Author: Sharon Jang | Reviewer: Sonja de Groot | Published: 20 April 2022 | Updated: XX October 2024
Physical activity after spinal cord injury (SCI) can provide many health benefits, as in the able-bodied population. This page covers the benefits of exercising with an SCI, precautions, and adaptations to exercising with an SCI.
Key Points
- Exercising after an SCI can improve muscle strength, type, and size, your abilities to do things on a day-to-day basis, your well-being, and decrease risks for secondary complications.
- There are many ways to get physically active, including sports, being active in the community, and going to the gym.
- Many exercises and sports can be adapted for those with SCI using adaptive equipment.
- Although rare, some secondary complications such as autonomic dysreflexia (AD), orthostatic hypotension (OH), skin breakdown, and temperature regulation, may arise.
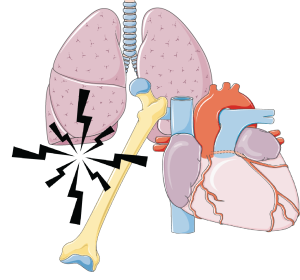
After SCI, there is deconditioning of muscles, bones, joints, and changes in the heart and blood vessels due to inactivity. This can lead to various secondary complications, such as heart disease, breathing complications, weakening of the bones (osteoporosis), pain, spasticity, and diabetes. Exercise has many positive changes for those with an SCI including muscle type and size, improved muscle strength, independence, well-being, and helping to prevent secondary health complications.
Muscle type, size, and strength
 In the body, there are 2 main types of muscle fibers: slow twitch (type I) and fast twitch (type II). Slow twitch muscles are known as the endurance muscles, as they are able to hold a contraction for a long period of time before getting tired. For example, the muscles that are used to keep your head upright are mostly made up of slow twitch muscle fibers. Type II fibers are known for their short burst of speed or strength. They can generate more strength, but get tired really quickly. Over time with an SCI, the muscles with the endurance type (type I) tend to turn into the more fatigable type (type II). There is some moderate-weak evidence that shows that among those with limited movement in their legs, the use of functional electrical stimulation (FES) can help shift muscle fibers from being more fatigable to more endurance based.
In the body, there are 2 main types of muscle fibers: slow twitch (type I) and fast twitch (type II). Slow twitch muscles are known as the endurance muscles, as they are able to hold a contraction for a long period of time before getting tired. For example, the muscles that are used to keep your head upright are mostly made up of slow twitch muscle fibers. Type II fibers are known for their short burst of speed or strength. They can generate more strength, but get tired really quickly. Over time with an SCI, the muscles with the endurance type (type I) tend to turn into the more fatigable type (type II). There is some moderate-weak evidence that shows that among those with limited movement in their legs, the use of functional electrical stimulation (FES) can help shift muscle fibers from being more fatigable to more endurance based.
After injury, muscles in the body slowly begin to become smaller (atrophy). However, there is moderate to weak evidence that indicates that moving your arms and legs, either passively or actively, can help build muscle up again. Two (weak evidence) studies found that amongst those with limited to no leg function, electrical stimulation (Neuromuscular electrical stimulation (NMES) or FES) can increase the size of the thigh muscles. In addition, there is weak evidence that the use of a body-weight support treadmill can also increase the size of the lower leg muscle, resulting in a partial reversal of muscle shrinking.
 There is strong-moderate evidence that exercising can help individuals of any injury level improve their strength. Among those with paraplegia, there is strong evidence that strength training (i.e., doing weight training) can improve muscle strength in the arms. There is also strong evidence showing that body weight support training can improve overall muscle strength, and moderate evidence that arm cycling can help strengthen the arms and the front of the shoulder. Among those with tetraplegia, there is strong evidence that the use of FES on the arm and shoulder can improve muscle strengthening. Moreover, strong evidence suggests that neuromuscular stimulation (NMES) can improve strength among those with cervical level injuries. If you are unable to access specialized equipment, strength training with free weights or using an arm cycle can show similar benefits as well.
