Author: Kelsey Zhao | Reviewer: Michael Berger, Christopher Doherty | Published: 23 January 2024 | Updated: ~
Key Points
- Nerve transfer surgeries in SCI aim to restore some movement to the arm or hand by connecting a healthy nerve to the nerve of a paralyzed muscle.
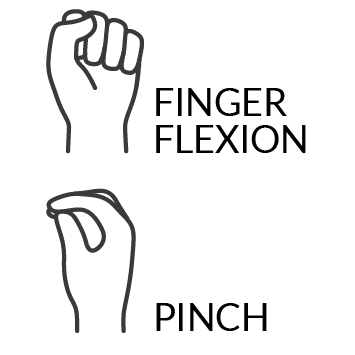
- This surgery is most commonly used to improve finger and thumb movement for people with cervical SCIs.
- Depending on the type of injury, some nerve transfers are time-sensitive and must be done within 6 months, while others can be done years after the injury.
- Experts recommend at least two years of physical and occupational therapy after a nerve transfer to rehabilitate the muscles.
- Although the current evidence is limited, nerve transfers are a promising treatment for improving an individual’s independence and quality of life.
Spinal cord injury (SCI) disrupts the nerve pathways that send signals between the brain and muscles. This disruption can lead to loss of muscle strength and movement.
Nerve transfer surgery aims to restore some movement to a paralyzed muscle by connecting a nearby functional nerve from above the SCI to the non-functional nerve of the paralyzed muscle. The paralyzed muscle and its non-functional nerve are called the recipient. The functional nerve transferred to the recipient is called the donor. The donor nerve used is expendable (i.e. removing the nerve does not cause any significant loss of movement) or taken from an area where there is more than one muscle that performs the same movement. Over time and with rehabilitation, the healthy cells of the functional nerve will use the non-functional nerve as a scaffold to grow towards the paralyzed muscle. This creates a new pathway for signals to travel between the brain and the muscle.
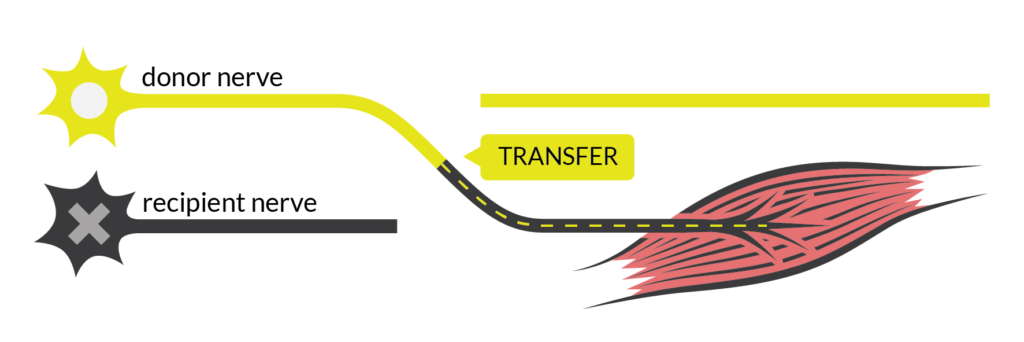
Nerve transfers involve the transfer of a functional donor nerve to a non-functional recipient nerve to create a new signal pathway to a paralyzed muscle.1
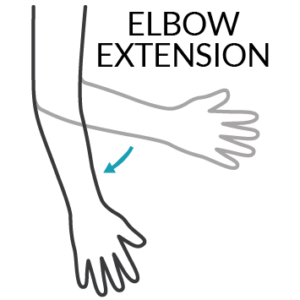
Since the success of nerve transfer techniques were demonstrated in other nerve injuries, like brachial plexus injury, they are now being applied to SCI. Nerve transfers are usually done after a cervical SCI to regain movement in the upper limbs. Some functions commonly targeted in nerve transfers include elbow extension, wrist extension, finger extension, finger flexion, and finger extension.
Table 1: Common nerve transfer surgeries and the donor/recipient nerves that can be used to restore each muscle function.2-5
Function |
Donor |
Recipient |
|
|
Teres minor nerve | Triceps nerve |
| Teres minor and motor portion of posterior division of axillary nerve | Triceps nerve | |
| Motor portion of posterior division of axillary nerve | Triceps nerve | |
| Fascicle of anterior division of axillary nerve | Triceps nerve | |
|
|
Supinator nerve | ECRB (Extensor carpi radialis brevis) nerve |
|
|
Supinator nerve | PIN (Posterior interosseous nerve) |
|
|
Brachialis nerve | AIN (Anterior interosseous nerve) |
| ECRB nerve | AIN | |
| Supinator nerve | AIN | |
| Fascicle to pronator teres nerve | FDS (Flexor digitorum superficialis) nerve |
Although wrist extension (bend wrist up) and wrist flexion (bend wrist down) can be targeted with nerve transfer, wrist movement is often reconstructed with tendon transfers instead. Learn more about tendon transfers in the How do nerve transfers compare to tendon transfers? section below.
Improved movement in the arms and hands can increase an individual’s independence and confidence in many areas of life, including daily activities, mobility, and socializing.
