Author: SCIRE Community Team | Reviewers: Lesley Houle, Rachel Nicoletti | Published: 12 June 2018 | Updated: ~
Sexual health changes are common after spinal cord injury (SCI). This page provides an overview of changes to sexual function after SCI and options for management.
Key Points
- Sexual health is an important part of health and well-being after SCI.
- People with SCI may experience changes to sexual desire, sensation, arousal, and orgasm because of the injury.
- Other changes related to the injury, such as changes to bladder and bowel control, movement, self-image, and life roles may also affect sexual health after SCI.
- People with SCI may experience changes to sexual desire, sensation, arousal, and orgasm because of the injury.
- There are a number of treatments and techniques that may be used to help improve sexual arousal and satisfaction after SCI, including medications, physical treatments, and adaptive devices.
Sexual health means being healthy and well in all parts of life related to sexuality. Sexual health is more than just being physically healthy; it also means feeling emotionally, mentally and socially well as a sexual being.
Having good sexual health means that we are able to be sexual beings and take part in sexual activities that are healthy and meaningful to each of us with our own unique needs, values, and life circumstances.
What is “sexuality”?
Sexuality describes who we are as sexual beings. It includes all the ways that we may experience and express ourselves sexually, including through aspects of our identities (such as gender identity), our physical features and functions, how we relate to others, our roles in relationships and society, and our sexual thoughts, values, beliefs and behaviours.
Sexual health after spinal cord injury
Sexual health and intimacy are important parts of living a fulfilling life and this continues to be true after SCI. In most cases, injury to the spinal cord will affect a person’s physical sexual functions in some way. Although being sexual may not be the same as it was before the injury, people with SCI continue to be sexual beings and can still have satisfying sexual and intimate lives after injury.
Watch a SCIRE video introducing sexual health after SCI.
We often think that “sex” means sexual intercourse involving penetration. However, this is only one small part of what sex is. “Sex” describes any activity that you find pleasurable and sexually satisfying. Sex means different things to different people and can include a wide range of activities, such as intimacy, kissing, touching, masturbation, oral sex, using sex toys and many other activities, as long as they feel like “sex” to you.
How is sex different after SCI?
Many people find that the beliefs they had about sex and the ways that they had sex before their injury may not be those that work best afterwards. Some things that might be different about sex after SCI may include:
- Sex might require more planning instead of being entirely “spontaneous”
- Activities that you enjoyed before your injury (such as penetrative sex) may be less important than they were before
- Body parts other than the genitals may be more pleasurable when touched (such as the lips, nipples, or areas of skin near the level of injury)
- Different sexual positions may work better after injury
- You may have a different role in your sexual relationships than you did before
- Communicating with your partner may be more important for satisfying sex than it was before
Everyone is different and will experience their sexuality differently after injury. Being open to different ideas about what sex is can be a helpful way to find what works best and is most satisfying for you after injury.
To help understand changes to sexual function after SCI, it can be helpful to understand how the sex organs work when the spinal cord is not injured.
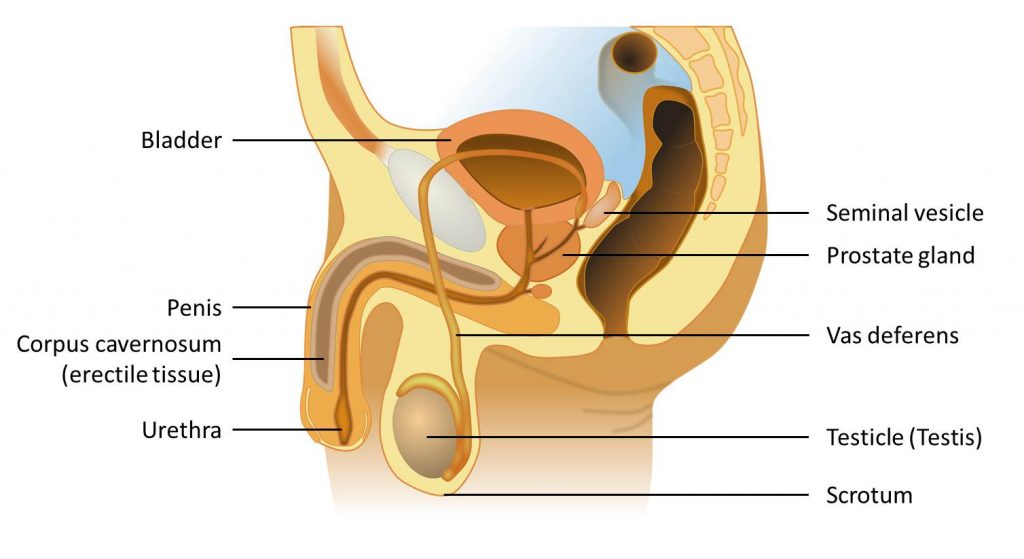
The male reproductive system
The testicles (testes) are the main male sex glands, located within a sac called the scrotum underneath the penis. The testes create sperm and hormones, which then travel through connecting tubes towards the penis. The prostate gland and seminal vesicles are glands that make fluids that mix with sperm to make semen.
The penis is a shaft that has several columns of spongy tissue. These tissues contain blood vessels that can fill up with blood to make the penis firmer (an erection). The urethra is a tube that travels through the prostate gland and penis to expel semen during ejaculation. It also passes urine from the bladder.