There is strong-moderate evidence that exercising can help individuals of any injury level improve their strength. Among those with paraplegia, there is strong evidence that strength training (i.e., doing weight training) can improve muscle strength in the arms. There is also strong evidence showing that body weight support training can improve overall muscle strength, and moderate evidence that arm cycling can help strengthen the arms and the front of the shoulder. Among those with tetraplegia, there is strong evidence that the use of FES on the arm and shoulder can improve muscle strengthening. Moreover, strong evidence suggests that neuromuscular stimulation (NMES) can improve strength among those with cervical level injuries. If you are unable to access specialized equipment, strength training with free weights or using an arm cycle can show similar benefits as well.
Activities of Daily Living
 There is some moderate evidence that shows that exercising can enhance the ability to perform daily tasks by yourself. Exercising improves your fitness level (such as your strength and endurance), which can help you perform daily tasks. More specifically, tasks may become easier by reducing physical strain and a decrease in the amount of time required to do an activity. One moderate evidence study found that doing physical therapy exercises in addition to neuromuscular stimulation enhanced participant’s ability to perform self-care (e.g., dressing, feeding, toileting) and mobility (e.g., transferring, wheelchair pushing). Other weak evidence supports these findings, as they found that exercise can help improve transferring and the ability to put on/take off clothing, wheeling and cleaning. Furthermore, increased fitness levels have also been associated with return to work.
There is some moderate evidence that shows that exercising can enhance the ability to perform daily tasks by yourself. Exercising improves your fitness level (such as your strength and endurance), which can help you perform daily tasks. More specifically, tasks may become easier by reducing physical strain and a decrease in the amount of time required to do an activity. One moderate evidence study found that doing physical therapy exercises in addition to neuromuscular stimulation enhanced participant’s ability to perform self-care (e.g., dressing, feeding, toileting) and mobility (e.g., transferring, wheelchair pushing). Other weak evidence supports these findings, as they found that exercise can help improve transferring and the ability to put on/take off clothing, wheeling and cleaning. Furthermore, increased fitness levels have also been associated with return to work.
Well-being
 Some evidence suggests that exercise can help individuals improve perceptions of well-being. Well-being has been defined as how well an individual feels in their mind, their satisfaction with their health and functioning, and their overall satisfaction in life. Two aspects of well-being that are relatively well-researched are the impact of physical activity on depression and quality of life. There is weak evidence that found that all types of physical activity can help improve depressive symptoms and can improve quality of life. This relationship between physical activity and depressive symptoms and quality of life can be explained by a strong evidence study, which indicates that exercise can lead to decreased stress and pain. For example, strong evidence has shown that exercise can reduce shoulder pain, which can allow individuals to perform a greater variety of movements without consequences. The reduction in stress and pain, in turn, is thought to improve quality of life and depressive symptoms. However, many of these studies lack a control group. As a result, we are unable to determine if physical activity alone has an influence on subjective well-being.
Some evidence suggests that exercise can help individuals improve perceptions of well-being. Well-being has been defined as how well an individual feels in their mind, their satisfaction with their health and functioning, and their overall satisfaction in life. Two aspects of well-being that are relatively well-researched are the impact of physical activity on depression and quality of life. There is weak evidence that found that all types of physical activity can help improve depressive symptoms and can improve quality of life. This relationship between physical activity and depressive symptoms and quality of life can be explained by a strong evidence study, which indicates that exercise can lead to decreased stress and pain. For example, strong evidence has shown that exercise can reduce shoulder pain, which can allow individuals to perform a greater variety of movements without consequences. The reduction in stress and pain, in turn, is thought to improve quality of life and depressive symptoms. However, many of these studies lack a control group. As a result, we are unable to determine if physical activity alone has an influence on subjective well-being.
Secondary complications
After sustaining an SCI, multiple secondary complications can occur. However, research suggests that exercise can help prevent or reduce the severity of secondary complications, including:
 Conditions impacting the heart and blood vessels, by improving the strength of the heart and balancing out the sympathetic (fight or flight; stimulation) and parasympathetic (relax and slowing) nervous systems,
Conditions impacting the heart and blood vessels, by improving the strength of the heart and balancing out the sympathetic (fight or flight; stimulation) and parasympathetic (relax and slowing) nervous systems,- Breathing complications, through strengthening the muscles required for breathing and through increasing the amounts of oxygen taken up by the body,
- Weakened bones, by increasing bone mass density,
- Type II diabetes, through improving the balance of blood sugar (glucose),
- Pain, through strengthening, and
- Spasticity, which can be reduced short term with exercising.