This YouTube video explains the basics of nerve transfer and tendon transfer surgeries, and the differences between the two. This video was created by Neramy Ganesan, a graduate of the University of Toronto MSc Biomedical Communications Program, with the help of content expert Dr. Jana Dengler at Sunnybrook Health Sciences Centre. Please see the end credits in the video for more details.6
Level of injury
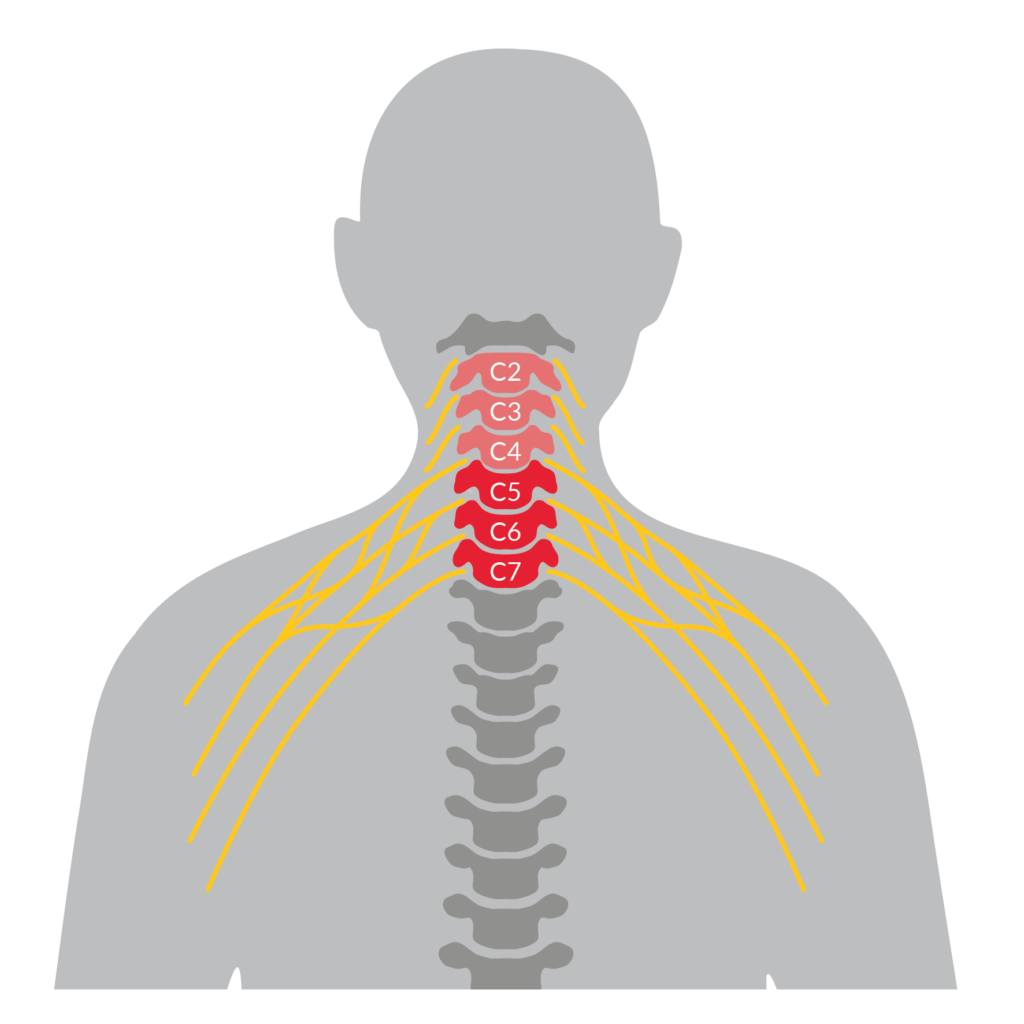
Nerve transfers are usually done on cervical spinal cord injuries levels C5-C7.7
Nerve transfers are typically used to improve arm and hand function for people with higher level spinal cord injuries between C5 and C7. Keep in mind that since nerve transfers are a surgical treatment targeting movement, suitability is based on the level of muscle function. For example, someone with an incomplete SCI whose overall level of injury is C3, but C5 for muscle function, is more likely to be eligible for nerve transfer than someone whose level of injury is C3 for both sensory and muscle function.
Recent studies have shown some success with nerve transfers in injury levels up to C2, but more recovery of movement is associated with lower levels of cervical injury. Consideration for nerve transfer surgery in levels above C5 is made on a case-by-case basis, depending on what donor nerves are available.
Refer to our articles on Spinal Cord Anatomy and Spinal Cord Injury Basics for more information!
Nerve function and time since injury
Two types of neurons make up the nerve pathways that send movement signals to and from the brain and the muscles.
- Upper motor neurons connect the brain to the spinal cord.
- Lower motor neurons connect the spinal cord to muscle.
The ideal timing for how long after SCI a nerve transfer can be performed depends on whether the upper or the lower motor neurons in the nerve pathway of the paralyzed muscle are damaged. Which motor neurons are damaged is different for nerve pathways that exit the spinal cord (out to the muscle) at the level of injury and nerve pathways that exit below the level of injury.
Motor neurons at the level of injury
Often, both lower and upper motor neurons are damaged at and around the level of injury. The loss of a functional nerve in the muscle causes it to degenerate and atrophy (waste away). The muscle atrophy becomes irreversible 12-18 months after the injury, at which point a nerve transfer would be unable to restore any movement to the muscle. In this case, a nerve transfer should be done around 6 months after SCI, so that the donor nerve cells can reach the paralyzed muscle before the degeneration becomes irreversible.
Motor neurons below the level of injury
Below the SCI, often the upper motor neuron is damaged but the lower motor neuron that connects the muscle to the spinal cord is still intact. The nerve in the muscle is still functional, but you cannot control it because the connection to the brain is disrupted. The muscle is maintained by the activity of the functional nerve’s connection to the spinal cord so degeneration occurs more slowly. In this case, a nerve transfer may be possible for years after the injury, but patient selection is more specific and surgery outcomes are less predictable.
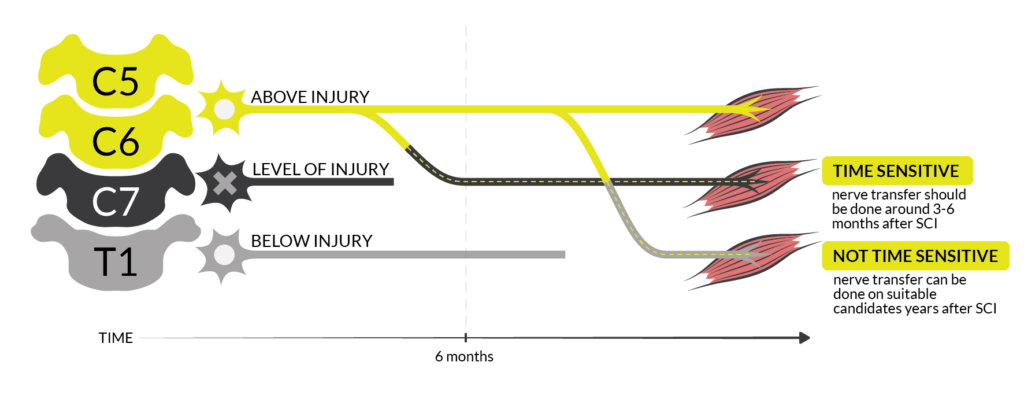
The timing of nerve transfer after spinal cord injury depends on whether the nerve that connects to the muscle is damaged. If it is, the muscle will degenerate more quickly, and nerve transfer should be considered earlier.8
Other considerations
Some other factors to consider when deciding whether to do a nerve transfer surgery include:
- Caregiver availability for the period after surgery when you will need extra support with daily activities.