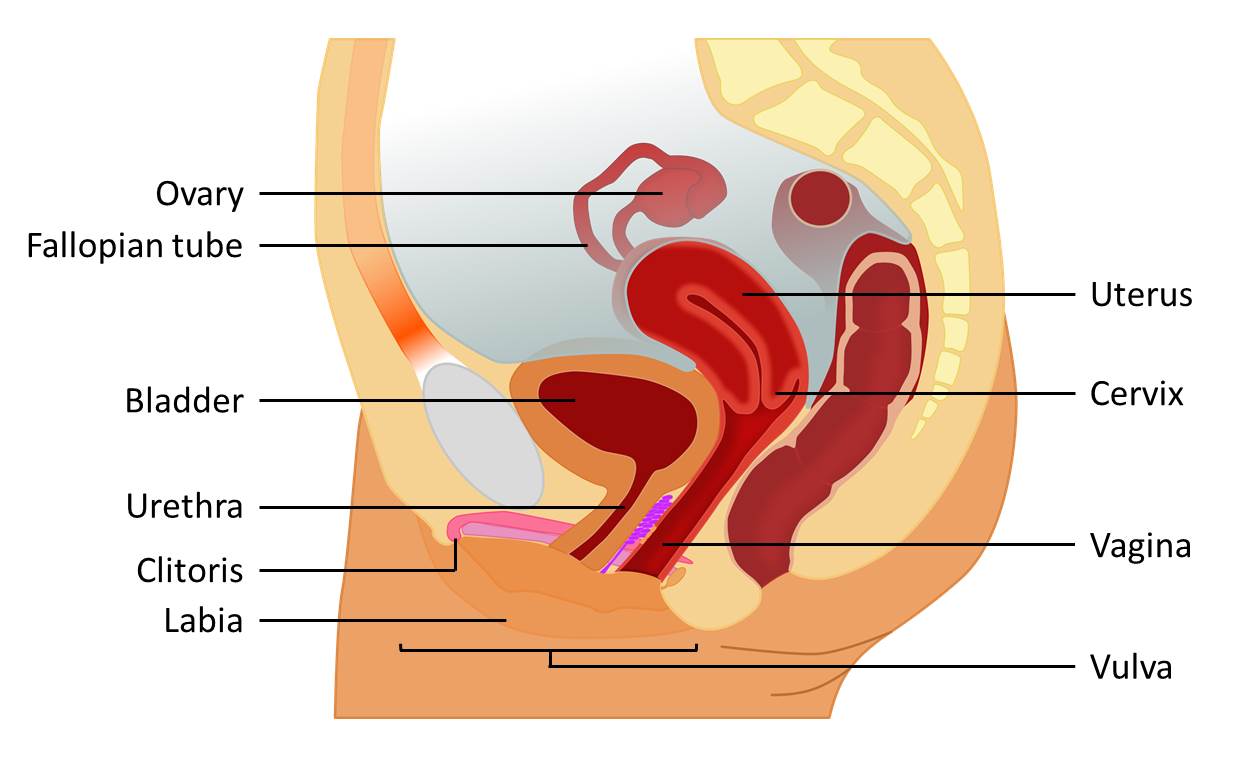
The female reproductive system
The ovaries are the main female sex glands. They are located within the abdomen and produce egg cells. The Fallopian tubes connect the ovaries to the uterus. The uterus (or womb) is where fertilized eggs develop into a fetus. It connects below to the inner part of the vagina through the cervix (the ‘neck’ of the uterus).
The vagina then extends from the cervix to the outside of the pelvis (the vulva), which is surrounded by the inner and outer vaginal lips (the labia). The opening to the urethra, where urine is expelled, is between the opening to the vagina and the clitoris.The clitoris is a small, button-like organ which is sensitive to sexual touch. It is located at the top of the inner labia above the urethra and opening to the vagina.
Sexual arousal
Sexual arousal describes how the mind and body become sexually excited and prepare the body for sex. In men, sexual arousal causes increased circulation to the penis, which fills the spongy tissues with blood and causes an erection. In women, sexual arousal involves developing lubrication in the vagina and increased circulation to the vagina and clitoris.
Sexual arousal happens in two ways
Sexual arousal happens in response to sexual thought or touch. These two ways of getting aroused have different pathways through the nervous system.
Arousal from thoughts (Psychogenic arousal)
Becoming aroused by sexual thoughts is called psychogenic arousal (‘psychogenic’ means ‘originating in the mind’). This type of arousal happens when a person sees, hears, or imagines something sexual. This causes nerve signals from the brain to travel down the spinal cord and through nerves in the thoracic and lumbar spinal cord (from T11 to L2) to the sex organs.
Arousal from touch (Reflex arousal)
When arousal happens in response to sexual touch, it is called reflex arousal. Sexual touch causes nerve signals to travel to the spinal cord and back without travelling to the brain first. This leads to automatic (reflex) arousal of the sex organs. Reflex arousal involves nerves in the sacral spinal cord (from S2 to S4).
Orgasm
 Orgasm is the peak of sexual excitement. It involves a sudden release of sexual tension caused by sexual activity, which is accompanied by rhythmic movement of muscles in the pelvis and feelings of pleasure.
Orgasm is the peak of sexual excitement. It involves a sudden release of sexual tension caused by sexual activity, which is accompanied by rhythmic movement of muscles in the pelvis and feelings of pleasure.