 There are many ways for you to remain physically active, even after SCI! Strength training can be done at a local community center or private gym, most often with the equipment already there. Strength training can also be done at home with free weights and exercise bands. Some equipment that can be used for strength training include free weights, exercise bands, and pulleys. For aerobic exercise, some alternatives include using an arm ergometer (arm cycle), a rowing machine (if possible), and adaptive rowers, such as the Ski-Erg.
There are many ways for you to remain physically active, even after SCI! Strength training can be done at a local community center or private gym, most often with the equipment already there. Strength training can also be done at home with free weights and exercise bands. Some equipment that can be used for strength training include free weights, exercise bands, and pulleys. For aerobic exercise, some alternatives include using an arm ergometer (arm cycle), a rowing machine (if possible), and adaptive rowers, such as the Ski-Erg.
 Adaptive sports is another way to get active. There are a variety of adaptive sports, including court sports (e.g., basketball, rugby, tennis), water sports (e.g., sailing, kayaking), race sports (e.g., cycling, track and field), and winter sports (e.g., Nordic and alpine skiing).
Adaptive sports is another way to get active. There are a variety of adaptive sports, including court sports (e.g., basketball, rugby, tennis), water sports (e.g., sailing, kayaking), race sports (e.g., cycling, track and field), and winter sports (e.g., Nordic and alpine skiing).
Refer to our article on Adapted Sports & Equipment for more information!
 Alternatively, specialty equipment is available to help facilitate exercise after SCI. However, this equipment is more commonly used in rehabilitation settings, as they are very expensive and additional assistance is often required. A Functional Electrical Stimulation (FES) bike can be used to simulate the legs while cycling, and has been shown improve strength and endurance. Body-weight Support Treadmills are specialized treadmills with a sling attached. This type of treadmill allows an individual to move their legs on the treadmill, while having their bodyweight supported by a sling. Some models are available to allow users to control how much of their bodyweight they feel while in the treadmill, which can alter the challenge of walking.
Alternatively, specialty equipment is available to help facilitate exercise after SCI. However, this equipment is more commonly used in rehabilitation settings, as they are very expensive and additional assistance is often required. A Functional Electrical Stimulation (FES) bike can be used to simulate the legs while cycling, and has been shown improve strength and endurance. Body-weight Support Treadmills are specialized treadmills with a sling attached. This type of treadmill allows an individual to move their legs on the treadmill, while having their bodyweight supported by a sling. Some models are available to allow users to control how much of their bodyweight they feel while in the treadmill, which can alter the challenge of walking.
If going to the gym or playing sports is not your thing, there are still other ways to get active! Performing daily tasks can be hard work as well. For example, activities such as heavy gardening, going grocery shopping and carrying home groceries, doing a lot of housework such as vacuuming and cleaning the house, going for a push with family/friends are all ways of being active. However, if these are your activity of choice, you want to make sure you are pushing yourself enough to get your heart rate up and keep it up for a while.
In 2020, exercise guidelines for the SCI population were released. Currently, the starting level guidelines for fitness benefits are:
- at least 20 minutes of moderate to vigorous intensity endurance (aerobic) exercise, 2 times per week
- 3 sets of strength exercises for each major muscle group at a moderate to vigorous intensity, 2 times a week.
 The advance level provides guidelines for additional fitness and health benefits, such as reducing your risk for diabetes. It is recommended to get at least 30 minutes of moderate to vigorous intensity aerobic exercise at least 3 times a week, in addition to the 3 sets of strength exercises twice a week.
The advance level provides guidelines for additional fitness and health benefits, such as reducing your risk for diabetes. It is recommended to get at least 30 minutes of moderate to vigorous intensity aerobic exercise at least 3 times a week, in addition to the 3 sets of strength exercises twice a week.
