Author: Kelsey Zhao | Reviewer: James Milligan | Published: 19 March 2025 | Updated: ~
SCIRE would like to acknowledge the staff at Spinal Cord Injury BC who contributed invaluable knowledge and experience to the development of this article.
Key Points
- Primary care providers (PCPs) help manage your health over a lifetime. They can diagnose and treat common health concerns and coordinate specialist health care.
- See your PCP whenever you have a concern about your health and discuss the possibility of annual check-ups.
- In this article, we provide a thorough guide to preparing for an appointment with a PCP after spinal cord injury.
- Health checklists can help you and your PCP make sure routine tests and screenings are done.
- There are many online resources and local organizations your PCP can consult to learn more about providing care to people with spinal cord injury.
 Primary care providers (PCPs) take care of the day-to-day health of people at all stages of life. They are often the first contact when someone has a non-emergency health concern. This person is often a family doctor, but the role can also be filled by a nurse practitioner, physician assistant. They play a central role in the care team for people with spinal cord injury (SCI) and you will maintain a relationship with your PCP for many years. The responsibilities of a PCP include:
Primary care providers (PCPs) take care of the day-to-day health of people at all stages of life. They are often the first contact when someone has a non-emergency health concern. This person is often a family doctor, but the role can also be filled by a nurse practitioner, physician assistant. They play a central role in the care team for people with spinal cord injury (SCI) and you will maintain a relationship with your PCP for many years. The responsibilities of a PCP include:
- Diagnose and treat common health conditions.
- Encourage and provide advice for a healthy lifestyle.
- Conduct preventative screenings, tests, and checks.
- Refer more complex or specific problems to specialists or programs.
- Coordinate the care you receive from specialists, programs, etc.
People with SCI should see a PCP whenever there is a health concern that needs to be addressed. Due to complex health issues, people with SCI should discuss with their PCP whether an annual physical check-up would be suitable.
If you have a health concern and do not have or cannot reach a PCP, consider virtual health services, telehealth services, and walk-in clinics. If you need immediate care, please visit an urgent care/treatment centre. If your condition is severe or life-threatening, go to your nearest Emergency Room or call your regional emergency phone number.
If you do not have a PCP, find out if there is a community or government registry that will put you on a waitlist to find one.
Go to an urgent care/urgent treatment centre if…
- You need immediate care, and you cannot get an appointment with your PCP soon enough (for example, an infection or pressure injury that will get worse with time).
 Go to the emergency room or call your regional emergency number if…
Go to the emergency room or call your regional emergency number if…
- Your condition is getting worse very quickly.
- You condition is life-threatening.
- You have autonomic dysreflexia that is not responding well to treatment.
- The problem is time-sensitive, and you cannot get an appointment with your PCP soon enough and there is no urgent care centre nearby.
Appointments with PCPs are often short in time. This guide offers recommendations to help make the most of your appointment. Most PCPs do not have many patients with SCI and are not familiar with SCI-related health care needs. Although people with SCI should not be responsible for educating others on SCI, being on top of your own needs is important. Becoming an expert in your own health can help you work with your PCP as a team and keep you healthy.
Write down what you want to address in the appointment
- Current health concerns. Gather information to try and understand the problem, what may be causing it, and possible solutions

- Questions you have about your health or potential treatments/therapies
- Prescriptions that need to be refilled
- Forms and referrals that need to be filled out and signed. For referrals to programs, check that you meet the eligibility requirements. If a referral letter is required, it may speed things along to present an initial draft of the letter to your PCP.
It is possible that all you concerns cannot be addressed in a single appointment. Set priorities by keeping in mind which concerns you want addressed as soon as possible and which ones can wait for another appointment.
Bring up to date medical and health information
Make sure your PCP is up to date on your medical history. For your own records, it can be helpful to keep a folder for your personal medical and health information. This could be a physical folder or a digital one. These records may include:
- A health journal: Keep a journal of ongoing health concerns, the symptoms you are experiencing, and your day-to-day activities. This gives your doctor more information to better understand and address the issue (for example, if you are experiencing persistent urinary tract infections, a bladder journal might help you find the root cause). The SCI Health Toolkit App is a free, easy-to-use tool designed to help you track and monitor health changes, and walk you through health checks.