In men, orgasm is often accompanied by ejaculation. Ejaculation involves coordinated movements along the reproductive glands and tubes that send semen out of the penis. The muscles at the neck of the bladder also close to prevent semen from accidentally entering the bladder. In women, orgasm is accompanied by rhythmic muscle tensing in the vagina and uterus.
When the spinal cord is injured, some or all of the nerve signals that would normally allow the brain and sex organs to communicate with one another cannot get through. This can affect sexual responses in many different ways.
Changes to sensation
Most people will have some loss of feeling in the genitals and nearby skin after injury. Some people experience sensations that are less intense and others may not be able to feel their genitals at all. In some cases, pain or other unusual sensations may be felt in response to touch which was previously pleasurable.
While there is typically reduced feeling below the injury, some people notice that areas at or above the level of injury (such as the nipples, lips or ears) may be more sensitive to sexual touch after injury.
Changes to erection
Most men experience changes to their ability to get an erection and maintain it during sex. This is called erectile dysfunction. The type of erectile dysfunction that a person has depends on where the injury is on the spinal cord.
- Men with injuries at T10 and above typically lose the ability to get an erection from sexual thoughts (a psychogenic erection). However, they are usually able to get an erection through touch (a reflex erection). Sometimes reflex erections may happen in non-sexual situations (such as while inserting a catheter).
- Men with injuries from L3 to S1 may be able to have both psychogenic and reflex erections, although these responses may be poorly coordinated during sex.
- Men with injuries from S2 to S4 typically lose the ability to have reflex erections; however, they may be able to have psychogenic erections.
Listen to Cory’s experience with erections after spinal cord injury.
 Most men with SCI can get an erection in some form. However, erections are rarely the same as they were before the injury. Most men find that their erections are unreliable and can often be inadequate for penetrative sexual activity. It may also be difficult to keep the erection during sex. There are many different options for treating erectile dysfunction after SCI, which are explained below.
Most men with SCI can get an erection in some form. However, erections are rarely the same as they were before the injury. Most men find that their erections are unreliable and can often be inadequate for penetrative sexual activity. It may also be difficult to keep the erection during sex. There are many different options for treating erectile dysfunction after SCI, which are explained below.
Changes to ejaculation
 Most men with SCI also experience changes to their ability to ejaculate. They may experience an inability to ejaculate during sex, unpredictable ejaculation, or a condition called retrograde ejaculation. Retrograde ejaculation is when semen is propelled into the bladder during ejaculation because the bladder neck muscles do not close at the right time. Retrograde ejaculation is most common in people with injuries from T11 to L3. Many men with SCI require medical assistance to obtain sperm to have biological children. For some men with injuries above T6, ejaculation can also trigger autonomic dysreflexia.
Most men with SCI also experience changes to their ability to ejaculate. They may experience an inability to ejaculate during sex, unpredictable ejaculation, or a condition called retrograde ejaculation. Retrograde ejaculation is when semen is propelled into the bladder during ejaculation because the bladder neck muscles do not close at the right time. Retrograde ejaculation is most common in people with injuries from T11 to L3. Many men with SCI require medical assistance to obtain sperm to have biological children. For some men with injuries above T6, ejaculation can also trigger autonomic dysreflexia.
Changes to female arousal
In women, SCI may lead to reduced arousal responses (such as reduced vaginal lubrication). These changes depend on where the injury is on the spinal cord.
- Women with injuries at T10 and above may lose the ability to become aroused from sexual thoughts (psychogenic arousal), but may still be able to experience arousal from touch (reflex arousal).
- Women with injuries from L3 to S1 may retain both psychogenic and reflex arousal.
- Women with injuries from S2 to S4 may lose reflex arousal, but may still have psychogenic arousal.
In addition, women with SCI may also experience spasms of the vaginal muscles related to spasticity. This can cause difficulties with penetration. Treatments and techniques for improving genital arousal responses in women are outlined below.
Changes to female orgasm
Women may experience a change in their ability to orgasm following SCI. This typically involves greater difficulties in having an orgasm or an inability to have an orgasm at all. Having an orgasm may also feel different after SCI.
Changes to sexual desire
Many people experience changes to sexual desire (sometimes called libido) after an SCI. This can happen for several reasons, related to both physical changes from the injury and other life changes. For example, hormonal changes, emotional distress, and reduced sexual sensation may affect sexual desire.
Changes to self-image
Self-image describes how a person sees themselves and believes that others see them. Self-image may affect how sexually attractive a person feels and their confidence in becoming sexual after an injury. It is also an important aspect of one’s willingness to engage in social activities like dating or becoming intimate with a new partner. For some people, it takes time to adjust to the physical and life changes after an SCI and become comfortable in their own skin. Other people may find that assistance from mental health providers or peers can help them regain their self-confidence to be sexual and participate fully in intimate relationships.
Watch a SCIRE YouTube video about sexual self-esteem after SCI.
Changes to relationships
Spinal cord injury affects all aspects of life and this can cause changes to relationships as well. For example, partners may take on greater caregiving responsibilities and there may be changes in working and family roles within the partnership. While every couple is different, most people do experience some changes to their relationships which can have an impact on their sexual health.
