Author: Dominik Zbogar | Reviewer: Giorgio Scivoletto | Published: 30 April 2025 | Updated: ~
Key Points
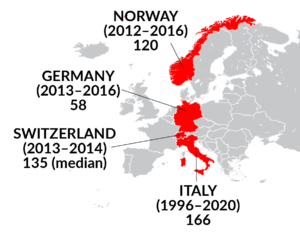
- The length of stay (LOS) in spinal cord injury (SCI) inpatient rehabilitation varies widely between countries, from 41 days in USA to 135 in Switzerland.
- Between countries, LOS varies due to cultural, economic, and health infrastructure factors.
- Within a country, LOS varies depending on the severity/level of injury, age, complications and pre-existing conditions, and functional goals.
- Inpatient SCI rehab LOS has been decreasing over decades for reasons including advancements in medical and surgical care, technology and equipment, changing injury characteristics and demographics, changes in healthcare policy and insurance, changes in rehab practice and increased focus on community-based (outpatient) care.
How long people receive inpatient rehabilitation for spinal cord injury (SCI) is called rehabilitation length of stay (LOS). Rehabilitation is often part of the care pathway for a SCI patient. From initial injury to discharge into the community, the care pathway typically involves acute care, rehabilitation and discharge into the community, each addressing different aspects of recovery. Progression through the care pathway is not always seamless. For example, the interval before rehabilitation can involve more than one acute facility, or a patient may be readmitted to acute care while in rehabilitation.
Acute care
This period of early health care after a major injury or illness includes both emergency services in the community (like ambulance and paramedic services) and treatment at an acute care hospital. During this time, serious and urgent health problems are addressed to stabilize the patient.
Average acute care LOS
USA
30 days in the 1970s to 19 days since 2015
Canada
Between 25-37 days depending on injury severity/level
Rehabilitation
When a person is medically stable, most people leave acute care and are transferred to a “rehabilitation center” or “rehabilitation hospital”, where they focus on recovering and developing the skills for living with an SCI long-term. In some cases, the acute and rehabilitation services are in the same hospital. In other cases, the rehabilitation hospital is a separate centre.
Inpatient rehabilitation
Inpatient rehabilitation involves staying at a rehabilitation centre and receiving full-day programming.
Outpatient rehabilitation
Outpatient rehabilitation has individuals living in the community and visiting the rehabilitation centre for regular services. This phase can continue for several months, focusing on further functional improvements, community reintegration, and vocational training.
Community
Returning to community living after an SCI involves planning for suitable living arrangements after rehabilitation and for a possible return to previous activities. Some return home while others may go to a long-term or transitional care facility. This is done with support from the whole health team and may be led by a social worker or discharge planner.
Refer to our article on Understanding Rehabilitation for more information!
 The LOS for SCI rehabilitation varies significantly between countries due to differences in healthcare systems, insurance models, resource availability, economic factors, cultural and social factors, and adaptation of evidence-based rehabilitation practices. These factors are discussed in detail in the next sections.
The LOS for SCI rehabilitation varies significantly between countries due to differences in healthcare systems, insurance models, resource availability, economic factors, cultural and social factors, and adaptation of evidence-based rehabilitation practices. These factors are discussed in detail in the next sections.
In this section, we show rehab LOS values for select countries around the world since 2010. The LOS is counted in average days (unless we indicate otherwise). Text descriptions provide details about subgroups while images provide a summary value.
North America
United States (2020 – 2023)
41 days (median)
Canada (2021)
- Traumatic SCI:
- Complete tetraplegia: 112
- Incomplete tetraplegia: 82
- Complete paraplegia: 73
- Incomplete paraplegia: 65
- Non-traumatic SCI
- Complete tetraplegia: 95
- Incomplete tetraplegia: 67
- Complete paraplegia: 70
- Incomplete paraplegia 55

Europe
Germany (2013 – 2016)
57.7
Italy (1996 – 2020)
- With complications: 180.4 (93)
- Without complications: 154.5 (85)

Norway (2012 – 2016)
120
Switzerland (2013 – 2014)
135 (median)
Middle East
Saudi Arabia (2009 – 2014)
- Traumatic SCI: 85
- Non-traumatic SCI: 64
Asia
China (2010 – 2019)
113.5
 Australia (2010 – 2011)
Australia (2010 – 2011)
130 (median)
In the USA the median rehabilitation LOS has decreased from 91 days in 1972-1979 to 41 days in 2020-2023.