Refer to our article on Exercise Guidelines for Adults with SCI for more information!
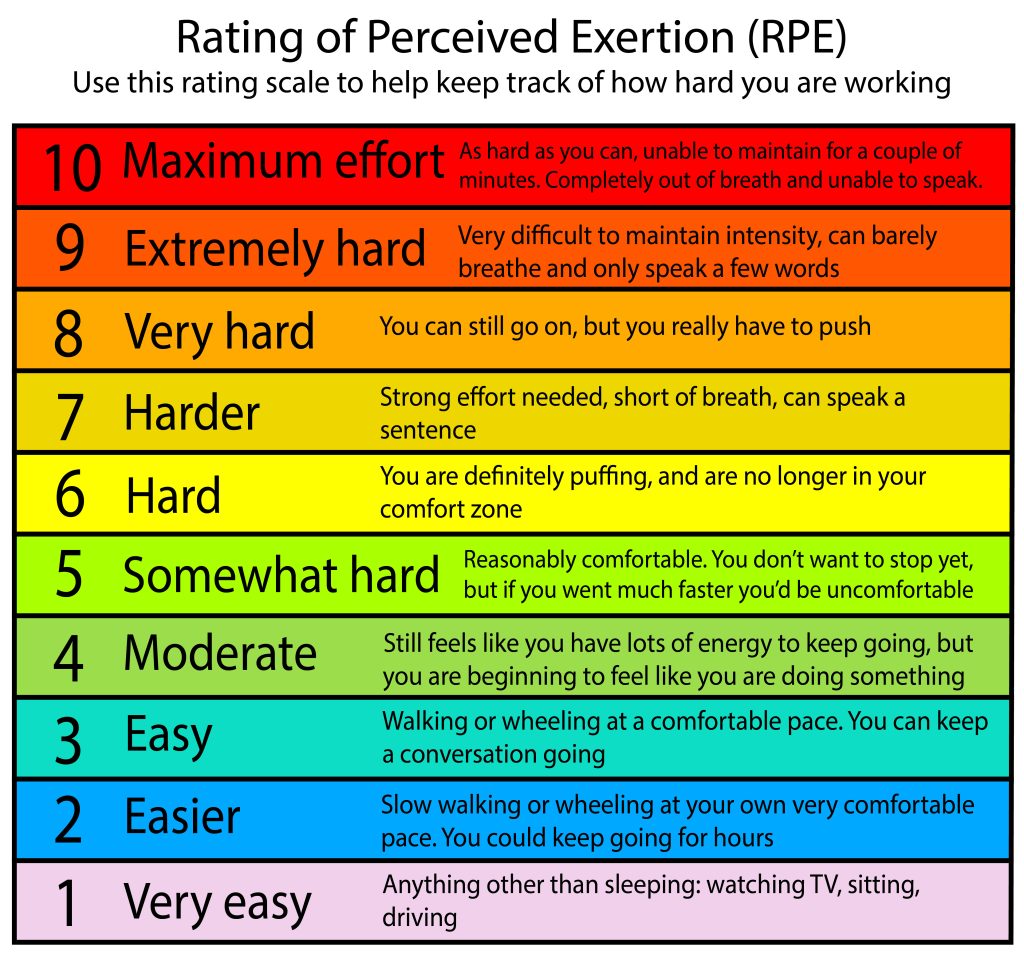
Another way to gauge your effort is through a Rating of Perceived Exertion (RPE). The RPE is a subjective rating scale where the individual rates how hard they feel they are working, where 0 is not working at all, and 10 is working at your absolute maximum. If someone is just starting off with exercising, starting between a 5-7 on the RPE scale is a good idea.

Watch SCIRE’s YouTube Video explaining how to use RPE when exercising!
Another way to evaluate how hard you are working is through using the talk test. The talk test uses your ability to carry out a conversation while performing exercise to gauge exercise intensity. According to the talk test, a moderate intensity workout is achieved when one is able to talk to someone while working out, but not being able to sing. During a vigorous intensity workout, you would only be able to say a couple of words to someone, and speaking is difficult.