Changes to fertility
Fertility is a male’s capacity to cause a pregnancy in a fertile female and a female’s ability to become pregnant from a fertile male. Men may have difficulty ejaculating during sex and often require medical interventions to obtain sperm. Sperm may also be lower quality following SCI because of a number of changes to the body. However, there are many medical interventions that may assist with fertility in men after SCI.
Women’s fertility is typically not affected by an SCI and they can usually become pregnant after injury. Immediately after the injury, women may experience a temporary loss in menstruation (having a period), but can still become pregnant.
This page does not discuss fertility treatments, for more information, please see SCISexualHealth.ca.
The function of the sex organs is only one part of sexual health. There are many other important considerations that may affect sexual health after SCI.
Bladder and bowel changes
Loss of bowel and bladder control is often one of the biggest concerns related to sex after SCI. People with SCI may experience bladder or bowel accidents during sex or have medical equipment such as an indwelling catheter. This can lead to anxiety or feeling self-conscious about being sexual with a partner.
Bladder and bowel changes can be managed in a number of different ways. The most important is to maintain a regular routine of bowel and bladder care to reduce the likelihood of having an accident. It may also help to:
- Discuss the topic openly with partners before sex (outside of the bedroom)
- Empty the bladder and bowel before sexual activity
- Maintain good bowel and bladder hygiene
- Prepare for potential accidents ahead of time by using waterproof sheets and having towels and wipes on hand to manage if an accident happens
Condoms can also be worn over an indwelling catheter that is folded back over the penis; please see the ‘Contraception’ page on SCISexualHealth.ca for more information.
Please see our articles on Bladder Changes After SCI and Bowel Changes After SCI for more information.
Listen to Cory describe how he manages bowel, bladder, and sex.
Hear about Cory’s initial concerns with positioning during the his recovery.
Positioning and movement for sexual activity
 Assuming positions for sex may be more challenging after an SCI because of changes in movement control and flexibility. It may also be hard to get into certain positions because of reduced flexibility caused by spasticity and joint contractures. It may help to:
Assuming positions for sex may be more challenging after an SCI because of changes in movement control and flexibility. It may also be hard to get into certain positions because of reduced flexibility caused by spasticity and joint contractures. It may help to:
- Try out different positions to find out which positions work best
- Try out different places to have sex, such as in a wheelchair
- Use assistive devices, such as bolsters, slings, and other devices to help with movement and positioning
Autonomic dysreflexia
Autonomic dysreflexia is a serious medical emergency that can affect people with SCI at T6 and above. This condition involves a sudden rise in blood pressure, which may be accompanied by heart rate changes, headaches, sweating, and other symptoms. It typically occurs in response to strong stimulation below the level of injury, even if there is no feeling in the area.
Autonomic dysreflexia may happen during sexual activity and ejaculation or as a result of sexual health treatments. If you are prone to autonomic dysreflexia, it is important to be able to recognize it when it happens and know how to treat it right away.
Please see our article on Autonomic Dysreflexia Emergency Treatments for more information.
Medications
Some medications that are used to treat other symptoms of SCI may have sexual side effects. One of the most common is Baclofen, a medication that is used to treat spasticity, which can make it more difficult to have an erection. Other medications, such as some antidepressant medications, may reduce sexual desire. If you suspect that your medications may be affecting your sexual health, speak to your health providers for more information.
Skin care
Care needs to be taken to avoid injuring the skin during sexual activity. Excessive rubbing, pressure or other forces to the skin during sexual activity can lead to pressure injuries. Care should be taken to avoid irritating or damaging the skin and any changes in skin condition should be noted and cared for as soon as possible.
Please see our article on Pressure Injuries for more information.
Erections lasting for hours (Priapism)
Priapism is an erection that lasts for more than two hours. If an erection is maintained for a long time, there will not be adequate blood circulation, which can damage the penis. Priapism is a medical emergency requiring immediate treatment from a doctor. It may happen as a side effect of treatment for erectile dysfunction, such as medications, penile rings, or injections. If you or your partner experiences an erection that lasts more than two hours, seek medical attention immediately.
Birth control and safe sex
Following an SCI, most women are still able to become pregnant, even if menstruation is temporarily stopped (which may last up to 6 months after injury). Men may also be able to cause a pregnancy after SCI. It is important that individuals who could potentially become pregnant use birth control according to their doctor’s instructions.
In addition, your risk of contracting a sexually transmitted infection (an STI) is the same after injury as it was before the injury, so it is important to engage in safe sex practices.
A sexual health assessment is typically done with a health provider such as a nurse, physician, or other health provider specializing in the care of people with SCI. Depending on your location and the services available to you, this may take place at a doctor’s office, rehabilitation centre, or specialized sexual health service.
General health and sexual health history
A review of your health and medical history, including information about your SCI, functional abilities (such as hand function) and other health conditions (including spasticity, mental health, and bladder and bowel changes), as well as your medications and other current medical treatments. Your health providers will also ask you about your current and previous sexual history and current sexual abilities and concerns.
Physical exam
Although most often not required, a sexual physical exam may include:
- Testing for movement control and muscle tone in the genitals and anus (such as the ability to squeeze the anus or control the pelvic floor muscles)
- Testing for sensation in the pelvic region
- Testing reflexes in the genital region, which may involve squeezing parts of the genitals and observing the reactions
Erectile dysfunction medications
Several medications are used to treat erectile dysfunction after SCI. The most common medications are called Phosphodiesterase 5 inhibitors (PDE5i), such as Sildenafil (Viagra), Vardenafil (Levitra), and Tadalafil (Cialis). These medications work by opening the blood vessels and increasing blood flow in the penis. This helps maintain an erection during sexual activity.