This decrease over the years is a trend also seen in other high-income countries (HIC). This decrease in LOS for inpatient SCI rehabilitation may be due to a combination of several factors reflecting both the evolution of care practices and the economic realities of healthcare delivery:
Advancements in medical and surgical care
Early surgical intervention, better acute care, and improved stabilization techniques post-injury may allow for quicker transitions from acute care to rehabilitation or community settings. This is supported by studies showing that early surgery may lead to shorter LOS in acute care, which could impact how soon patients are admitted to rehabilitation.
Changes in healthcare policy and funding
Economic incentives in healthcare systems, particularly in HICs, have pushed for shorter hospital stays to manage costs. Insurance policies and healthcare reforms often aim to reduce LOS to lower expenditure, which has influenced rehabilitation practices.
Changes in rehabilitation practices
Intensity of rehabilitation and not just LOS can influence outcomes. In the US for example, some rehab facilities have a three-hour rule where at least three hours of intensive rehab therapy per day, at least five days a week. This has led to a focus on maximizing therapy within a shorter period, thereby reducing LOS while still aiming for similar or better outcomes. Rehabilitation methods have evolved, emphasizing more intensive, shorter-duration therapies that aim to achieve functional gains more quickly. This includes the use of early, intensive physical therapy, occupational therapy, and other modalities that can lead to earlier discharges.
Technological and equipment advances
The availability of advanced assistive devices, home adaptations, and technology for home use allows individuals with SCI to manage more aspects of their care at home, reducing the need for extended inpatient stays.
Increased focus on community-based rehabilitation
There is a growing trend towards discharging patients to community settings earlier for continued rehabilitation, supported by home health services, outpatient programs, or community-based rehabilitation centers. This shift is partly due to evidence showing that community integration and social participation can be maintained or even enhanced with earlier discharge.
Changes in demographic and injury characteristics
Changes in the demographics of those injured, and the level and severity of SCI may also play a role. An increase in SCI among older people may increase rehab periods. Conversely, a trend towards more effective complication prevention could lead to shorter rehabilitation periods. Also, a trend towards incomplete SCI could lead to shorter rehabilitation periods. However, this trend towards incomplete SCI is not always reflected in a reduction of LOS as a sizeable subset of those with incomplete tetraplegia suffer from central cord syndrome which has very poor independence recovery.
The next section provides more information on these demographic factors.
Severity of injury
- Complete SCI (no sensory or motor function below the level of injury) typically requires longer stays.
- Incomplete SCI (some preserved function below the level of injury) may involve shorter stays, but this varies widely depending on the extent of motor and sensory recovery.
Level of injury
- Higher-level injuries (cervical injuries) tend to result in more significant functional impairments, leading to longer stays.
- Lower-level injuries (thoracic or lumbar injuries) may require less rehabilitation time, though patients still need extensive care for functional independence.
Refer to our article on SCI Basics for more information!
Complications
Patients who develop complications like pressure ulcers, respiratory issues, or infections often experience prolonged rehabilitation stays but without any improvement in independence. Also, medical complications in rehabilitation are a predictor of rehospitalization in the period after rehabilitation discharge.
Age and pre-existing conditions
Older patients or those with pre-existing health conditions may require longer rehabilitation. The increased age of patients can often mean that caregivers are older and are themselves unable to assist their partner, complicating discharge planning.
Functional goals
Rehabilitation LOS can be extended or shortened based on the patient’s ability to achieve specific functional milestones, such as regaining mobility, independence in self-care, or achieving vocational goals.
Early versus late decompression surgery
Early surgery is associated with a small decrease in acute care LOS. However, there is no association between early surgery and rehabilitation LOS. More research is needed to support the finding as the 2 studies on this topic had very imprecise estimates.
Early versus late admission to rehab
Research has shown that SCI patients without effective rehabilitation in the six months following injury had a significantly longer length of stay in rehabilitation (as well as a notably lower percent increase in motor recovery from admission to discharge). Additionally, it has been shown that early rehabilitation is effective in accelerating and promoting improvement in activities of daily living.