Watch SCIRE’s YouTube video explaining how to adapt exercises.
Going back into a gym after an SCI may be daunting given that much of the equipment may no longer be accessible. However, there are a number of ways to adapt gym equipment, including grip assistance, transfer boards, chest straps, and using free weights and wedges. When exercising at a gym, you may require some additional assistance getting set up on pieces of equipment. If this is the case, consider going with a family member or a friend, and don’t be afraid to ask the gym attendant for help.

Adaptive grip aids include commercial gloves (left), tensor bandages (upper right) and weight lifting cuffs (bottom right).
After a high-level SCI, hand functioning may be impaired, resulting in a lack of ability to grip. To address this in a gym setting, some available options include using tensor bands, commercially available gloves, or weight-lifting cuffs. Tensor bandages can be used to wrap your hands around a handlebar. Benefits of using a tensor bandage include wide availability and low cost. Commercially available gloves, such as the Active Hands, are also available to assist with grip function on handles. These gloves provide a bit more support to the wrist and have a Velcro strap around the wrist. They also have a second Velcro that goes over the hand, which secures the hand to the handle. However, commercial gloves may not be as readily available and are usually expensive. Lastly, some individuals use weight-lifting cuffs, which are available at most gyms for use, to assist with grip function. These cuffs have a Velcro strap that goes around the wrist and a hook that can be connected to handlebars. Although commonly found in gyms, weightlifting cuffs only work for specific movements, such as pushing and pulling. In addition, they might not fit around handles of all sizes.

An abdominal binder (circled in red) being used to help keep an upright posture during rowing.
Abdominal (core) function is often impacted with an SCI, which may limit the types of activities you are able to do. One way to address this issue is through the use of a chest strap. A chest strap is a neoprene strap that comes in differing widths but is often wide enough to cover your abdominal area. The idea is to wrap the chest strap around the backrest of your wheelchair and around your torso, preventing you from falling forward if you are doing a pulling exercise. Chest straps are commonly used in various wheelchair sports as well, to provide additional support.
Refer to our article on Abdominal Binders for more information!
When exercising in a wheelchair, you may find that the wheel lock still allows for some movement in the wheels, which may hinder an exercise. One way to address this situation is through adding additional support at the base of the wheel using wedges or free weights. Free weights can be placed behind the rear tire on both sides, or in front of the rear tire on both sides. In place, small wooden wedges (or door stoppers) can be placed under the tires on all four sides (in front and at the back) to help prevent rocking.

Watch SCIRE’s YouTube video explaining potential complications during exercise.
Exercise is relatively safe for individuals with SCI. However, there are some complications that, while rare, can arise.
Low blood pressure
 When you first start exercising, it is common to possibly feel some nausea, or like you might pass out. This is a result of exercise-induced (exertional) hypotension, or a sudden drop in blood pressure due to exercise. One way to overcome this is to build up your exercise routine. When doing aerobic exercises, try a discontinuous approach: exercise for 2-3 minutes, then take a break. The idea is to slowly increase the length of exercising before you require a break, working your way up to 20-30 minutes of exercise. Once you are able to continuously exercise for 20-30 minutes, then you may consider increasing the resistance.
When you first start exercising, it is common to possibly feel some nausea, or like you might pass out. This is a result of exercise-induced (exertional) hypotension, or a sudden drop in blood pressure due to exercise. One way to overcome this is to build up your exercise routine. When doing aerobic exercises, try a discontinuous approach: exercise for 2-3 minutes, then take a break. The idea is to slowly increase the length of exercising before you require a break, working your way up to 20-30 minutes of exercise. Once you are able to continuously exercise for 20-30 minutes, then you may consider increasing the resistance.
Autonomic Dysreflexia
 Autonomic dysreflexia is a condition where blood pressure suddenly increases to dangerous levels. If this occurs, stop exercising. Sit up and try to lower your legs if possible, loosen any tight clothing, and move off of any high-pressure areas (e.g., sit bones, hands/wrists if you are using assistive grip). If symptoms do not go away, seek medical attention.
