Author: SCIRE Community Team | Reviewer: Darryl Caves | Published: 17 January 2018 | Updated: ~
Standing with supportive equipment is a therapy option after spinal cord injury (SCI). This page outlines basic information about the use of supported standing after SCI.
Key Points
- Passive standing using supportive equipment is a therapy option for people who do not stand as part of their everyday mobility.
- Passive standing involves using equipment such as standing frames, tilt tables, orthoses or standing wheelchairs to support an upright position for a period of time.
- Standing involves a change in posture that challenges the circulatory system, loads the legs, and provides different sensory stimulation.
- Research evidence suggests that standing may improve blood pressure control and spasticity management. There is conflicting evidence about whether passive standing helps with bone density or bowel and bladder health.
- Further research is needed to better understand the benefits of standing after SCI and how long standing should be done for to achieve those benefits.
Standing is an important part of functional movement in humans. Standing is needed for walking, and also provides a challenge to the circulatory system, bones, and muscles in ways that cannot be achieved in sitting or lying.
Passive standing (standing with support instead of by muscle activation) may have treatment benefits after SCI, even when the recovery of walking and standing abilities is unlikely. Standing may have benefits in treating health conditions associated with SCI, such as conditions involving the musculoskeletal, circulatory, breathing, bowel and bladder systems. It remains a key treatment tool used in rehabilitation.
Supported standing involves the use of special equipment to support an upright posture. The type of equipment used depends on the person’s unique characteristics and abilities (such as the amount of muscle control in the arms, legs and trunk), the equipment that is available, and other medical concerns like joint contractures, spasticity and osteoporosis. Equipment used for standing may include a wide range of different devices such as:
Tilt tables
Tilt tables are flat surfaces that can be tilted from a horizontal position into a vertical standing position. The person is strapped securely to the table while in a horizontal lying position and the table can be tilted vertically. Tilt tables are typically the first devices that are used to work towards standing because the table can be gradually increased by degrees. This is often needed because it may take some time to tolerate being upright and maintaining a safe blood pressure. It is also a good device to test a person’s physical tolerance and safety for standing.
Standing frames
Standing frames are simple frames that have padding at the joints to support a standing position. There are many different types of standing frames. The frame needs to be fitted to the person’s unique physical abilities and body type and minimize areas of excess pressure.
Standing wheelchairs
Standing wheelchairs are wheelchairs that can extend from a sitting position into standing. There are many different types of standing wheelchairs, from manual devices to motorized systems. However, standing wheelchairs are expensive and not commonly available.
Body weight-supported treadmill training
Suspension body weight support systems involve a harness system that is suspended from above to support a percentage of body weight while standing. These systems are typically used while walking on a treadmill (body weight-supported treadmill training) or sometimes while walking over ground. This type of system is usually used for people with incomplete injuries that may work towards standing or stepping independently.
See our article on Body Weight Supported Treadmill Training.
Robotic exoskeletons
Robotic exoskeletons are a relatively new and emerging technology that is typically used for walking and walking training, but may also have benefits related to standing. However, this equipment is costly and not available in most settings.
Walkers, crutches or canes may be used by people with incomplete SCI and good strength in the arms who need only minimal support in standing.
Orthoses
Orthoses and braces may be used to brace the hip, knee and/or ankle joints to keep them from bending. This can help to support the person in an upright standing posture with training and rehabilitation. Orthoses and braces are typically custom-made and usually used by people with paraplegia who have good upper body strength and hip flexibility. Orthoses and braces used for standing may include:
- Knee Ankle Foot Orthoses (KAFOs) provide support at the knee, ankle and foot.
- Reciprocating Gait Orthoses (RGOs) are more complex orthoses that are made of a left and right KAFO that are linked together with a rigid brace at the pelvis or abdomen. The brace has hip joints that are built with an alternating stepping mechanism. When one leg is extended, the other flexes forward, providing assistance for stepping. Although normally used for walking, reciprocating gait orthoses can also be used to help support a standing position.
Functional electrical stimulation
Functional electrical stimulation (FES) involves the use of electrical stimulation to activate muscles that are weak or paralyzed after an SCI during a purposeful activity. FES over the trunk or leg muscles may be used while standing with equipment for added benefits.
See our article on Functional Electrical Stimulation (FES) for more information.
Standing equipment may be expensive and sometimes requires repeated visits to healthcare facilities, which can sometimes be a barrier to regular standing. It is important for the individual to work with their health providers to find appropriate equipment that is safe and suitable.
Once appropriate equipment and strategies for standing are selected with assistance from a health provider, standing is gradually introduced over time. The amount of time spent standing, the amount of load that is taken through the legs, and the final standing position will be adjusted until a suitable standing position can be maintained. During these first several sessions, health providers will monitor for any adverse effects related to the treatment.