Barriers to discharge
Sometimes, individuals remain in the rehabilitation setting after their rehabilitation goals have been met and even when they are deemed ready for discharge. For example, family deliberations, procurement of supported care or services, provision of required equipment, need for residential care, a lack of accessible housing or a requirement for home modifications can all result in an extended stay in rehabilitation. Architectural barriers in heritage buildings and neighbourhoods in old European cities can be a significant barrier to discharge that the North American reader may not have considered.
Specialized centres of care
When patients have access to specialized centres of care there is a decrease in mortality and LOS. However, relatively few specialized SCI rehabilitation centers exist globally and they are generally concentrated in high-income countries. Examples include the acute care centres and rehabilitation units that are part of the Spinal Cord Injury Model Systems in USA and the Rick Hansen Spinal Cord Injury Registry in Canada. The global lack of specialist rehabilitation skills in low-income countries can result in inadequate initial management of SCI cases at the receiving hospital and a rapid development of secondary complications, ultimately contributing to a longer length of hospital stay and potentially poorer functional outcomes or even death.
Healthcare models
LOS can be influenced by the healthcare models. In one study from 2005 comparing USA, Canada and Italy, it was found that LOS in USA was influenced by third party payer requirements for discharge where patients are discharged as soon as they achieve a minimally acceptable level of mobility. In contrast, for Italy and Canada, length of stay in rehabilitation was based primarily on patients achieving the highest level of independence feasible. Today, 20 years later, while the health care systems in many countries are intended to allow continued rehabilitation (inpatient or outpatient) until patients reach a mobility plateau or maximal mobility independence, there is tremendous financial pressure to discharge patients as quickly as possible.
Healthcare differences between HICs and LMICs
While there is much variability even within HICs and low- and middle-income countries (LMICs), the health care infrastructure in HICs supports a more structured and systematic approach to SCI rehabilitation with clear protocols for early intervention, which can reduce LOS. In many LMICs, the infrastructure might be less developed, leading to inefficiencies in care delivery. Additionally, insurance coverage and health policies in HICs often allow for longer recovery times in rehabilitation settings, while in LMICs, financial constraints might force earlier discharge.
HICs tend to have better resources in terms of advanced medical equipment, trained personnel, and ongoing support services post-discharge, which can facilitate quicker rehabilitation and shorter hospital stays. In LMICs, economic conditions can directly impact LOS as lack of funding and constraints in resources mean that rehabilitation might be slower or less effective due to a lack of necessary equipment, like robotic rehabilitation devices, trained staff, and lack of systems for post-discharge care, including home care services, community support, and outpatient rehabilitation, which could reduce the need for prolonged inpatient stays. Environmental factors like access to transportation for follow-up care or the availability of accessible living environments also play a role.
Cultural attitudes towards disability and rehabilitation can influence LOS. In some LMICs, there may be cultural barriers to accepting or seeking out rehabilitation services, which could prolong hospital stays. Social factors include lower awareness of SCI care, which might delay initial treatment and extend the rehabilitation period.
 The evidence for how LOS affects individual functional improvement at discharge is mixed. Some studies report a longer LOS is associated with increased functional improvement while others report the opposite.
The evidence for how LOS affects individual functional improvement at discharge is mixed. Some studies report a longer LOS is associated with increased functional improvement while others report the opposite.
Longer LOS may allow for additional opportunities for interdisciplinary treatments, patient education, and discharge planning to support transitions in care and reduce risk of re-hospitalization. However, LOS alone does not account for the intensity and quality of rehabilitation. In a hypothetical situation, patients recover their motor function faster and finish their rehabilitation program sooner if the therapy intensity is increased. Also, other factors such as psychological support, and community reintegration efforts play critical roles in long-term outcomes for SCI patients. Time in an inpatient rehabilitation hospital can be disruptive to patients and adjusting sooner to routine at home, say as an outpatient, can accelerate community reintegration efforts.
Note too, that those with the most severe injuries tend to have the longest LOS in rehabilitation, yet their outcomes are often worse than those with shorter LOS and less severe injuries. It would be incorrect to assume then that longer LOS results in worse outcomes. Instead, consider the context of injury/demographic factors (as discussed in the previous sections) when looking at LOS values.
Ideally, the appropriate rehabilitation LOS for any person is determined by collaborative decision-making between the rehabilitation team, the patient, and their family. The ultimate goal is functional independence and quality of life improvement, even if rehabilitation continues in an outpatient or community-based setting.