There is strong evidence that phosphodiesterase 5 inhibitors are safe and effective for treating erectile dysfunction after SCI. In general, men who are able to have reflex erections respond better to these medications.
Injectable erectile dysfunction medications
Medications that are injected through a small needle directly into the penis (called intracavernosal injections) are another common treatment. The most common medication used is Alprostadil (Caverject). The needle injects the medication into the sides of the penis to allow the blood vessels of the penis to relax and fill up with blood.
There is moderate evidence that injectable medications are effective for treating erectile dysfunction following SCI. However, there may be an increased risk of priapism, a prolonged erection that can cause damage to the penis.
Vacuum devices
Vacuum devices (sometimes called ‘pumps’) are a non-drug treatment option for getting an erection. With these devices, the penis is inserted into a cylindrical device, where a handheld pump creates a vacuum by drawing air out of the cylindrical device. This causes a change in pressure that draws blood into the penis to cause an erection.
Penile (penis) rings may help to maintain an erection from a vacuum device. A ring can be placed around the base of the penis to limit blood flow away from the penis and keeping it firm. Care should be taken when using these devices and they should not be left on for more than 30 minutes because they can cause tissue damage, especially if there is reduced sensation.
Vacuum devices are commonly used for managing erectile dysfunction after SCI, as they are non-invasive and non-drug treatment options. They may also assist with maintaining a person’s ability to have an erection over time. There is weak evidence that vacuum devices and penile rings are effective to assist with the treatment of erectile dysfunction after SCI. However, it is important that these devices are medically approved and used carefully.
Surgical implants (Penile prostheses)
Surgical implants to the penis, also known as penile prostheses, are a permanent surgical procedure that involves inserting a flexible or inflatable implant into the areas of the penis that would normally become firm during an erection. They will then remain in place, holding the penis erect. Inflatable prostheses can be inflated to fill up only when needed.
Implants are typically only used if other treatments fail because they are permanent and once implanted, other methods will not work. There is weak evidence that surgical implants may be effective for improving erectile dysfunction after SCI.
Pelvic floor exercises (Perineal muscle training)
The pelvic floor muscles (also called the perineal muscles) are a group of muscles which are located in the pelvic region. They support the internal organs from below and play a role in bladder, bowel, and sexual function. There is weak evidence that pelvic floor exercise may help improve erectile dysfunction in men with SCI who retain some ability to control these muscles.
Vibration
Vibration sensation applied to the penis from a commercial mechanical vibrator, such as the FertiCare device, may assist men with SCI in achieving ejaculation. This is sometimes called vibrostimulation, and is a frequently used technique to obtain sperm for fertility. There is weak evidence that vibration may assist with ejaculation in men with injuries above T10. These devices may also be used for sexual pleasure by some men.
Electroejaculation
 Electroejaculation is another procedure which can be used for ejaculation to collect sperm. This procedure involves the insertion of an electrical probe into the rectum, which is placed close to the prostate gland and seminal vesicles. Electrical currents are then used to stimulate the nerves to cause a reflex ejaculation. There is weak evidence that this treatment can cause ejaculation in men that are unable to ejaculate through vibrostimulation.
Electroejaculation is another procedure which can be used for ejaculation to collect sperm. This procedure involves the insertion of an electrical probe into the rectum, which is placed close to the prostate gland and seminal vesicles. Electrical currents are then used to stimulate the nerves to cause a reflex ejaculation. There is weak evidence that this treatment can cause ejaculation in men that are unable to ejaculate through vibrostimulation.
Experimental treatments for improving sensation and pleasure
There are a few experimental treatments that have shown promise in improving sexual sensation following SCI that are not currently available for treatment.
An experimental microsurgery procedure where nerves in the groin were connected to those from the penis has been shown to improve sensation of the penis in some individuals with SCI.
Sensory substitution training is an experimental technique in which stroking motions of the penis were connected to stroking of the tongue, so that the brain would be able to use the intact sense to substitute for one that is lost. In one study, this type of training improved sexual pleasure in men with SCI.
Clitoris stimulation
The clitoris is very sensitive to touch and can be stimulated manually or with a vibrator to assist with sexual arousal. There is moderate evidence that clitoral stimulation using a mechanical vibrator and stimulation with the hands both increased the sexual response of women with SCI and were both effective. There is some evidence that stimulation of other areas such as the cervix or nipples may also result in orgasm, but more research is needed.
Vacuum devices
Vacuum devices are a relatively new technology for women with SCI, in which a small cup can be placed over the clitoris and a small amount of suction is applied to increase blood to flow and arousal. There is moderate evidence that a vacuum suction device for the clitoris was effective for improving sensory stimulation and increasing lubrication in women with SCI. However, further studies are needed to confirm these results.
Medications to assist with sexual response
Sildenafil (Viagra) has been studied as a way to improve sexual responses in women with SCI with some remaining genital sensation. However, there is moderate evidence from one study that this medication was not effective for improving sexual arousal in women with SCI.
Pelvic floor exercises (Perineal muscle training)
Although it has been proposed that pelvic floor exercises may help with sexual function in women with some control in these muscles, it has not yet been studied in people with SCI.