- Emotional/psychological supports.
- Personal goals for function or recovery. Speak to your health care provider to determine whether a nerve transfer is suitable for your goals.
- Transportation to the clinic or hospital for diagnostic testing, the surgery, and rehabilitation.
- Other injuries in the arms, hands, or wrists or other neurological conditions that could increase the risk of complications in surgery and/or rehabilitation.
- General considerations for surgery (e.g., open wounds, infection, high blood pressure, diabetes, heart and lung problems, extreme obesity, mental health).
- SCI considerations for surgery (e.g., pressure sores, joint stiffness, spasticity, autonomic dysreflexia).
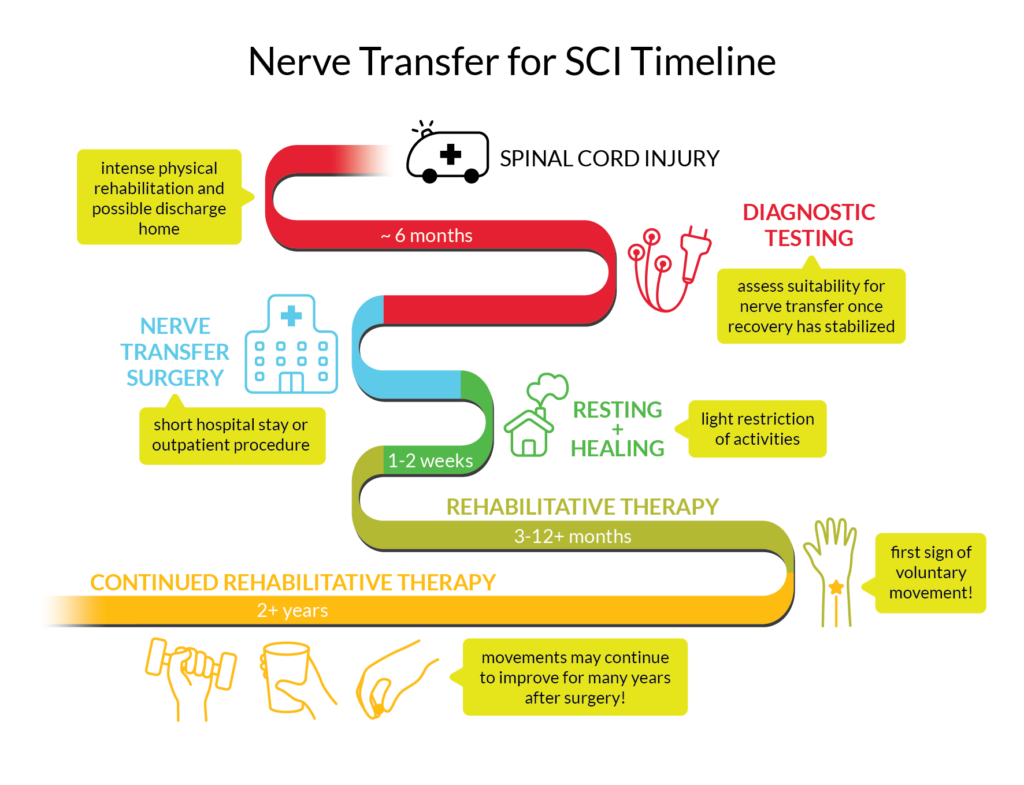
A timeline of the process for time-sensitive nerve transfer for a cervical spinal cord injury where the lower motor neuron of the recipient muscle is injured.9
Before surgery
The irreversible degeneration of muscle needs to be balanced with giving the nerves time to heal from the SCI. However, after 6 months, the probability of nerves recovering on their own becomes much less likely. The timing and type of nerve transfer ultimately depend on the nature of the SCI and what nerves are affected by the injury.
Suitability for nerve transfer is determined through physical examinations of muscle function and electrodiagnostic testing. Physical examination looks at the stability, strength and range of motion (how far you can move a limb in different directions) of the muscles and joints.
Electrodiagnostic tests may include the following:
Electromyography (EMG)
Electromyography measures the activity of nerves in a muscle by inserting a small needle electrode (similar to acupuncture) into the muscle tissue.
Nerve Conduction Studies
Nerve conduction studies measure the strength and speed of the signals travelling through a nerve by sending electrical pulses from a device and measuring with electrodes.
The combination of results from electrodiagnostic tests and physical exams is used to identify nerves and muscles that are functional /non-functional and figure out which muscles and nerves should be used in the nerve transfer. The tests could also determine if there is a possibility that the muscles will recover on their own and not require surgery. The results can also help to estimate what your timeline for surgery might look like.
During surgery
General anesthesia is given before the surgery. Electrical stimulation can be used to make sure the right nerves are being cut. Once the identities of the nerves are confirmed, the healthy nerve is cut and stitched to the cut end of the damaged nerve.
After surgery
In the 1-2 weeks following surgery, activity will be restricted to allow your skin and nerves to heal. After the period of rest, you can return to regular activity and begin intensive physical/occupational therapy. Even though the nerve transfer reconnects the pathway from the paralyzed muscle to the brain/spinal cord, it is not like plugging two extension cords together and having the current run through instantly. Attaching the two nerves allows the recipient nerve to act as a scaffold for the cells of the donor nerve to grow through, towards the muscle. This process can take months or years depending on the distance to the muscle because nerve cells grow at approximately 1mm per day.
Rehabilitation
After healing, you undergo intense physical therapy and occupational therapy to recover and maintain the muscle’s range of motion and strength, and to relearn how to move the muscle with the new nerve pathway. This rehabilitation process will teach you how to use the muscle properly and strengthen the muscles with a variety of exercises. Experts recommend that consistent therapy be continued for a minimum of 2 years.
Research on nerve transfers has found that people can continue to experience improvements in function as far as 4 years after the surgery with physical and occupational therapy.