In reality, rehabilitation LOS is impacted by the many factors discussed in this article. Factors specific to the patient include injury severity, age, medical complications, pre-existing conditions, and their individual recovery progress. Factors beyond the individual patient are those determined by the healthcare system and include how long it takes to be admitted to rehab, barriers to being discharged from rehab, specialized centres of care, and healthcare models. Insurance systems, and economics/resource availability especially play a role in the differences seen between HICs and LMICs. Finally, socio-cultural factors can also play a role, with lower awareness of SCI care or cultural barriers to accepting or seeking out rehabilitation services resulting in delayed initial treatment and extend the rehabilitation period.
Over the decades, rehab LOS has been decreasing. Reasons for this include advancements in surgical care and technologies, changes in rehab practices, increased focus on community-based rehabilitation, less severe injuries and complications, and economic/healthcare system pressures.
SCIRE Community. Emergency and Hospital Care
SCIRE Community. Understanding Rehabilitation
SCIRE Community. SCI Basics
Evidence for “The SCI care pathway” is based on:
Burns, A. S., Santos, A., Cheng, C. L., Chan, E., Fallah, N., Atkins, D., Dvorak, M. F., Ho, C., Ahn, H., Paquet, J., Kwon, B. K., & Noonan, V. K. (2017). Understanding Length of Stay after Spinal Cord Injury: Insights and Limitations from the Access to Care and Timing Project. Journal of Neurotrauma, 34(20), 2910. https://doi.org/10.1089/NEU.2016.4935
NSCISC. (2024). Traumatic Spinal Cord Injury Facts and Figures at a Glance. https://bpb-us-w2.wpmucdn.com/sites.uab.edu/dist/f/392/files/2024/06/Facts_and_Figures_2024_Final.pdf
Praxis Spinal Cord Institute. (2022). Rick Hansen Spinal Cord injury Registry: A look at Spinal Cord Injury in Canada in 2022. https://praxisinstitute.org/wp-content/uploads/2024/10/Praxis-Registry-Annual-Report-2022.pdf
Evidence for “Typical rehab LOS around the world” is based on:
National Spinal Cord Injury Statistical Center. (2023, August). 2023 Annual Statistical Report for the Spinal Cord Injury Model Systems. University of Alabama at Birmingham. https://bpb-us-w2.wpmucdn.com/sites.uab.edu/dist/f/392/files/2024/06/9.4_SAS_System_Output.pdf
Noonan, V. K. (2023). A Look at Spinal Cord Injury in Canada: Rick Hansen Spinal Cord Injury Registry (RHSCIR) – 2021 SCI Data Summary. Topics in Spinal Cord Injury Rehabilitation, 29(Supplement), 165–170. https://doi.org/10.46292/SCI23-00031SPonfick 2017
Scivoletto, G., Marcella, M., Floriana, P., Federica, T., & Marco, M. (2020). Impact of complications at admission to rehabilitation on the functional status of patients with spinal cord lesion. Spinal Cord 2020 58:12, 58(12), 1282–1290. https://doi.org/10.1038/s41393-020-0501-zHalvorsen 2018
Franceschini, M., Bonavita, J., Cecconi, L., Ferro, S., Pagliacci, M. C., Ferro, S., Bellentani, M., Franceschini, M., Cavina, A., Biggeri, A., Cecconi, L., De Iure, F., Gordini, G., Redaelli, T., Actis, M. V., Del Popolo, G., Bertagnoni, G., Avesani, R., & Falabella, V. (2020). Traumatic spinal cord injury in Italy 20 years later: current epidemiological trend and early predictors of rehabilitation outcome. Spinal Cord 2020 58:7, 58(7), 768–777. https://doi.org/10.1038/s41393-020-0421-y
Mahmoud, H., Qannam, H., Zbogar, D., & Mortenson, B. (2017). Spinal cord injury rehabilitation in Riyadh, Saudi Arabia: Time to rehabilitation admission, length of stay and functional independence. Spinal Cord, 55(5), 509. https://doi.org/10.1038/SC.2016.165
Zhang, Z., Wang, F., & Wu, Y. (2020). Factors affecting length of stay in hospital of patients with traumatic spinal cord injury in China. Journal of Rehabilitation Medicine, 52(11), 1–5. https://doi.org/10.2340/16501977-2761
Tovell, A., & Harrison, J. (2018). Spinal Cord Injury, Australia, 2010-2011. Injury research and statistics series no. 80. Cat. no. INJCAT 156.