For people of all genders, there are many other tips and techniques that may be recommended by health providers and peers to improve sexual satisfaction and participation. However, because these techniques have not been scientifically studied, we do not know how effective they are.
Assistive devices
Sexual assistive devices and sex toys, such as hands-free vibrators or positioning products like bolsters and slings, may assist with enabling different activities and enjoyment during sexual activity. For a guide to assistive sexual devices, please see the pleasureABLE Sexual Device Manual for Persons with Disabilities.
Counselling and talk therapies
Many people experience mental distress and anxiety related to changes to their sexual health. For many people, this can be one of the biggest barriers to being sexual after SCI. It may be helpful to speak to a mental health professional, sexual health clinician, or peer about your concerns and feelings.
Sexual exploration
Because the body responds differently to sex than it did before, many people find that exploration is an important way to find what feels and works best after SCI. For example, exploring other areas of arousal (such as the lips, neck, ears, or nipples) on your own or with a partner may help find new ways to experience sexual pleasure. Often, people find that the areas of skin near the level of injury are sensitive to sexual stimulation.
In addition, experimenting with different positions during sexual activity may also help during sex. Some people find that it is easier to get an erection in certain positions over others and that increasing time spent on foreplay may assist with achieving arousal. Talking to your partner about your needs and what feels best during sex can be an important part of your sexual life after SCI.
Sexual health is an important part of living well after SCI. SCI may affect many aspects of sexual function, such as sensation, arousal, and orgasm. However, people with SCI can still have fulfilling sexual lives after injury.
Several medical treatments have been shown to assist with physical arousal responses in men and women, such as medications and vacuum devices. Many other ways of enhancing sexual health may also be recommended, such as trying out different positions, activities, and sexual devices.
For a review of how we assess evidence at SCIRE Community and advice on making decisions, please see SCIRE Community Evidence.
Elliott S, McBride K (2014). Sexual and Reproductive Health Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors. Spinal Cord Injury Rehabilitation Evidence. Version 5.0. Vancouver: p 1- 84.
Available from: https://scireproject.com/evidence/rehabilitation-evidence/sexual-and-reproductive-health/
Evidence for ‘What medical treatments are available for men?’ is based on the following studies:
Erectile dysfunction medications
Derry FA, Dinsmore WW, Fraser M, Gardner BP, Glass CA, Maytom MC, et al. Efficacy and safety of oral sildenafil (viagra) in men with erectile dysfunction caused by spinal cord injury. Neurology 1998;51:1629-1633.
Giuliano F, Hultling C, El Masry WS, Smith MD, Osterloh IH, Orr M, et al. Randomized trial of sildenafil for the treatment of erectile dysfunction in spinal cord injury. Sildenafil Study Group. Ann Neurol 1999;46:15-21.
Hultling C, Giuliano F, Quirk F, Pena B, Mishra A, Smith MD. Quality of life in patients with spinal cord injury receiving Viagra (sildenafil citrate) for the treatment of erectile dysfunction. Spinal Cord 2000;38:363-370.
Del Popolo G, Li Marzi V, Mondaini N, Lombardi G. Time/duration effectiveness of sildenafil versus tadalafil in the treatment of erectile dysfunction in male spinal cord-injured patients. Spinal Cord 2004;42:643-648.
Giuliano F, Rubio-Aurioles E, Kennelly M, Montorsi F, Kim ED, Finkbeiner AE, et al. Efficacy and safety of vardenafil in men with erectile dysfunction caused by spinal cord injury. Neurology 2006;66:210-216.
Tuzgen S, Karamehmetoglu SS, Karacan I, Tanriverdi T. Use of sildenafil in the treatment of erectile dysfunction in patients with spinal cord injury. Neurosurg 2006;16:40-43.
Giuliano F, Sanchez-Ramos A, Löchner-Ernst D, Del Popolo G, Cruz N, Leriche A, et al. Efficacy and safety of tadalafil in men with erectile dysfunction following spinal cord injury. Arch Neurol. 2007;64:1584-1592.
Ergin S, Gunduz B, Ugurlu H, Sivrioglu K, Oncel S, Gok H, Erhan B, Levendoglu F, Senocak O. A placebo-controlled, multicenter, randomized, double-blind, flexible-dose, two-way crossover study to evaluate the efficacy and safety of sildenafil in men with traumatic spinal cord injury and erectile dysfunction. J Spinal Cord Med. 2008;31:522-31.
Khorrami MH, Javid A, Moshtaghi D, Nourimahdavi K, Mortazavi A, Zia HR. Sildenafil efficacy in erectile dysfunction secondary to spinal cord injury depends on the level of cord injuries. Int J Androl 2010;33:861-4.
Injectable erectile dysfunction medications (Intracavernosal injections)
Renganathan R, Suranjan B, Kurien T. Comparison of transdermal nitroglycerin and intracavernous injection of papaverine in the treatment of erectile dysfunction in patients with spinal cord lesions. Spinal Cord1997;35:99-103
Vacuum Devices and Penile rings
Moemen MN, Fahmy I, AbdelAal M, Kamel I, Mansour M, Arafa MM. Erectile dysfunction in spinal cord-injured men: Different treatment options. Int J Impotence Res 2008;20:181-187.