- Medications: Note the name of the medication, the dose and when a refill is needed. Free apps like the Medisafe App can help you keep track of your medications.
- Other treatments or supplements: Include any over-the-counter medication, vitamins, and natural remedies that you are taking. Note any alternative medicine treatments you are using.
- Tests screenings: Keep track of routine tests/screening and when the next one should be scheduled. Keep a record of test results and imaging results if available.
Accessibility
If this is your first appointment with your PCP since your injury, you may need to phone or visit their office to ask about accessibility.
Building accessibility
- Accessible parking
- Accessible routes into and throughout the building
- Automatic power doorways
Medical equipment accessibility
- Adjustable height accessible exam table
- Transfer and lift equipment
- Wheelchair accessible scales
Scheduling flexibility
- Appointments later in the day
- Appointments scheduled around other health-related commitments like physiotherapy or a bowel routine.
- Longer appointments to accommodate complex health issues, transfers, skin inspections etc.
- Virtual or telephone appointments for certain concerns.
Physical Exams
There are many screenings, tests, and checks that require an in-person procedure where your body is examined by looking, feeling, using medical tools, or taking a sample of cells. You may also be required to transfer for the procedure. Being prepared and informed for these procedures can make your experience safer and more comfortable. Some tips to keep in mind:
Equipment for exams
- If accessible equipment like an adjustable exam table is not available, bring a caregiver, friend, or family who can help you transfer safely and stay at the side of the table to prevent falls.
- If accessible equipment is required for the procedure, you or your PCP may need to reach out to get the procedure done at another clinic or hospital that has the equipment.
Health complications during exams
- Before starting, have a conversation with your PCP about issues that might come up during the procedure and how to address them.
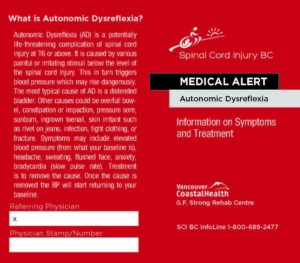
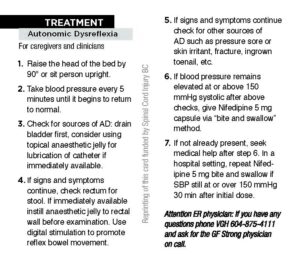
- For people with an injury above T6, a procedure below the injury can trigger autonomic dysreflexia (AD). Inform your PCP about the triggers, symptoms and how to manage your AD. Consider measuring blood pressure before and after the procedure to monitor for AD.
- Depending on your bowel and bladder dysfunction, accidents may happen during procedures. Empty the bowel bladder before an exam of the pelvic region and let your PCP know if you may have an accident during the procedure.
- If you experience muscle spasms that could affect the procedure, discuss triggers and how to manage spasticity with your PCP.
If a physical exam is not necessary, virtual appointments and phone appointments with your PCP may be a suitable option.
Refer to our articles on Autonomic Dysreflexia, Urinary Tract Infections, and Spasticity for more information!
Practical Tips
- Ask if a note can be added to your profile about physical disability and use of mobility aid(s) so that staff knows to book you in an accessible exam room.
- Make sure everyone who provides health care to you sends notes, images, and results to your PCP, who is responsible for coordinating your care.
- Be aware of other services in the community (such as labs, imaging centres, and specialist offices) that have accessible equipment.
- Wallet cards are small cards available for free that provide basic information on common SCI complications: autonomic dysreflexia, urinary tract infections, and pressure injuries. Keep them on you to give to your PCP at an appointment or to first responders and paramedics in an emergency. Wallet cards can be printed at home or mailed from livingwithsci.ca/wallet-information-cards.
- Request a “standing order” for laboratory tests done often like bloodwork and urine tests so that you don’t need to make an appointment every time.