Evidence for “How has rehab LOS changed over the years” is based on:
National Spinal Cord Injury Statistical Center. (2023, August). 2023 Annual Statistical Report for the Spinal Cord Injury Model Systems. University of Alabama at Birmingham. https://bpb-us-w2.wpmucdn.com/sites.uab.edu/dist/f/392/files/2024/06/9.4_SAS_System_Output.pdf
Fehlings, M. G., Hachem, L. D., Tetreault, L. A., Skelly, A. C., Dettori, J. R., Brodt, E. D., Stabler-Morris, S., Redick, B. J., Evaniew, N., Martin, A. R., Davies, B., Farahbakhsh, F., Guest, J. D., Graves, D., Korupolu, R., McKenna, S. L., & Kwon, B. K. (2024). Timing of Decompressive Surgery in Patients With Acute Spinal Cord Injury: Systematic Review Update. Global Spine Journal, 14(3 Suppl), 38S. https://doi.org/10.1177/21925682231197404
Mac-Thiong, J. M., Feldman, D. E., Thompson, C., Bourassa-Moreau, E., & Parent, S. (2012). Does Timing of Surgery Affect Hospitalization Costs and Length of Stay for Acute Care following a Traumatic Spinal Cord Injury? Https://Home.Liebertpub.Com/Neu, 29(18), 2816–2822. https://doi.org/10.1089/NEU.2012.2503
Bryden, A. M., & Gran, B. (2024). Seeking sufficient and appropriate care during the first year after spinal cord injury: a qualitative study. Spinal Cord 2024 62:5, 62(5), 241–248. https://doi.org/10.1038/s41393-024-00974-x
Burns, A. S., Santos, A., Cheng, C. L., Chan, E., Fallah, N., Atkins, D., Dvorak, M. F., Ho, C., Ahn, H., Paquet, J., Kwon, B. K., & Noonan, V. K. (2017). Understanding Length of Stay after Spinal Cord Injury: Insights and Limitations from the Access to Care and Timing Project. Journal of Neurotrauma, 34(20), 2910. https://doi.org/10.1089/NEU.2016.4935
Forrest, G., Reppel, A., Kodsi, M., Smith, J., & Enix, D. (2019). Inpatient rehabilitation facilities: The 3-hour rule. Medicine, 98(37), e17096. https://doi.org/10.1097/MD.0000000000017096
Kao, Y. H., Chen, Y., Deutsch, A., Wen, H., & Tseng, T. S. (2021). Rehabilitation length of stay and functional improvement among patients with traumatic spinal cord injury. Spinal Cord 2021 60:3, 60(3), 237–244. https://doi.org/10.1038/s41393-021-00686-6
Lamontagne, M. E., Gagnon, C., Allaire, A. S., & Noreau, L. (2013). Effect of rehabilitation length of stay on outcomes in individuals with traumatic brain injury or spinal cord injury: a systematic review protocol. Systematic Reviews, 2, 59. https://doi.org/10.1186/2046-4053-2-59
Truchon, C., Fallah, N., Santos, A., Vachon, J., Noonan, V. K., & Cheng, C. L. (2017). Impact of Therapy on Recovery during Rehabilitation in Patients with Traumatic Spinal Cord Injury. Journal of Neurotrauma, 34(20), 2901. https://doi.org/10.1089/NEU.2016.4932
Morone, G., Pirrera, A., Iannone, A., & Giansanti, D. (2023). Development and Use of Assistive Technologies in Spinal Cord Injury: A Narrative Review of Reviews on the Evolution, Opportunities, and Bottlenecks of Their Integration in the Health Domain. Healthcare, 11(11), 1646. https://doi.org/10.3390/HEALTHCARE11111646
Baehr, L. A., Kaimal, G., Hiremath, S. V., Trost, Z., & Finley, M. (2022). Staying active after rehab: Physical activity perspectives with a spinal cord injury beyond functional gains. PLoS ONE, 17(3), e0265807. https://doi.org/10.1371/JOURNAL.PONE.0265807
Kendall, M. B., Amsters, D., Schuurs, S., Borg, D. N., Pershouse, K., & Kuipers, P. (2022). Longitudinal effects of time since injury and age at injury on outcomes of people with spinal cord injury in Queensland, Australia. Spinal Cord, 60(12), 1087. https://doi.org/10.1038/S41393-022-00824-8