Some activities to rehabilitate muscle function after nerve transfers include:
Early stage (no movement in the muscle yet)
-
- Education: Understanding which muscles and nerves are involved in the nerve transfer and how the surgery has changed the way they work.
- Range of motion: Exercises to maintain how far the muscle can move in different directions. Splints may be used to manage range of motion and spasticity.
- Donor activation: Physically moving the donor muscle to activate the donor nerve.
- Visualization: Moving the donor muscle and visualizing moving the recipient muscle. This is an important exercise in early rehabilitation.
- Donor co-contraction: Moving the donor muscle and having someone else move the recipient muscle at the same time to strengthen the connection between the nerve and the new movement.
After first sign of muscle movement
-
- Donor co-contraction: Moving the donor muscle and recipient muscle at the same time to strengthen the nerve connection.
- Moving only the recipient muscle.
- Exercises based on real life activities.
- Doing exercises in water or with assistive devices like slings and prostheses can make movements easier by reducing the effect of gravity.
- Biofeedback or neuromuscular electrical stimulation (NMES) may be used to promote movement.
Strength and endurance
-
- Gradually increased resistance of exercises (adding weights).
- Gradually increased repetitions of exercises.
- Incorporating function of muscle into everyday life.
Visualization for muscle rehabilitationVisualization (also known as mental practice, mental imagery, and motor imagery) is a technique where you consciously and repeatedly imagine performing a movement without actually moving your body. One theory for why this technique works is that visualizing a movement activates areas of the brain that overlap significantly with the areas that activate when physically doing the movement. Studies of people without SCI and athletes who use visualization when learning new skills have shown that physical movement performance improves. In rehabilitation for neurological disorders, including SCI, evidence from high-quality studies has shown that visualization used in combination with physical therapy has positive effects on muscle movement. |
Tendons are rope-like bands that connect your muscles to your bones. In a tendon transfer, the tendon of a healthy muscle with functional nerves is cut and attached to the tendon of a paralyzed muscle. This transfer allows the working muscle to take over the movement of the paralyzed muscle. This is another way that movement can be restored in the arm or hand for someone with tetraplegia.

Tendon transfers involve using a working muscle to power a paralyzed muscle movement by transferring the tendon of the working muscle to the paralyzed muscle.10
Nerve transfers and tendon transfers can also be used in combination to restore movement. Patients in one study who underwent both nerve transfer and tendon transfer reported no preference because each was beneficial in a different way. Hands with nerve transfers resulted in more natural and dexterous movement, and hands with tendon transfers felt stronger. Each has characteristics that make the procedure more or less suitable for an individual depending on their injury, timing, and recovery goals.
Table 2: Comparison of nerve transfers and tendon transfers
Nerve Transfer |
Tendon Transfer |
|
What kind of movement is improved? |
More precise, controlled movements that do not require as much strength. | Stronger movements that do not require as much precise coordination. |
What kind of activities could this surgery help with? |
• Using devices like a phone, keyboard, mouse, or touchscreen. • Social interactions like a handshake or hug • Eating and drinking independently • Holding light objects • Pressure relief movements • Some self-catheterization steps |
• Lifting and holding heavy objects • Wheelchair pushing and maneuvering • Eating and drinking independently • Dressing • Improved transfers • Personal hygiene • Writing |
When can I get this surgery? |
Depending on your injury, this surgery is usually done around 6 months after SCI, or could be done years later in some cases. | Any time after SCI. |
How long does healing take? |
You can do light activities immediately after surgery while your skin heals. You can return to normal activities after 2-4 weeks. Avoid weight-bearing, repetitive, or straining activities for 1 month. |
A splint and cast will be used to immobilize your arm for 1-2 months while the tendon heals. Avoid weight-bearing activities and sports for 2-3 months. Some centres may start physical/occupational therapy exercises days after surgery, during the immobilization period. |
How long will rehabilitation take? |
Daily exercises at home and physical/occupational therapy at least once per month for 2 years. | Approximately 3 months Physical/occupational therapy helps you to learn the new movement and makes sure the tendons heal properly. |
How long will it take to see movement? |
First improvements in movement usually happen between 3 to 12 months, depending on the type of nerve transfer. There are accounts of initial movement recovery as late as 2.5 years after surgery. Research shows that movement may continue to improve for years after surgery. |
Improvements in movement usually occur between 1-3 months after surgery. Research shows that movement may continue to improve for up to 12 months after surgery. |
Like with any other surgery, there is a risk of bleeding, infection, and other complications in the healing process. Some people who get a nerve transfer experience temporary weakness in the wrist after surgery that usually returns to normal strength during recovery. Similarly, there may be areas of numbness that develop that often go away over time. So far, the evidence shows that nerve transfer surgeries are safe, and people rarely experience permanent losses in movement or sensation because of the surgery.
Having to rely on others to carry out normal daily activities for a period after surgery can be challenging. A strong social support system and mental health supports can be helpful for recovery.
Some people feel disappointment and frustration with the slow pace at which improvements are made after a nerve transfer. It is important to set realistic expectations going into a nerve transfer. That said, even small improvements in function can have significant impacts on independence and confidence.
As with any surgery, there is a possibility that the nerve transfer surgery does not work. If a nerve transfer fails to restore any function to a paralyzed muscle after physical and occupational therapy, it may be possible to do a tendon transfer to try and regain that movement.
The reasons why a nerve transfer succeeds or fails are still an ongoing area of research. Expert opinion suggests that timing (i.e. when in the recovery process the surgery takes place), and the frequency and intensity of physical and occupational therapy influence how successful a nerve transfer is.
Future research directions for nerve transfer surgeryAlthough nerve transfers are available to people with SCI as a treatment option, it is still a relatively new area of ongoing research. Some of the research underway in the realm of nerve transfer surgery include:
|
There is some evidence that a successful nerve transfer surgery in combination with consistent physical/occupational therapy can lead to increases in the movement, control, and strength of a paralyzed muscle. In recent studies, the nerve transfer surgeries performed were 87.5 – 92% successful at recovering some strength. Better outcomes were seen in people with lower levels of cervical SCI, a greater range of motion and strength in the donor muscle, and more activity in the recipient muscle. More research evidence is needed, but experts are hopeful that nerve transfers can improve the ability to do daily activities such as inserting catheters, relieving pressure, holding and releasing items, and eating. That said, there is some limited evidence that reports people who undergo nerve transfers can experience increases in overall independence and quality of life. It is possible to see improvements for many years after the surgery with continued physical/occupational therapy.