Denil J, Ohl DA, Smythe C. Vacuum erection device in spinal cord injured men: Patient and partner satisfaction. Arch Phys Med Rehabil 1996;77:750-753.
Chancellor MB, Rivas DA, Panzer DE, Freedman MK, Staas WE,Jr. Prospective comparison of topical minoxidil to vacuum constriction device and intracorporeal papaverine injection in treatment of erectile dysfunction due to spinal cord injury. Urology 1994;43:365-369.
Heller L, Keren O, Aloni R, Davidoff G. An open trial of vacuum penile tumescence: constriction therapy for neurological impotence. Paraplegia 1992;30:550-553.
Zasler ND, Katz PG. Synergist erection system in the management of impotence secondary to spinal cord injury. Arch Phys Med Rehabil 1989;70:712-716.
Surgical implants (Penile prosthesis)
Kim YD, Yang SO, Lee JK, Jung TY, Shim HB. Usefulness of a malleable penile prosthesis in patients with a spinal cord injury. Int J Urol 2008;15:919-923.
Zermann DH, Kutzenberger J, Sauerwein D, Schubert J, Loeffler U. Penile prosthetic surgery in neurologically impaired patients: Long-term followup. J Urol 2006;175:1041-1044.
Gross AJ, Sauerwein DH, Kutzenberger J, Ringert R-H. Penile prostheses in paraplegic men. Brit J Urol 1996;78:262-264.
Pelvic floor exercises (Perineal muscle training)
Courtois FJ, Mathieu C, Charvier KF, Leduc B, Bélanger M. Sexual rehabilitation for men with spinal cord injury: preliminary report on a behavioral strategy. Sex Disabil 2001;19:149-157.
Vibration
Beretta G, Chelo E, Zanollo A. Reproductive aspects in spinal cord injured males. Paraplegia 1989;27:113-118.
Sonksen J, Biering-Sorensen F, Kristensen JK. Ejaculation induced by penile vibratory stimulation in men with spinal cord injuries. The importance of the vibratory amplitude. Paraplegia 1994;32:651-660.
Le Chapelain L, Nguyen Van Tam P, Dehail P, Berjon JJ, Barat M, Mazaux JM, et al. Ejaculatory stimulation, quality of semen and reproductive aspects in spinal cord injured men. Spinal Cord 1998;36:132-136.
Brackett NL, Kafetsoulis A, Ibrahim E, Aballa TC, Lynne CM. Application of 2 vibrators salvages ejaculatory failures to 1 vibrator during penile vibratory stimulation in men with spinal cord injuries. J Urol 2007b;177:660-663.
Sonksen J, Fode M, Lochner-Ernst D, Ohl DA. Vibratory ejaculation in 140 spinal cord injured men and home insemination of their partners. Spinal Cord 2012;50:63-66.
Electroejaculation
Brindley GS. The fertility of men with spinal injuries. Paraplegia 1984;22:337-348.
Halstead LS, VerVoort S, Seager SW. Rectal probe electrostimulation in the treatment of anejaculatory spinal cord injured men. Paraplegia 1987;25:120-129.
Ohl DA, Bennett CJ, McCabe M, Menge AC, McGuire EJ. Predictors of success in electroejaculation of spinal cord injured men. J Urol 1989;142:1483-1486.
Lochner-Ernst D, Mandalka B, Kramer G, Stohrer M. Conservative and surgical semen retrieval in patients with spinal cord injury. Spinal Cord 1997;35:463-468.
Le Chapelain L, Nguyen Van Tam P, Dehail P, Berjon JJ, Barat M, Mazaux JM, et al. Ejaculatory stimulation, quality of semen and reproductive aspects in spinal cord injured men. Spinal Cord 1998;36:132-136.
Kolettis PN, Lambert MC, Hammond KR, Kretzer PA, Steinkampf MP, Lloyd LK. Fertility outcomes after electroejaculation in men with spinal cord injury. Fertil Steril 2002;78:429-431.
Experimental treatments for improving sensation and pleasure
Overgoor ML, de Jong TP, Cohen-Kettenis PT, Edens MA, Kon M. Increased sexual health after restored genital sensation in male patients with spina bifida or a spinal cord injury: the TOMAX procedure. J Urol 2013;189:626-632.
Borisoff JF, Elliott SL, Hocaloski S, Birch GE. The development of a sensory substitution system for the sexual rehabilitation of men with chronic spinal cord injury. J Sex Med. 2010 Nov;7(11):3647-58.
Evidence for ‘What medical treatments are available for women?’ is based on the following studies:
Clitoral stimulation
Sipski ML, Alexander CJ, Gómez-Martín O, Grossbard M, Rosen R. Effect of vibratory stimulation on sexual response in women with spinal cord injury. J Rehabil Res Devel 2005;42:609-616.
Whipple B, Richards E, Tepper M, Komisaruk BR. Sexual response in women with complete spinal cord injury. Sex Disab 1996;14:191-201.
Courtois F, Alexander M, McLain ABJ. Women’s Sexual Health and Reproductive Function After SCI.Top Spinal Cord Inj Rehabil. 2017 Winter;23(1):20-30.
Vacuum devices
Alexander M, Bashir K, Alexander C, Marson L, Rosen R. Randomized Trial of Clitoral Vacuum Suction Versus Vibratory Stimulation in Neurogenic Female Orgasmic Dysfunction. Arch Phys Med Rehabil. 2018 Feb;99(2):299-305.