Nas, K., Yazmalar, L., Şah, V., Aydin, A., & Öneş, K. (2015). Rehabilitation of spinal cord injuries. World Journal of Orthopedics, 6(1), 8. https://doi.org/10.5312/WJO.V6.I1.8
Scivoletto, Giorgio. (2025) personal communication
Evidence for “Injury/demographic factors influencing rehab LOS” is based on:
Chan, S. S. S., & Chan, A. P. S. (2005). Rehabilitation outcomes following traumatic spinal cord injury in a tertiary spinal cord injury centre: a comparison with an international standard. Spinal Cord 2005 43:8, 43(8), 489–498. https://doi.org/10.1038/sj.sc.3101743
DeVivo, M. J., Kartus, P. L., Stover, S. L., & Fine, P. R. (1990). Benefits of early admission to an organised spinal cord injury care system. Paraplegia, 28(9), 545–555. https://doi.org/10.1038/SC.1990.74
Tooth, L., McKenna, K., & Geraghty, T. (2003). Rehabilitation outcomes in traumatic spinal cord injury in Australia: functional status, length of stay and discharge setting. Spinal Cord 2003 41:4, 41(4), 220–230. https://doi.org/10.1038/sj.sc.3101433
Whiteneck, G., Gassaway, J., Dijkers, M., Backus, D., Charlifue, S., Chen, D., Hammond, F., Hsieh, C. H., & Smout, R. J. (2011). Inpatient treatment time across disciplines in spinal cord injury rehabilitation. The Journal of Spinal Cord Medicine, 34(2), 133. https://doi.org/10.1179/107902611X12971826988011
Whiteneck, G., Gassaway, J., Dijkers, M. P., Heinemann, A. W., & Kreider, S. E. D. (2012). Relationship of patient characteristics and rehabilitation services to outcomes following spinal cord injury: The SCIRehab Project. The Journal of Spinal Cord Medicine, 35(6), 484. https://doi.org/10.1179/2045772312Y.0000000057
Dejong, G., Tian, W., Hsieh, C. H., Junn, C., Karam, C., Ballard, P. H., Smout, R. J., Horn, S. D., Zanca, J. M., Heinemann, A. W., Hammond, F. M., & Backus, D. (2013). Rehospitalization in the First Year of Traumatic Spinal Cord Injury After Discharge From Medical Rehabilitation. Archives of Physical Medicine and Rehabilitation, 94(4), S87–S97. https://doi.org/10.1016/J.APMR.2012.10.037
Scivoletto, Giorgio (2025). personal communication
Evidence for “Healthcare system factors determining rehab LOS” is based on:
Fehlings, M. G., Hachem, L. D., Tetreault, L. A., Skelly, A. C., Dettori, J. R., Brodt, E. D., Stabler-Morris, S., Redick, B. J., Evaniew, N., Martin, A. R., Davies, B., Farahbakhsh, F., Guest, J. D., Graves, D., Korupolu, R., McKenna, S. L., & Kwon, B. K. (2024). Timing of Decompressive Surgery in Patients With Acute Spinal Cord Injury: Systematic Review Update. Global Spine Journal, 14(3 Suppl), 38S. https://doi.org/10.1177/21925682231197404
Ter Wengel, P. V., De Gendt, E. E. A., Martin, E., Adegeest, C. Y., Stolwijk-Swuste, J. M., Fehlings, M. G., Oner, F. C., & Vandertop, W. P. (2022). Impact of Surgical Timing on Motor Level Lowering in Motor Complete Traumatic Spinal Cord Injury Patients. Https://Home.Liebertpub.Com/Neu, 39(9–10), 651–657. https://doi.org/10.1089/NEU.2021.0428
Wilson, J. R., Singh, A., Craven, C., Verrier, M. C., Drew, B., Ahn, H., Ford, M., & Fehlings, M. G. (2012). Early versus late surgery for traumatic spinal cord injury: the results of a prospective Canadian cohort study. Spinal Cord 2012 50:11, 50(11), 840–843. https://doi.org/10.1038/sc.2012.59
