2005;98:1024-7.
Hummel K, Craven BC, Giangregorio L. Serum 25(OH)D, PTH and correlates of suboptimal 25(OH)D levels in persons with chronic spinal cord injury. Spinal Cord 2012;50:812-6.
Mathieu C, Gysemans C, Giulietti A, Bouillon R. Vitamin D and diabetes. Diabetologia 2005;48:1247-57.
Melchiorri G, Andreoli A, Padura E, Sorge R, De Lorenzo A. Use of vibration exercise in spinal cord injury patients who regularly practice sport. Funct Neurol. 2007;22:151-154
Mohr T, Podenphant J, Biering-Sorensen F, Galbo H, Thamsborg G, Kjaer M. Increased bone mineral density after prolonged electrically induced cycle training of paralyzed limbs in spinal cord injured man. Calcif Tissue Int 1997;61:22-25.
Snijder MB, van Dam RM, Visser M, Deeq DJ, Dekker JM, Bouter LM, et al. Adiposity in relation to vitamin D status and parathyroid hormone levels: a population-based study in older men and women. J Clin Endocrinol Metab 2005;90:4119-23.
Warden SJ, Bennell KL, Matthews B, Brown DJ, McMeeken JM, Wark JD. Efficacy of low intensity pulsed ultrasound in the prevention of osteoporosis following spinal cord injury. Bone 2001;29:431-6.
Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr 2000;72:690-3.
Zhou XJ, Vaziri ND, Segal JL, Winer RL, Eltorai I, Brunnemann BS. Effects of chronic spinal cord injury and pressure ulcer on 25(OH)-vitamin D levels. J Am Paraplegic Soc 1993;16:9-13
Image credits:
- Osteoparoz by Aisha Huseynova. CC BY-SA 4.0, via Wikimedia Commons.
- Cdm hip fracture 343 by Booyabazooka. CC BY-SA 3.0, via Wikimedia Commons.
- Soy Beans by Jessica and Lon Binder. CC BY-NC-ND 2.0, via Flickr.
- Steamed Kale by Laurel F. CC BY-SA 2.0, via Flickr.
- Broccoli by Steffen Zahn. CC BY 2.0, via Flickr.
- Shiitake Chinese Mushrooms by Artizone. CC BY-NC-ND 2.0, via Flickr.
- Fracture by fahmionline, ID. CC BY 3.0 US, via The Noun Project.
- Bone density machine by bwaters23. CC BY-NC-SA 2.0, via Flickr.
- Vitamin D pills by Laura Dahl. CC BY-NC-ND 2.0, via Flickr.
- Bone density by Eucalyp. [CC BY 3.0 US.
- Functional Electrical Stimulation Therapy for walking ©MilosRPopovic, CC BY-SA 4.0.
- Body weight-supported treadmill training with HAL Robot Suit exoskeleton by Oliver Jansen. CC BY-NC-ND 4.0.