Autonomic dysreflexia is a condition where blood pressure suddenly increases to dangerous levels. If this occurs, stop exercising. Sit up and try to lower your legs if possible, loosen any tight clothing, and move off of any high-pressure areas (e.g., sit bones, hands/wrists if you are using assistive grip). If symptoms do not go away, seek medical attention.
Refer to our article on Autonomic Dysreflexia for more information!
Temperature regulation
 With a high level injury, temperature dysregulation, the body’s inability to control temperature, may be influenced. The ability to produce sweat can be compromised with higher levels of injury, resulting in an inability to cool down the body. In colder environments, it may be harder to warm up.
With a high level injury, temperature dysregulation, the body’s inability to control temperature, may be influenced. The ability to produce sweat can be compromised with higher levels of injury, resulting in an inability to cool down the body. In colder environments, it may be harder to warm up.
When exercising in hot or warmer environments, make sure you are drinking water consistently throughout your workout. Consider wearing looser clothing, and try to work out in an environment with ventilation, fans, or air conditioning. If you notice that you tend to overheat during exercise and are unable to sweat, you can also try carrying a spray bottle with you and spray your face down to cool off. When exercising in cooler environments, be mindful of your hands, arms, legs, and feet and make sure they aren’t getting too cold. Try dressing in layers so you can wear more if necessary, but also take layers off if you get warm.
Skin concerns
![]() When exercising, it is important to be cautious of skin integrity, especially if you have no sensation. One area to be mindful of is the back when performing rocking or twisting motions. Rocking and twisting movements may cause the back to rub on the backrest of the wheelchair, creating a potential for skin breakdown. Another area to be mindful of is areas used with straps, such as the hands and sometimes the feet. For example, if using a grip aid for a longer duration of time to perform an activity, you may want to check for red spots that may have been caused by the straps. Ensure to check your skin after exercising for redness.
When exercising, it is important to be cautious of skin integrity, especially if you have no sensation. One area to be mindful of is the back when performing rocking or twisting motions. Rocking and twisting movements may cause the back to rub on the backrest of the wheelchair, creating a potential for skin breakdown. Another area to be mindful of is areas used with straps, such as the hands and sometimes the feet. For example, if using a grip aid for a longer duration of time to perform an activity, you may want to check for red spots that may have been caused by the straps. Ensure to check your skin after exercising for redness.
Refer to our article on Pressure Injuries for more information!
Overuse injuries
 Overuse injuries occur when you exercise muscles that are already often used on a daily/frequent basis. An example of this is the shoulders, as it is used for pushing a wheelchair. To prevent overuse injury, make sure you have the correct posture when performing exercises. When working on the shoulder, try to consider alternatives to pushing your wheelchair as exercise, if possible. For example, the use of an arm bike could be an alternative to get around as they require less demand on your shoulders and arms. In addition, try to balance aerobic exercise and strength training in muscle groups prone to overuse injuries.
Overuse injuries occur when you exercise muscles that are already often used on a daily/frequent basis. An example of this is the shoulders, as it is used for pushing a wheelchair. To prevent overuse injury, make sure you have the correct posture when performing exercises. When working on the shoulder, try to consider alternatives to pushing your wheelchair as exercise, if possible. For example, the use of an arm bike could be an alternative to get around as they require less demand on your shoulders and arms. In addition, try to balance aerobic exercise and strength training in muscle groups prone to overuse injuries.
Benefits of physical activity as you age

Watch SCIRE’s video explaining to learn about ways to stay active as you age.20
It is normal as you age for the function of body systems and organs to gradually decline. People with SCI and other disabilities may find that this process starts earlier in life and has a bigger impact on daily function. Physical activity is important to keep your body and mind healthy. Physical activity can help someone aging with SCI prevent and slow down losses in function, independence, and quality of life. Small changes in muscle strength, heart health, breathing, or pain can have big impacts on the daily activities of someone with SCI. Physical activity can also be a good way to socialize if you are able to join a community group or program.