- Request clean empty urine containers for when you need to test for urinary tract infection. You may need to explain to your PCP that urinary tract infections are common for people with SCI.
| People with SCI have a higher risk for antibiotic resistance. Avoid using antibiotics to prevent UTI or to treat unspecific symptoms that could be caused by something else. Inappropriate use of antibiotics can lead to infections with antibiotic resistant bacteria, that cannot be treated with common medications. |
During the appointment
- Take notes or ask if you can record the appointment so you do not have to worry about remembering everything your PCP says and follow up with tasks as needed.
- Ask questions or ask for more information if you are unsure or don’t understand something.
- If you are nervous, bring a caregiver/friend/family member who can help take notes and help advocate for your needs.
Reach out to other people with SCI/peer support programs
Attending peer programs or calling a help line run by SCI organizations can connect you with someone who can help you prepare for the appointment. Often, another person with SCI will have had similar health issues and can provide advice on how to address it with your PCP. There may also be people or programs that can help you prepare documents or do research.
SCI-specific health checks
Checklists made for people with SCI can help keep you and your PCP on top of routine exams and tests. They can also help you find the language to ask and talk about health issues.
The American Spinal Injury Association (ASIA) has checklists for people with SCI.
- Annual Health Maintenance Checklist for SCI-specific health checks that should be done on a regular basis.
- Episodic Care Tips Checklist for addressing specific SCI-related complications.
 If your PCP is interested in more in-depth information, case studies, advice, and guidelines for these checklists and SCI-specific care, they can check out the Primary Care Article series from ASIA’s peer-reviewed journal. For brief overviews on managing common SCI complications in primary care, they can visit the Primary Care section on the SCIRE Professional website.
If your PCP is interested in more in-depth information, case studies, advice, and guidelines for these checklists and SCI-specific care, they can check out the Primary Care Article series from ASIA’s peer-reviewed journal. For brief overviews on managing common SCI complications in primary care, they can visit the Primary Care section on the SCIRE Professional website.
Visit SCIRE Professional for more information on Primary Care for SCI
Standard health checks
PCPs should also do the same general health checks and routine screenings that they would for any other patient. The College of Family Physicians of Canada provides Preventative Care Checklists.
Sexual and reproductive health care
Both the public and some health professionals can have the misconception that people with physical disabilities are not sexually active, at risk for sexually transmitted infections (STIs), interested in sexual activity, or interested in having kids. Initiate a conversation with your PCP if you have questions or concerns about sexual health (challenges with sexual activity, contraception, sexually transmitted diseases), reproductive health (fertility, pregnancy, family planning), or menstruation/menopause.
If your PCP is interested in learning more to better care for people with SCI and people with disabilities, there are many resources they can consult. See a selection of free resources below:
Online resources
American Spinal Injury Association (ASIA) – SCI Healthcare Resources for Primary Care Providers
asia-spinalinjury.org/primary-care
Online hub providing a variety of resources for family physicians caring for patients with spinal cord injury from guides to make a health facility accessible, to SCI care information, to patient education materials.
Americans with Disabilities Act (ADA) – Access to Medical Care for Individuals With Mobility Disabilities
ada.gov/resources/medical-care-mobility
Online guide to making a health care facility accessible to people with mobility disabilities. Includes answers to commonly asked questions.
Spinal Cord Injury Research Evidence (SCIRE) Professional – Primary Care
SCIRE Professional provides systematic reviews of spinal cord injury (SCI) research, to allow researchers and health professionals to guide their practice based on current best evidence. This includes a section specifically for primary care providers.
Spinal Cord Injury Research Evidence (SCIRE) Community
SCIRE Community provides free information about spinal cord injury research that is written in everyday language.
Model Systems Knowledge Translation Center (MSKTC) – Spinal Cord Injury Factsheets
Online factsheets providing information on the changes that come with living with spinal cord injury.
International Spinal Cord Society (ISCoS) – Global Education Initiative
Online learning module for health care providers on rehabilitation and management for SCI.
Connect with SCI organizations and specialists
Local non-profit SCI organizations, rehabilitation centres, and SCI centres can be excellent resources for region-specific information and advice. Regular communication with SCI-related specialists can also be helpful for both coordinating care and sharing knowledge.