Medications to assist with sexual response
Alexander MS, Rosen RC, Steinberg S, Symonds T, Haughie S, Hultling C. Sildenafil in women with sexual arousal disorder following spinal cord injury. Spinal Cord 2011;49:273-279.
Sipski ML, Rosen RC, Alexander CJ, Hamer RM. Sildenafil effects on sexual and cardiovascular responses in women with spinal cord injury. Urology 2000;55:812-815.
Pelvic floor exercises (Perineal muscle training)
Courtois F, Alexander M, McLain ABJ. Women’s Sexual Health and Reproductive Function After SCI.Top Spinal Cord Inj Rehabil. 2017 Winter;23(1):20-30.
Other references
Alexander CJ, Sipski ML, Findley TW. Sexual activities, desire, and satisfaction in males pre- and post-spinal cord injury. Arch Sex Behav 1993;22:217-228.
Alexander M, Courtois F, Elliott S, Tepper M. Improving sexual satisfaction in persons with spinal cord injuries: Collective wisdom. Top Spinal Cord Inj Rehabil. 2017;23(1):57-70.
Alexander MS, Rosen RC, Steinberg S, Symonds T, Haughie S, Hultling C. Sildenafil in women with sexual arousal disorder following spinal cord injury. Spinal Cord 2011;49:273-279.
Anderson KD. Targeting recovery: Priorities of the spinal cord-injured population. J Neurotrauma 2004;21:1371-1383.
Axel SJ. Spinal cord injured women’s concerns: Menstruation and pregnancy. Rehabil Nurs 1982;7:10-15.
Baker ER, Cardenas DD, Benedetti TJ. Risks associated with pregnancy in spinal cord-injured women. Obstet Gynecol 1992;80:425-428.
Brackett NL, Lynne CM, Aballa TC, Ferrell SM. Sperm motility from the vas deferens of spinal cord injured men is higher than from the ejaculate. J Urol 2000;164:712-715.
Denys P, Mane M, Azouvi P, Chartier-Kaster E, Thiebault J-B, Bussel B. Side effects of chronic baclofen on erection and ejaculation in patients with spinal cord lesions. Arch Phys Med Rehabil 1998;79;494-496.
Dunzendorfer, U. (ed.) Sildenafil. Basel: Springer Science & Business Media; 2004.
Jackson AB, Wadley V. A multicenter study of women’s self-reported reproductive health after spinal cord injury. Arch Phys Med Rehabil 1999;80:1420-1428.
Jones ML, Leslie DP, Bilsky G, Bowman B. Effects of intrathecal baclofen on perceived sexual functioning in men with spinal cord injury. J Spinal Cord Med 2008;31:97-102.
Lombardi G, Mondaini N, Macchiarella A, Del Popolo G. Female sexual dysfunction and hormonal status in spinal cord injured patients. J Androl 2007; 28(5):722-76.
Ohl DA, Bennett CJ, McCabe M, Menge AC, McGuire EJ. Predictors of success in electroejaculation of spinal cord injured men. J Urol 1989;142:1483-1486.
Rutkowski SB, Middleton JW, Truman G, Hagen DL, Ryan JP. The influence of bladder management on fertility in spinal cord injured males. Paraplegia 1995;33:263-266.
Sexual health and its linkages to reproductive health: an operational approach. Geneva: World Health Organization; 2017. Licence: CC BY-NC-SA 3.0 IGO.
Skrowonski E, Hartman K. Obstetric management following tramautic tetraplegia: case series and literature review. Aust NZJ Obstet Gynaecol 2008;45:485-491.
Sramkova T, Skrivanova K, Dolan I, Zamecnik L, Sramkova K, Kriz J, Muzik V, Fajtova R. Women’s Sex Life After Spinal Cord Injury. Sex Med. 2017 Dec;5(4):e255-e259.
Image credits:
- BeachWheelchairGPEIBLS_6945x_EDT ©Government of Prince Edward Island, CC BY-NC-ND 2.0
- Love Life ©amslerPIX, CC BY-NC 2.0
- Modified from: Male anatomy blank ©Tsaitgaist, CC-BY-SA-3.0 and Male anatomy ©alt.sex FAQalt, GFDL
- Modified from: Female anatomy with g-spot ©Tsaitgaist, CC BY-SA 3.0 or GFDL
- Closeness ©Mark S Waterhouse, CC BY 3.0 US
- Fireworks ©Alex Muravev, CC BY 3.0 US
- Impotent ©Stephen Plaster, CC BY 3.0 US
- Sperm ©Alejandro Capellan, CC BY 3.0 US
- Image by SCIRE Community Team
- 000068750037 ©Alagich Katya, CC BY 2.0
- Make love ©matias porta lezcano, CC BY 3.0 US
- Assorted Medications ©NIAID, CC BY 2.0
- Not 100% Effective © Nate Grigg, CC BY 2.0
- Image by SCIRE Community Team
- Viagra ©Tim Reckmann, CC BY 2.0
- Air based penis pump ©Bjoernnielsen, CC BY-SA 4.0
- Prótesis de pene inflable ©Eduardo García Cruz, CC BY 2.0
- Sperm ©Hare Krishna, CC BY 3.0 US
- Penis-shaped vibrator ©Mekitin, CC0 1.0
- Image by SCIRE Community Team