Physical activity can help keep your body healthy in many ways:
- Improve or maintain muscle strength
- Improve or maintain mobility
- Improve respiratory fitness
- Improve blood circulation
- Reduce risk of heart health problems
- Improve bone health and prevent osteoporosis
- Improve your overall mood and wellbeing
- Improve body composition (increase muscle, reduce unhealthy fat)
- Boost the immune system
- Improve chronic shoulder pain with strengthening and stretching
- Reduce fatigue
Refer to the “What are the benefits of exercise after SCI?” section above for more information.
Risks and considerations
While physical activity is essential to maintaining health as you age, the impacts of aging on your body may also increase your risk for injury. These risks should be considered when doing physical activity, especially because problems like pain, fractures, pulled muscles, and strains can hinder participation.
Be aware of:
- Pain that may be an indication of injury.
- Increased risk of fractures due to bone loss (people with SCI are at high risk for osteoporosis).
- Joint degeneration and injury in the shoulders and wrist (people with SCI develop overuse injury with age and have more arthritis and breakdown in the joints).
- Skin breakdown and pressure injury from motions that cause friction during physical activity (skin becomes more thin and less elastic with age and heals more slowly from injury).
How to know when to stop
Many people with SCI live with a baseline level of pain. This can make it difficult to determine whether discomfort and pain while doing physical activity is acceptable or harmful. Expert advice includes starting small and taking note of any discomfort/pain before, during, and after physical activity.
- If physical activity is not causing additional discomfort or pain that persists afterwards, you can maintain or make a small increase to the intensity and/or amount of physical activity.
- If physical activity is causing additional pain that persists afterwards, consider changing the type, or reducing the intensity and/or amount of physical activity.
Adaptations
You may need to adjust your physical activity routines and methods as you age to keep it safe and accessible. Consult your physiotherapist for advice on how to safely do physical activity based on your unique abilities and barriers.
Some possible adaptations:
- Changing the type of physical activity you do
- Slower-paced sports
- Less weight-bearing activities to accommodate injuries or arthritis
- Hobbies that get you moving
- People often get tired more quickly as they age. Start with shorter periods of less intense activity and increase gradually in small increments
- Opportunities to do PA at home (online classes, walking the dog, gardening, etc.)
- Opportunities in the community
- Check with local organizations for online and in-person PA programs
- Equipment and technology to facilitate PA
- Lift or transfer technology to get onto workout equipment
- Work with a trainer/coach who is knowledgeable about SCI
Can medication make you tired?
Some medications used to treat pain or spasticity may cause fatigue, reducing your motivation to be physically active. If you are concerned about the effects of your medication on energy levels, consult with your healthcare provider to see if there are opportunities to optimize your regimen.
Participating in physical activity after SCI can be intimidating, but it is beneficial. Being physically active can help improve your well-being and help reduce the impact of secondary complications after SCI. There are many ways to stay active after an injury, and many ways to adapt existing sports and equipment to help you get exercise. Although exercise is healthy, there are precautions to keep in mind when exercising. Overall, it is recommended that individuals with SCI stay active to promote a healthy lifestyle.
For a list of included studies, please see the Reference List. For a review of how we assess evidence at SCIRE Community and advice on making decisions, please see SCIRE Community Evidence.
Parts of this page has been adapted from SCIRE Professional “Physical Activity” Module:
Wolfe DL, McIntyre A, Ravenek K, Martin Ginis KA, Latimer AE, Eng JJ, Hicks AL, Hsieh JTC (2013). Physical Activity and SCI. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Mehta S, Sakakibara BM, editors. Spinal Cord Injury Rehabilitation Evidence. Version 4.0.
Available from: https://scireproject.com/evidence/physical-activity/
Evidence for “What are the benefits of exercise after SCI?” is based on:
Alexeeva, N., Sames, C., Jacobs, P. L., Hobday, L., DiStasio M. M., Mitchell S.A., & Calancie B. (2011). Comparsion of training methods to improve walking in persons with chronic spinal cord injury: a randomized clinical trial. The Journal of Spinal Cord Medicine, 34, 362—379.Ref 2
Andersen, J. L., Mohr, T., Biering-Sorensen, F., Galbo, H., & Kjaer, M. (1996). Myosin heavy chain isoform transformation in single fibres from m. vastus lateralis in spinal cord injured individuals: effects of long-term functional electrical stimulation (FES). Pflugers Archiv – European Journal of Physiology, 431, 513-518.