Current research findings are unable to tell us how long or how often standing should be done to have benefits. Studies have used standing for 20 to 60 minutes, three to four times per week to study the effects of this treatment. It will be different for everyone. The standing prescription will be based on the person’s unique situation.
Depending on the treatment goals, standing may also involve:
- Adding extra weight while standing
- Using standing together with functional electrical stimulation (FES) to activate the muscles of the legs and/or trunk
- Weight-shifting, balance or stepping activities
Supported standing is considered to be a relatively safe treatment for use after SCI. However, there are some situations in which standing may not be appropriate and some possible risks. This is not a complete list; please consult a health provider for further safety information.
Standing should not be used in the following situations:
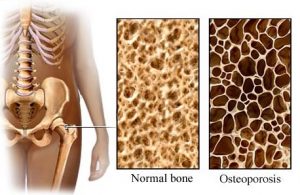
- By people with recent broken bones (fractures) or a high risk of fractures (such as people with severe osteoporosis)
- Where the standing equipment places excess pressure on areas where there are injuries, sores, and wounds; or areas of skin prone to pressure injuries
- By individuals whose limbs cannot be brought into a good standing position due to other conditions like joint contractures, spasticity, or heterotopic ossification
- By people with medical conditions where heart rate or blood pressure are uncontrolled, such as those who are unable to stay upright without a major drop in blood pressure (severe orthostatic hypotension)
- By people with muscle or joint injuries or other conditions that may be worsened by standing
Risks of standing may include:
- Pressure injuries if the position and equipment used for standing creates too much pressure or shear while standing – it is essential that the equipment used for standing is appropriately fitted to prevent skin damage
- Blood pooling in the legs may lead to feelings of light-headedness, dizziness or fainting (orthostatic hypotension)
- Broken bones (fractures) are possible in weight-bearing positions in people with osteoporosis
- Increased spasticity or autonomic dysreflexia in some people
- Pain in the standing position
For more information on these topics, see our articles on Pressure Injuries, Orthrostatic Hypotension, Osteoporosis, Spasticity, and Autonomic Dysreflexia
If using electrical stimulation, the safety precautions and risks associated with use of functional electrical stimulation (FES) also apply.
Bone health
It is not clear if standing helps to maintain or increase bone density in the legs after SCI. Current research evidence is inconclusive and further studies are needed.
Blood pressure and circulation
Another proposed use of standing after SCI is to help with blood pressure control. One study provides weak evidence that standing with a harness and assistance from health providers helps to increase resting blood pressure and reduce drops in blood pressure when standing (orthostatic hypotension) in people with cervical SCI.
Spasticity
There is weak evidence that standing may help to reduce spasticity short term in people with SCI. There are also surveys that report that many people with SCI report that regular standing helped to reduce their spasticity.
Bowel problems
There is not enough evidence to determine whether standing can also improve bowel function. Further research in this area is needed.
Supported standing serves as a therapy option for people such as individuals with SCI as they do not normally stand as part of their everyday mobility. This therapy involves equipment such as standing frames, tilt tables, orthoses, or standing wheelchairs to support an upright position for a designated period of time. While there is research supporting the benefits of supported standing, conflicting evidence is still apparent. Further research is needed to better understand the benefits of supported standing after SCI.
For a review of how we assess evidence at SCIRE Community and advice on making decisions, please see SCIRE Community Evidence.
Parts of this page have been adapted from the SCIRE Professional “Bone Health”, “Orthostatic Hypotension”, “Spasticity”, and “Bowel Dysfunction and Management” Modules:
Craven C, Lynch CL, Eng JJ (2014). Bone Health Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors. Spinal Cord Injury Rehabilitation Evidence. Version 5.0. Vancouver: p 1- 37.
Available from: https://scireproject.com/evidence/bone-health/
Krassioukov A, Wecht JM, Teasell RW, Eng JJ (2014). Orthostatic Hypotension Following Spinal Cord Injury. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors. Spinal Cord Injury Rehabilitation Evidence. Version 5.0. Vancouver: p. 1-26.
Available from: https://scireproject.com/evidence/orthostatic-hypotension/
Hsieh JTC, Connolly SJ, McIntyre A, Townson AF, Short C, Mills P, Vu V, Benton B, Wolfe DL (2016). Spasticity Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Curt A, Mehta S, Sakakibara BM, editors. Spinal Cord Injury Rehabilitation Evidence. Version 6.0.
Available from: https://scireproject.com/evidence/spasticity/
Coggrave M, Mills P, Willms R, Eng JJ, (2014). Bowel Dysfunction and Management Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors. Spinal Cord Injury Rehabilitation Evidence. Version 5.0. Vancouver: p 1- 48.
Available from: https://scireproject.com/evidence/bowel-dysfunction-and-management/
Evidence for “Does standing work for treating the symptoms of SCI?” is based on the following studies:
Bone health
[1] Dudley-Javoroski S, Saha PK, Liang G, Li C, Gao Z, and Shields RK. High dose compressive loads attenuate bone mineral loss in humans with spinal cord injury. Osteoporos Int 2012; 23:2335-2346.