Janssen, T. W. J., Van Oers, C. A. J. M., Van Der Woude, L. H. V., & Hollander, A. P. (1994). Physical strain in daily life of wheelchair users with spinal cord injuries. Medicine and Science in Sports and Exercise, 26(6), 661–670. https://doi.org/10.1249/00005768-199406000-00002
Scivoletto, G., Morganti, B., & Molinari, M. (2005). Early versus delayed inpatient spinal cord injury rehabilitation: An Italian study. Archives of Physical Medicine and Rehabilitation, 86(3), 512–516. https://doi.org/10.1016/J.APMR.2004.05.021
Sumida, M., Fujimoto, M., Tokuhiro, A., Tominaga, T., Magara, A., & Uchida, R. (2001). Early rehabilitation effect for traumatic spinal cord injury. Archives of Physical Medicine and Rehabilitation, 82(3), 391–395. https://doi.org/10.1053/APMR.2001.19780
Burns, A. S., Marino, R. J., Kalsi-Ryan, S., Middleton, J. W., Tetreault, L. A., Dettori, J. R., Mihalovich, K. E., & Fehlings, M. G. (2017). Type and Timing of Rehabilitation Following Acute and Subacute Spinal Cord Injury: A Systematic Review. Global Spine Journal, 7(3 Suppl), 175S. https://doi.org/10.1177/2192568217703084
Scivoletto, Giorgio (2025). Personal communication
Parent, S., Barchi, S., LeBreton, M., Casha, S., & Fehlings, M. G. (2011). The Impact of Specialized Centers of Care for Spinal Cord Injury on Length of Stay, Complications, and Mortality: A Systematic Review of the Literature. Journal of Neurotrauma, 28(8), 1363. https://doi.org/10.1089/NEU.2009.1151
Arejan, R. H., Azadmanjir, Z., Ghodsi, Z., Dehghan, H. R., Sharif-Alhoseini, M., Tabary, M., Khaleghi-Nekou, M., Naghdi, K., Vaccaro, A. R., Zafarghandi, M. R., & Rahimi-Movaghar, V. (2022). How Can Policymakers be Encouraged to Support People With Spinal Cord Injury—Scoping Review. Global Spine Journal, 12(4), 732–741. https://doi.org/10.1177/21925682211005406/ASSET/IMAGES/LARGE/10.1177_21925682211005406-FIG3.JPEG
O’Connell, C., Armstrong, J., De la Cerna-Luna, R., Ganvir, S., & Arnillas Brigneti, P. (2024). Perspective of the World Rehabilitation Alliance: Global Strategies to Strengthen Spinal Cord Injury Rehabilitation Services in Health Systems. Healthcare 2024, Vol. 12, Page 2313, 12(22), 2313. https://doi.org/10.3390/HEALTHCARE12222313
Ditunno, P. L., Patrick, M., Stineman, M., Morganti, B., Townson, A. F., & Ditunno, J. F. (2005). Cross-cultural differences in preference for recovery of mobility among spinal cord injury rehabilitation professionals. Spinal Cord 2006 44:9, 44(9), 567–575. https://doi.org/10.1038/sj.sc.3101876Abedi 2022
Reinhardt, J. D., Mansmann, U., Fellinghauer, B. A. G., Strobl, R., Grill, E., Von Elm, E., & Stucki, G. (2011). Functioning and disability in people living with spinal cord injury in high-and low-resourced countries: A comparative analysis of 14 countries. International Journal of Public Health, 56(3), 341–352. https://doi.org/10.1007/S00038-010-0222-8/METRICS
Ronca, E., Scheel-Sailer, A., Eriks-Hoogland, I., Brach, M., Debecker, I., & Gemperli, A. (2020). Factors influencing specialized health care utilization by individuals with spinal cord injury: a cross-sectional survey. Spinal Cord 2020 59:4, 59(4), 381–388. https://doi.org/10.1038/s41393-020-00581-6Beauregard 2012
Marchesini, N., Rubiano, A. M., Sala, F., Demetriades, A. K., & Alves, O. L. (2022). Secondary damage management of acute traumatic spinal cord injury in low and middle-income countries: A survey on a global scale (Part III). Brain & Spine, 2, 101694. https://doi.org/10.1016/J.BAS.2022.101694