Primary care providers have an invaluable role in the care team for people with SCI. They provide diagnoses, treatments, advice, referrals to specialist services, and conduct preventative screenings and tests.
Being prepared for your appointment and staying on top of your health concerns can go a long way in helping your PCP address your concerns. Work together with your PCP to figure out the best way to coordinate your appointments, find solutions for accessibility, and address your health concerns.
There are many free resources available to help people with SCI stay on top of their health and help PCPs provide care to their patients with SCI.
For a review of how we assess evidence at SCIRE Community and advice on making decisions, please see SCIRE Community Evidence.
SCIRE Community. “Autonomic Dysreflexia”
SCIRE Community. “Urinary Tract Infections”
SCIRE Community. “Spasticity”
SCI-BC Wallet Cards
Health Tracking Mobile Apps:
Health Checklists:
- American Spinal Injury Association Annual Health Maintenance Checklist
- American Spinal Injury Association Episodic Care Tips Checklist
- College of Family Physicians of Canada Preventative Care Checklists
Resources for Primary Care Providers:
- American Spinal Injury Association Primary Care Article series
- American Spinal Injury Association SCI Healthcare Resources for Primary Care Providers
- Americans with Disabilities Act Access to Medical Care for Individuals with Mobility Disabilities
- SCIRE Professional Primary Care
- Model Systems Knowledge Translation Center Spinal Cord Injury Factsheets
- International Spinal Cord Society Global Education Initiative
Evidence for “What is a primary care provider?” is based on:
Holland, K. (2023, June 29). Types of Doctors: PCP vs. Family Doctor vs. Internist. https://www.healthline.com/find-care/articles/primary-care-doctors/types-of-doctors#internist
McColl, M. A., Aiken, A., McColl, A., Sakakibara, B., & Smith, K. (2012). Primary care of people with spinal cord injury: scoping review. Canadian Family Physician Medecin de Famille Canadien, 58(11), 1207–1216, e626-35.
Evidence for “When should I see my primary care provider?” is based on:
McColl, M. A., Aiken, A., McColl, A., Sakakibara, B., & Smith, K. (2012). Primary care of people with spinal cord injury: scoping review. Canadian Family Physician Medecin de Famille Canadien, 58(11), 1207–1216, e626-35.
Evidence for “How do I prepare for an appointment?” is based on:
How to Prepare for a Doctor’s Appointment | National Institute on Aging. (2020, February 3). NIH National Institue on Aging. https://www.nia.nih.gov/health/medical-care-and-appointments/how-prepare-doctors-appointment
Making the Most of Your Appointment | HealthLink BC. (2022, November 14). Healthlink BC. https://www.healthlinkbc.ca/health-topics/making-most-your-appointment
Access to Medical Care for Individuals with Mobility Disabilities | ADA.gov. (2020, June 26). https://www.ada.gov/resources/medical-care-mobility/
Phelan, S. T., & Unser, C. (2020, March 13). Eight tips to improve outpatient visits for spinal cord injury patients. https://www.contemporaryobgyn.net/view/eight-tips-improve-outpatient-visits-spinal-cord-injury-patients
Evidence for “What should I ask my primary care provider to check?” is based on:
Hough, S., Cordes, C. C., Goetz, L. L., Kuemmel, A., Lieberman, J. A., Mona, L. R., Tepper, M. S., & Varghese, J. G. (2020). A Primary Care Provider’s Guide to Sexual Health for Individuals With Spinal Cord Injury. Topics in Spinal Cord Injury Rehabilitation, 26(3), 144–151. https://doi.org/10.46292/sci2603-144
Image credits
- Doctor smiling ©SCIRE, CC BY-NC 4.0
- Ambulance by Dahlia nur aini, the Noun Project
- Question by Yunita Bela, the Noun Project
- Automatic doorway ©SCIRE, CC BY-NC 4.0
- Accessible parking ©SCIRE, CC BY-NC 4.0
- Adjustable-height exam table by S. Department of Justice (Disability Rights Section)
- Autonomic Dysreflexia Wallet Card by Spinal Cord Injury BC
- Notes by Qadeer Hussain, the Noun Project
- Checklist by Anggara Putra, the Noun Project