[2] Goktepe A, Tugco I, Alaca, R, Gunduz S, Nikent M. Does standing protect bone density in patients with chronic spinal cord injury? JSCM 2008;31:197-201.
[3] Needham-Shropshire BM, Broton JG, Klose KJ, Lebwohl N, Guest RS, Jacobs PL. Evaluation of a training program for persons with SCI paraplegia using the Parastep 1 ambulation system: part 3. Lack of effect on bone mineral density. Arch Phys Med Rehabil 1997;78:799-803.
[4] Kunkel CF, Scremin AM, Eisenberg B, Garcia JF, Roberts S, Martinez S. Effect of “standing” on spasticity, contracture, and osteoporosis in paralyzed males. Arch Phys Med Rehabil 1993;74:73-78.
[5] Kaplan PE, Roden W, Gilbert E, Richards L, Goldschmidt JW. Reduction of hypercalciuria in tetraplegia after weight-bearing and strengthening exercises. Paraplegia 1981;19:289-293.
[6] Ben M, Harvey L, Denis S, et al. Does 12 weeks of regular standing prevent loss of ankle mobility and bone mineral density in people with recent spinal cord injuries? Aust J Physiother. 2005;51:251-256.
[7] de Bruin ED, Frey-Rindova P, Herzog RE, Dietz V, Dambacher MA, Stussi E. Changes of tibia bone properties after spinal cord injury: effects of early intervention. Arch Phys Med Rehabil 1999;80:214-220.
[8] Dudley-Javoroski S, and Shields RK. Active-resisted stance modulates regional bone mineral density in humans with spinal cord injury. Journal of Spinal Cord Medicine 2013; 36: 191-199.
Blood Pressure and Circulation
[1] Harkema SJ, Ferreira CK, van den Brand RJ, Krassioukov AV. Improvements in orthostatic instability with stand locomotor training in individuals with spinal cord injury. J Neurotrauma 2008;25:1467-1475.
Spasticity
[1] Odeen I, Knutsson E. Evaluation of the effects of muscle stretch and weight load in patients with spastic paraplegia. Scand J Rehabil Med 1981;13:117-21.
[2] Bohannon R. Tilt table standing for reducing spasticity after spinal cord injury. Arch Phys Med Rehabil 1993;74:1121-2.
[3] Kunkel C, Scremin A, Eisenberg B, Garcia J, Roberts S, Martinez S. Effect of “standing” on spasticity, contracture, and osteoporosis in paralyzed males. Arch Phys Med Rehabil 1993;74:73-8.
[4] Dunn R, Walter J, Lucero Y, Weaver F, Langbein E, Fehr L, et al. Follow-up assessment of standing mobility device users. Assist Technol 1998;10:84-93.
[5] Eng JJ, Levins S, Townson A, Mah-Jones D, Bremner J, Huston G. Use of prolonged standing for individuals with spinal cord injuries. Phys Ther 2001;81:1392-9.
[6] Shields R & Dudley-Javoroski S. Monitoring standing wheelchair use after spinal cord injury: a case report. Disabil Rehabil 2005;27:142-6.
Bowel problems
[1] Hoenig H, Murphy T, Galbraith J, Zolkewitz M. Case study to evaluate a standing table for managing constipation. SCI Nursing 2001;18:74-7.
Other references
Dunn RB, Walter JS, Lucero Y, Weaver F, Langbein E, Fehr L, Johnson P, Riedy L. Follow-up assessment of standing mobility device users. Assist Technol. 1998;10(2):84-93.
Glickman LB, Geigle PR, Paleg GS. A systematic review of supported standing programs. J Pediatr Rehabil Med. 2010; 3(3),197-213.
Sadeghi M, McLvor J, Finlayson H, Sawatzky B. Static standing, dynamic standing and spasticity in individuals with spinal cord injury. Spinal Cord 2016;54:376-82.
Spinal Cord Injury Centre Physiotherapy Lead Clinicians. Clinical guideline for standing adults following spinal cord injury. 2019 Apr. Available from: https://scireproject.com/wp-content/uploads/2023/01/SCI-Standing-Clinical-Guidelines-Report-2019.pdf
Image credits
- 58/365 ©John Lustig, CC BY 2.0
- Image ©SCIRE
- Standing frame ©Memasa, CC BY-SA 3.0
- Functional Electrical Stimulation Therapy for walking ©MilosRPopovic, CC BY-SA 4.0
- Image ©SCIRE
- Modified from: oesteoporosis_eng ©go elsewhere…, CC BY-NC 2.0
- KRT LIFE HEALTH-BLOOD-PRESSURE PG ©Fort George G. Meade Public Affairs Office, CC BY 2.0