Øderud, T. (2014). Surviving spinal cord injury in low income countries. African Journal of Disability, 3(2), 80. https://doi.org/10.4102/AJOD.V3I2.80
Chanbour, H., Chen, J. W., Ehtesham, S. A., Ivey, C., Pandey, A. K., Dewan, M. C., & Zuckerman, S. L. (2022). Time to Surgery in Spinal Trauma: A Meta-Analysis of the World’s Literature Comparing High-Income Countries to Low-Middle Income Countries. World Neurosurgery, 167, e268–e282. https://doi.org/10.1016/J.WNEU.2022.07.140
Evidence for “Socio-Cultural factors determining rehab LOS” is based on:
Alves, M. A., Pilusa, S., & Mashola, M. K. (2023). The prevalence and profile of spinal cord injury in public healthcare rehabilitation units in Gauteng, South Africa. Spinal Cord Series and Cases, 9(1), 15. https://doi.org/10.1038/S41394-023-00571-9
Øderud, T. (2014). Surviving spinal cord injury in low income countries. African Journal of Disability, 3(2), 80. https://doi.org/10.4102/AJOD.V3I2.80
Evidence for “Does greater rehab LOS improve outcomes?” is based on:
Abdul-Sattar, A. B. (2014). Predictors of functional outcome in patients with traumatic spinal cord injury after inpatient rehabilitation: In Saudi Arabia. NeuroRehabilitation, 35(2), 341–347. https://doi.org/10.3233/NRE-141111
Kao, Y. H., Chen, Y., Deutsch, A., Wen, H., & Tseng, T. S. (2021). Rehabilitation length of stay and functional improvement among patients with traumatic spinal cord injury. Spinal Cord 2021 60:3, 60(3), 237–244. https://doi.org/10.1038/s41393-021-00686-6
Morrison, S. A., & Stanwyck, D. J. (1999). The Effect of Shorter Lengths of Stay on Functional Outcomes of Spinal Cord Injury Rehabilitation. Topics in Spinal Cord Injury Rehabilitation, 4(4), 44–55. https://doi.org/10.1310/LG0X-1X2Y-CV2Y-RUR9
Warschausky, S., Kay, J. B., & Kewman, D. G. (2001). Hierarchical linear modeling of FIM instrument growth curve characteristics after spinal cord injury. Archives of Physical Medicine and Rehabilitation, 82(3), 329–334. https://doi.org/10.1053/apmr.2001.21510
Herzer, K. R., Chen, Y., Heinemann, A. W., & González-Fernández, M. (2016). Association Between Time-to-Rehabilitation and Outcomes Following Traumatic Spinal Cord Injury. Archives of Physical Medicine and Rehabilitation, 97(10), 1620. https://doi.org/10.1016/J.APMR.2016.05.009
Sumida, M., Fujimoto, M., Tokuhiro, A., Tominaga, T., Magara, A., & Uchida, R. (2001). Early rehabilitation effect for traumatic spinal cord injury. Archives of Physical Medicine and Rehabilitation, 82(3), 391–395. https://doi.org/10.1053/APMR.2001.19780
Cohen, J. T., Marino, R. J., Sacco, P., & Terrin, N. (2012). Association between the Functional Independence Measure following spinal cord injury and long-term outcomes. Spinal Cord 2012 50:10, 50(10), 728–733. https://doi.org/10.1038/sc.2012.50
Truchon, C., Fallah, N., Santos, A., Vachon, J., Noonan, V. K., & Cheng, C. L. (2017). Impact of Therapy on Recovery during Rehabilitation in Patients with Traumatic Spinal Cord Injury. Journal of Neurotrauma, 34(20), 2901. https://doi.org/10.1089/NEU.2016.4932
Image credits
- The Blue Marble (remastered)NASA/Apollo 17 Crew, Public Domain
- BlankMap-World. Canuckguy (talk) and many others (see File history), Public domain, via Wikimedia Commons. Modified by SCIRE.
- Graph of Median LOS in the USA ©SCIRE, CC BY-NC 4.0
- GF Strong hallway ©SCIRE, CC BY-NC 4.0








 Australia (2010 – 2011)
Australia (2010 – 2011)