Read Caleb, Ainsley, and Dan’s full interviews in the full article: Community Stories – Experiences of Nerve Transfer Surgery.
Caleb: Nerve Transfer TrifectaAge: 35 Caleb had three nerve transfers on each arm for finger extension, finger flexion, and elbow extension 5 months after SCI. It has been 1 year and 3 months since his surgery. Three months after the surgery, Caleb started to see flickers of movement. There was some loss in strength after the surgery, but at the time he was still weak from the accident that caused his SCI. Caleb can now grip a 5lb kettle bell, while his triceps is still at a flicker but continues to recover. Caleb plans to continue building his finger extension and grip strength to improve his chair skills and everyday living activities. He is hoping that with time, his triceps will have the strength to help with transfers. Overall, Caleb says, “I am very impressed with the whole team and happy with the results!”. |
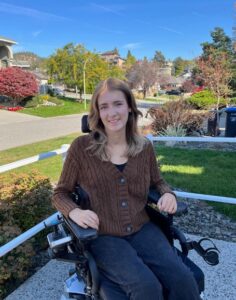
Ainsley: Nerve and Tendon Transfers
Age: 17 Ainsley had three nerve transfers on each arm for hand opening, hand closing, and elbow extension 6 months after SCI. She is now at 2 years post nerve transfer. Ainsley has also had a tendon transfer on the right side. After the surgery, Ainsley could move around right away but had to be careful and was on strong pain medications because of the many incisions. Scar management was important to heal the incisions with minimal scarring and avoid complications. After 2-3 months of visualization exercises, Ainsley noticed the first flickers of movement. By 5-6 months she was using her left hand for tasks. Unfortunately, her right hand didn’t progress beyond a flicker, so Ainsley and her team decided to do a tendon transfer for that side. Ainsley found that the recovery for tendon transfer was more difficult because she was in a cast for 1.5 months and not allowed to move. Today, Ainsley can open both hands, pick things up with her left hand, and extend both arms against gravity. She continues to improve every day but recalls that even before the surgery, “I definitely knew that I had to put in the work to make it stronger.” |
Dan: Nerve Transfer with a Chronic Injury
Dan had nerve transfers on both arms for finger flexion and extension 5 years after his SCI. He’s coming up on 3 years post nerve transfer. Recalling some of the effects right after the surgery, Dan described numbness, loss of strength, and two weeks of pain when raising his arm that “felt like I hit my funny bone but times 100”. Dan’s recovery from nerve transfer was tough and didn’t line up with the picture the surgeons and doctors painted. Because nerve transfers are done more on acute SCIs than chronic SCIs, he suspects the doctors were not aware of how much the surgery could affect the independence of someone living in the community without the supports that exist in in-patient rehabilitation. There needed to be more preparation to accommodate the losses in function he experienced. Considering his rehabilitation, he says, “…you’re on your own so I think it would be better if there was something more – like a program that you do for three months after the surgery”. Three years after the surgery, the numbness and pain from right after surgery have improved, but the losses in strength have persisted. Dan says, “I still have difficulty doing some things that I used to do before the surgery, but not too much.” That said, he has gained the ability to open and extend his fingers and has enough grip to squeeze the hand brakes of the electric bike attachment on his wheelchair. |
Overall, the research on nerve transfer surgeries suggests that it can improve arm/hand muscle function and independence for people with cervical SCI, and that the procedure is safe. However, this is an invasive procedure, so the evidence is limited because it is usually not possible to have randomization or a control group to experimentally demonstrate the benefits.
Extensive assessments are required to determine whether a nerve transfer could work for you. It is important to keep in mind that it may take years of physical/occupational therapy to see the full results of the treatment. There are also external factors to consider, including if you can take time off work/school for recovery, if you have adequate care and support, if you are mentally well enough to have surgery, and what your personal goals are for function. If you are interested in nerve transfer, speak to your health care provider to determine if it’s the right fit for your goals and your injury.
For a review of how we assess evidence at SCIRE Community and advice on making decisions, please see SCIRE Community Evidence.
Nerve and Tendon Transfers to Improve Upper Limb Function in Cervical Spinal Cord Injury (video)
Evidence for “What is nerve transfer surgery?” is based on:
Ahuja, C. S., Wilson, J. R., Nori, S., Kotter, M. R. N., Druschel, C., Curt, A., & Fehlings, M. G. (2017). Traumatic spinal cord injury. Nature Reviews Disease Primers, 3(1), 17018. https://doi.org/10.1038/nrdp.2017.18
Hill, E. J. R., & Fox, I. K. (2019). Current Best Peripheral Nerve Transfers for Spinal Cord Injury. Plastic & Reconstructive Surgery, 143(1), 184e–198e. https://doi.org/10.1097/PRS.0000000000005173
Evidence for “What can nerve transfers help with?” is based on:
Mahar, M., & Cavalli, V. (2018). Intrinsic mechanisms of neuronal axon regeneration. Nature Reviews Neuroscience, 19(6), 323–337. https://doi.org/10.1038/s41583-018-0001-8
Bazarek, S., & Brown, J. M. (2020). The evolution of nerve transfers for spinal cord injury. Experimental Neurology, 333, 113426. https://doi.org/10.1016/j.expneurol.2020.113426
Bunketorp-Käll, L., Reinholdt, C., Fridén, J., & Wangdell, J. (2017). Essential gains and health after upper-limb tetraplegia surgery identified by the International classification of functioning, disability and health (ICF). Spinal Cord, 55(9), 857–863. https://doi.org/10.1038/sc.2017.36
Evidence for Table 1 is based on:
Bazarek, S., & Brown, J. M. (2020). The evolution of nerve transfers for spinal cord injury. Experimental Neurology, 333, 113426. https://doi.org/10.1016/j.expneurol.2020.113426
Galea, M., Messina, A., Hill, B., Cooper, C., Hahn, J., & van Zyl, N. (2020). Reanimating hand function after spinal cord injury using nerve transfer surgery. Advances in Clinical Neuroscience & Rehabilitation, 20(2), 17–19. https://doi.org/10.47795/CQZF2655
Evidence for “Who is suitable for a nerve transfer?” is based on:
Khalifeh, J. M., Dibble, C. F., Van Voorhis, A., Doering, M., Boyer, M. I., Mahan, M. A., Wilson, T. J., Midha, R., Yang, L. J. S., & Ray, W. Z. (2019a). Nerve transfers in the upper extremity following cervical spinal cord injury. Part 1: Systematic review of the literature. Journal of Neurosurgery: Spine, 31(5), 629–640. https://doi.org/10.3171/2019.4.SPINE19173
Dengler, J., Mehra, M., Steeves, J. D., Fox, I. K., Curt, A., Maier, D., Abel, R., Weidner, N., Rupp, R., Vidal, J., Benito, J., Kalke, Y.-B., Curtin, C., Kennedy, C., Miller, A., Novak, C., Ota, D., & Stenson, K. C. (2021). Evaluation of Functional Independence in Cervical Spinal Cord Injury: Implications for Surgery to Restore Upper Limb Function. The Journal of Hand Surgery, 46(7), 621.e1-621.e17. https://doi.org/10.1016/j.jhsa.2020.10.036
Kirshblum, S. C., Burns, S. P., Biering-Sorensen, F., Donovan, W., Graves, D. E., Jha, A., Johansen, M., Jones, L., Krassioukov, A., Mulcahey, M. J., Schmidt-Read, M., & Waring, W. (2011). International standards for neurological classification of spinal cord injury (Revised 2011). The Journal of Spinal Cord Medicine, 34(6), 535–546. https://doi.org/10.1179/204577211X13207446293695
Javeed, S., Dibble, C. F., Greenberg, J. K., Zhang, J. K., Khalifeh, J. M., Park, Y., Wilson, T. J., Zager, E. L., Faraji, A. H., Mahan, M. A., Yang, L. J., Midha, R., Juknis, N., & Ray, W. Z. (2022). Upper Limb Nerve Transfer Surgery in Patients With Tetraplegia. JAMA Netw Open, 5(11), e2243890-. https://doi.org/10.1001/jamanetworkopen.2022.43890
Khalifeh, J. M., Dibble, C. F., Van Voorhis, A., Doering, M., Boyer, M. I., Mahan, M. A., Wilson, T. J., Midha, R., Yang, L. J. S., & Ray, W. Z. (2019b). Nerve transfers in the upper extremity following cervical spinal cord injury. Part 2: Preliminary results of a prospective clinical trial. Journal of Neurosurgery: Spine, 31(5). https://doi.org/10.3171/2019.4.SPINE19399
van Zyl, N., Hill, B., Cooper, C., Hahn, J., & Galea, M. P. (2019). Expanding traditional tendon-based techniques with nerve transfers for the restoration of upper limb function in tetraplegia: a prospective case series. Lancet, 394(10198), 565–575. https://doi.org/10.1016/S0140-6736(19)31143-2
Stanley, E. A., Hill, B., McKenzie, D. P., Chapuis, P., Galea, M. P., & N, van Z. (2022). Predicting strength outcomes for upper limb nerve transfer surgery in tetraplegia. J Hand Surg Eur Vol, 47(11), 1114–1120. https://doi.org/10.1177/17531934221113739
Berger, M. J., Dengler, J., Westman, A., Curt, A., Schubert, M., Abel, R., Weidner, N., Röhrich, F., & Fox, I. K. (2023). Nerve transfer after cervical spinal cord injury: Who has a “time sensitive” injury based on electrodiagnostic findings? Archives of Physical Medicine and Rehabilitation. https://doi.org/10.1016/j.apmr.2023.11.003
Bryden, A. M., Hoyen, H. A., Keith, M. W., Mejia, M., Kilgore, K. L., & Nemunaitis, G. A. (2016). Upper Extremity Assessment in Tetraplegia: The Importance of Differentiating Between Upper and Lower Motor Neuron Paralysis. Archives of Physical Medicine and Rehabilitation, 97(6), S97–S104. https://doi.org/10.1016/j.apmr.2015.11.021
Castanov, V., Berger, M., Ritsma, B., Trier, J., & Hendry, J. M. (2021). Optimizing the Timing of Peripheral Nerve Transfers for Functional Re-Animation in Cervical Spinal Cord Injury: A Conceptual Framework. Journal of Neurotrauma, 38(24), 3365–3375. https://doi.org/10.1089/neu.2021.0247
Hill, E. J. R., & Fox, I. K. (2019). Current Best Peripheral Nerve Transfers for Spinal Cord Injury. Plastic & Reconstructive Surgery, 143(1), 184e–198e. https://doi.org/10.1097/PRS.0000000000005173
Jain, N. S., Hill, E. J. R., Zaidman, C. M., Novak, C. B., Hunter, D. A., Juknis, N., Ruvinskaya, R., Kennedy, C. R., Vetter, J., Mackinnon, S. E., & Fox, I. K. (2020). Evaluation for Late Nerve Transfer Surgery in Spinal Cord Injury: Predicting the Degree of Lower Motor Neuron Injury. J Hand Surg Am, 45(2), 95–103. https://doi.org/10.1016/j.jhsa.2019.11.003
Fox, I. K., Novak, C. B., Krauss, E. M., Hoben, G. M., Zaidman, C. M., Ruvinskaya, R., Juknis, N., Winter, A. C., & Mackinnon, S. E. (2018). The Use of Nerve Transfers to Restore Upper Extremity Function in Cervical Spinal Cord Injury. PM&R, 10(11), 1173. https://doi.org/10.1016/j.pmrj.2018.03.013
Evidence for “What is the process for a nerve transfer?” is based on:
Dengler, J., Steeves, J. D., Curt, A., Mehra, M., Novak, C. B., & Fox, I. K. (2022). Spontaneous Motor Recovery after Cervical Spinal Cord Injury: Issues for Nerve Transfer Surgery Decision Making. Spinal Cord, 60(10), 922–927. https://doi.org/10.1038/s41393-022-00834-6
Hill, E. J. R., & Fox, I. K. (2019). Current Best Peripheral Nerve Transfers for Spinal Cord Injury. Plastic & Reconstructive Surgery, 143(1), 184e–198e. https://doi.org/10.1097/PRS.0000000000005173
Kane, N. M., & Oware, A. (2012). Nerve conduction and electromyography studies. Journal of Neurology, 259(7), 1502–1508. https://doi.org/10.1007/s00415-012-6497-3
Berger, M. J., Dengler, J., Westman, A., Curt, A., Schubert, M., Abel, R., Weidner, N., Röhrich, F., & Fox, I. K. (2023). Nerve transfer after cervical spinal cord injury: Who has a “time sensitive” injury based on electrodiagnostic findings? Archives of Physical Medicine and Rehabilitation. https://doi.org/10.1016/j.apmr.2023.11.003
Bersch, I., & Fridén, J. (2020). Upper and lower motor neuron lesions in tetraplegia: implications for surgical nerve transfer to restore hand function. J Appl Physiol (1985), 129(5), 1214–1219. https://doi.org/10.1152/japplphysiol.00529.2020
van Zyl, N., Hill, B., Cooper, C., Hahn, J., & Galea, M. P. (2019). Expanding traditional tendon-based techniques with nerve transfers for the restoration of upper limb function in tetraplegia: a prospective case series. Lancet, 394(10198), 565–575. https://doi.org/10.1016/S0140-6736(19)31143-2
Fox, I. K., Miller, A. K., & Curtin, C. M. (2018). Nerve and Tendon Transfer Surgery in Cervical Spinal Cord Injury: Individualized Choices to Optimize Function. Topics in Spinal Cord Injury Rehabilitation, 24(3), 275–287. https://doi.org/10.1310/sci2403-275
Kahn, L. C., Evans, A. G., Hill, E. J. R., & Fox, I. K. (2022). Donor activation focused rehabilitation approach to hand closing nerve transfer surgery in individuals with cervical level spinal cord injury. Spinal Cord Ser Cases, 8(1), 47. https://doi.org/10.1038/s41394-022-00512-y
Aguirre-Güemez, A. V, Mendoza-Muñoz, M., Jiménez-Coello, G., Rhoades-Torres, G. M., Pérez-Zavala, R., Barrera-Ortíz, A., & Quinzaños-Fresnedo, J. (2021). Nerve transfer rehabilitation in tetraplegia: Comprehensive assessment and treatment program to improve upper extremity function before and after nerve transfer surgery, a case report. J Spinal Cord Med, 44(4), 621–626. https://doi.org/10.1080/10790268.2019.1660841
Javeed, S., Dibble, C. F., Greenberg, J. K., Zhang, J. K., Khalifeh, J. M., Park, Y., Wilson, T. J., Zager, E. L., Faraji, A. H., Mahan, M. A., Yang, L. J., Midha, R., Juknis, N., & Ray, W. Z. (2022). Upper Limb Nerve Transfer Surgery in Patients With Tetraplegia. JAMA Netw Open, 5(11), e2243890-. https://doi.org/10.1001/jamanetworkopen.2022.43890
Larocerie-Salgado, J., Chinchalkar, S., Ross, D. C., Gillis, J., Doherty, C. D., & Miller, T. A. (2022). Rehabilitation Following Nerve Transfer Surgery. Techniques in Hand & Upper Extremity Surgery, 26(2), 71–77. https://doi.org/10.1097/BTH.0000000000000359
Opsommer, E., Chevalley, O., & Korogod, N. (2020). Motor imagery for pain and motor function after spinal cord injury: a systematic review. Spinal Cord, 58(3), 262–274. https://doi.org/10.1038/s41393-019-0390-1
Evidence for “How do nerve transfers compare to tendon transfers?” is based on:
Bazarek, S., & Brown, J. M. (2020). The evolution of nerve transfers for spinal cord injury. Experimental Neurology, 333, 113426. https://doi.org/10.1016/j.expneurol.2020.113426
van Zyl, N., Hill, B., Cooper, C., Hahn, J., & Galea, M. P. (2019). Expanding traditional tendon-based techniques with nerve transfers for the restoration of upper limb function in tetraplegia: a prospective case series. Lancet, 394(10198), 565–575. https://doi.org/10.1016/S0140-6736(19)31143-2
Evidence for Table 2 is based on:
van Zyl, N., Hill, B., Cooper, C., Hahn, J., & Galea, M. P. (2019). Expanding traditional tendon-based techniques with nerve transfers for the restoration of upper limb function in tetraplegia: a prospective case series. Lancet, 394(10198), 565–575. https://doi.org/10.1016/S0140-6736(19)31143-2
Aguirre-Güemez, A. V, Mendoza-Muñoz, M., Jiménez-Coello, G., Rhoades-Torres, G. M., Pérez-Zavala, R., Barrera-Ortíz, A., & Quinzaños-Fresnedo, J. (2021). Nerve transfer rehabilitation in tetraplegia: Comprehensive assessment and treatment program to improve upper extremity function before and after nerve transfer surgery, a case report. J Spinal Cord Med, 44(4), 621–626. https://doi.org/10.1080/10790268.2019.1660841
Kahn, L. C., Evans, A. G., Hill, E. J. R., & Fox, I. K. (2022). Donor activation focused rehabilitation approach to hand closing nerve transfer surgery in individuals with cervical level spinal cord injury. Spinal Cord Ser Cases, 8(1), 47. https://doi.org/10.1038/s41394-022-00512-y
Bunketorp-Käll, L., Reinholdt, C., Fridén, J., & Wangdell, J. (2017). Essential gains and health after upper-limb tetraplegia surgery identified by the International classification of functioning, disability and health (ICF). Spinal Cord, 55(9), 857–863. https://doi.org/10.1038/sc.2017.36
Fox, I. K., Miller, A. K., & Curtin, C. M. (2018). Nerve and Tendon Transfer Surgery in Cervical Spinal Cord Injury: Individualized Choices to Optimize Function. Topics in Spinal Cord Injury Rehabilitation, 24(3), 275–287. https://doi.org/10.1310/sci2403-275
Dunn, J. A., Sinnott, K. A., Rothwell, A. G., Mohammed, K. D., & Simcock, J. W. (2016). Tendon Transfer Surgery for People With Tetraplegia: An Overview. Archives of Physical Medicine and Rehabilitation, 97(6), S75–S80. https://doi.org/10.1016/j.apmr.2016.01.034
Javeed, S., Dibble, C. F., Greenberg, J. K., Zhang, J. K., Khalifeh, J. M., Park, Y., Wilson, T. J., Zager, E. L., Faraji, A. H., Mahan, M. A., Yang, L. J., Midha, R., Juknis, N., & Ray, W. Z. (2022). Upper Limb Nerve Transfer Surgery in Patients With Tetraplegia. JAMA Netw Open, 5(11), e2243890-. https://doi.org/10.1001/jamanetworkopen.2022.43890
Evidence for “What are the risks of nerve transfers?” is based on:
Francoisse, C. A., Russo, S. A., Skladman, R., Kahn, L. C., Kennedy, C., Stenson, K. C., Novak, C. B., & Fox, I. K. (2022). Quantifying Donor Deficits Following Nerve Transfer Surgery in Tetraplegia. J Hand Surg Am, 47(12), 1157–1165. https://doi.org/10.1016/j.jhsa.2022.08.014
van Zyl, N., Hill, B., Cooper, C., Hahn, J., & Galea, M. P. (2019). Expanding traditional tendon-based techniques with nerve transfers for the restoration of upper limb function in tetraplegia: a prospective case series. Lancet, 394(10198), 565–575. https://doi.org/10.1016/S0140-6736(19)31143-2
Bertelli, J. A., & Ghizoni, M. F. (2017). Nerve transfers for restoration of finger flexion in patients with tetraplegia. Journal of Neurosurgery: Spine, 26(1), 55–61. https://doi.org/10.3171/2016.5.SPINE151544
Wilson, T. J. (2019). Novel Uses of Nerve Transfers. Neurotherapeutics, 16(1), 26–35. https://doi.org/10.1007/s13311-018-0664-x Khalifeh, J. M., Dibble, C. F., Van Voorhis, A., Doering, M., Boyer, M. I., Mahan, M. A., Wilson, T. J., Midha, R., Yang, L. J. S., & Ray, W. Z. (2019a). Nerve transfers in the upper extremity following cervical spinal cord injury. Part 1: Systematic review of the literature. Journal of Neurosurgery: Spine, 31(5), 629–640. https://doi.org/10.3171/2019.4.SPINE19173
Mooney, A., Hewitt, A. E., & Hahn, J. (2021). Nothing to lose: a phenomenological study of upper limb nerve transfer surgery for individuals with tetraplegia. Disabil Rehabil, 43(26), 3748–3756. https://doi.org/10.1080/09638288.2020.1750716
Hill, E. J. R., & Fox, I. K. (2019). Current Best Peripheral Nerve Transfers for Spinal Cord Injury. Plastic & Reconstructive Surgery, 143(1), 184e–198e. https://doi.org/10.1097/PRS.0000000000005173
Evidence for “What are the limitations of nerve transfers?” is based on:
Mooney, A., Hewitt, A. E., & Hahn, J. (2021). Nothing to lose: a phenomenological study of upper limb nerve transfer surgery for individuals with tetraplegia. Disabil Rehabil, 43(26), 3748–3756. https://doi.org/10.1080/09638288.2020.1750716
Hill, E. J. R., & Fox, I. K. (2019). Current Best Peripheral Nerve Transfers for Spinal Cord Injury. Plastic & Reconstructive Surgery, 143(1), 184e–198e. https://doi.org/10.1097/PRS.0000000000005173
Heredia Gutiérrez, A., Cachón Cámara, G. E., González Carranza, V., Torres García, S., & Chico Ponce de León, F. (2020). Phrenic nerve neurotization utilizing half of the spinal accessory nerve to the functional restoration of the paralyzed diaphragm in high spinal cord injury secondary to brain tumor resection. Child’s Nervous System, 36(6), 1307–1310. https://doi.org/10.1007/s00381-019-04490-9
Bazarek, S., & Brown, J. M. (2020). The evolution of nerve transfers for spinal cord injury. Experimental Neurology, 333, 113426. https://doi.org/10.1016/j.expneurol.2020.113426
Evidence for “Are nerve transfers effective?” is based on:
Javeed, S., Dibble, C. F., Greenberg, J. K., Zhang, J. K., Khalifeh, J. M., Park, Y., Wilson, T. J., Zager, E. L., Faraji, A. H., Mahan, M. A., Yang, L. J., Midha, R., Juknis, N., & Ray, W. Z. (2022). Upper Limb Nerve Transfer Surgery in Patients With Tetraplegia. JAMA Netw Open, 5(11), e2243890-. https://doi.org/10.1001/jamanetworkopen.2022.43890
Khalifeh, J. M., Dibble, C. F., Van Voorhis, A., Doering, M., Boyer, M. I., Mahan, M. A., Wilson, T. J., Midha, R., Yang, L. J. S., & Ray, W. Z. (2019b). Nerve transfers in the upper extremity following cervical spinal cord injury. Part 2: Preliminary results of a prospective clinical trial. Journal of Neurosurgery: Spine, 31(5). https://doi.org/10.3171/2019.4.SPINE19399
Stanley, E. A., Hill, B., McKenzie, D. P., Chapuis, P., Galea, M. P., & N, van Z. (2022). Predicting strength outcomes for upper limb nerve transfer surgery in tetraplegia. J Hand Surg Eur Vol, 47(11), 1114–1120. https://doi.org/10.1177/17531934221113739
van Zyl, N., Hill, B., Cooper, C., Hahn, J., & Galea, M. P. (2019). Expanding traditional tendon-based techniques with nerve transfers for the restoration of upper limb function in tetraplegia: a prospective case series. Lancet, 394(10198), 565–575. https://doi.org/10.1016/S0140-6736(19)31143-2
Image credits
- Nerve Transfer by SCIRE
- Elbow Extension by SCIRE
- Wrist Extension by SCIRE
- Finger Extension by SCIRE
- Finger Flexion and Pinch by SCIRE
- Nerve and Tendon Transfers to Improve Upper Limb Function in Cervical Spinal Cord Injury (video)
- Nerve Transfer Level of Injury by SCIRE
- Time Sensitive Nerve Transfers by SCIRE
- Nerve Transfer Timeline by SCIRE
- Tendon Transfer by SCIRE
- Photo provided by participant (Caleb)
- Photo provided by participant (Ainsley)
- Photo provided by participant (Dan)








 Age: 37
Age: 37