Cameron T, Broton JG, Needham-Shropshire B, Klose KJ. An upper body exercise system incorporating resistive exercise and neuromuscular electrical stimulation (NMS). J Spinal Cord Med 1998;21(1):1-6.
Chen Y, Henson S, Jackson AB, Richards JS. Obesity intervention in persons with spnal cord injury. Spinal Cord 2006;44:82-91
Chilibeck PD, Jeon J, Weiss C, Bell G, Burnham R. Histochemical changes in muscle of individuals with spinal cord injury following functional electrical stimulated exercise training. Spinal Cord 1999;37(4):264-268.
Crameri RM, Weston A, Climstein M, Davis GM, Sutton JR. Effects of electrical stimulation- induced leg training on skeletal muscle adaptability in spinal cord injury. Scand J Med Sci Sports 2002;12(5):316-322.
Crameri RM, Cooper P, Sinclair PJ, Bryant G, Weston A. Effect of load during electrical stimulation training in spinal cord injury. Muscle Nerve 2004;29(1):104-111.
de Carvalho DC, Cliquet A, Jr. Energy expenditure during rest and treadmill gait training in quadriplegic subjects. Spinal Cord 2005;43(11):658-663.
De Groot PC, Hjeltnes N, Heijboer AC, Stal W, Birkeland K. Effect of training intensity on physical capacity, lipid profile and insulin sensitivity in early rehabilitation of spinal cord injured individuals. Spinal Cord 2003;41(12):673-679.
Ditor DS, Macdonald MJ, Kamath MV, Bugaresti J, Adams M, McCartney N et al. The effects of body-weight supported treadmill training on cardiovascular regulation in individuals with motor-complete SCI. Spinal Cord 2005;43(11):664-673.
Fukuoka Y, Nakanishi R, Ueoka H, Kitano A, Takeshita K, Itoh M. Effects of wheelchair training on VO2 kinetics in the participants with spinal-cord injury. Disability & Rehabilitation Assistive Technology 2006;1:167-74.
Glinsky, J., Harvey, L., Korten, M., Drury, C., Chee, S., & Gandevia, S. C. (2008). Short-term progressive resistance exercise may not be effective at increasing wrist strength in people with tetraplegia: a randomised controlled trial. Australian Journal of Physiotherapy, 54, 103- 108.
Grimby G, Broberg C, Krotkiewska I, Krotkiewski M. Muscle fibre composition in patients with traumatic cord lesion. Scand J Rehabil Med 1976;8(1):37-42.
Hetz SP, Latimer AE, Martin Ginis KA. Activities of daily living performed by individuals with SCI: Relationships with physical fitness and leisure time physical activity. Spinal Cord 2008;47(7):550-554.
Hicks AL, Adams MM, Martin GK, Giangregorio L, Latimer A, Phillips SM et al. Long-term body- weight-supported treadmill training and subsequent follow-up in persons with chronic SCI: effects on functional walking ability and measures of subjective well-being. Spinal Cord 2005;43(5):291-298.
Jacobs, P. L. (2009). Effects of resistance and endurance training in persons with paraplegia. Medicine & Science in Sports & Exercise, 41, 992-997.
Jeon JY, Weiss CB, Steadward RD, Ryan E, Burnham RS, Bell G et al. Improved glucose tolerance and insulin sensitivity after electrical stimulation-assisted cycling in people with spinal cord injury. Spinal Cord 2002;40(3):110-117.
Klose KJ, Schmidt DL, Needham BM, Brucker BS, Green BA, Ayyar DR. Rehabilitation therapy for patients with long-term spinal cord injuries. Archives of Physical Medicine & Rehabilitation 1990;71:659-62.
Le Foll-de Moro D, Tordi N, Lonsdorfer E, Lonsdorfer J. Ventilation efficiency and pulmonary function after a wheelchair interval-training program in subjects with recent spinal cord injury. Arch Phys Med Rehabil 2005;86(8):1582-1586.
Martin Ginis KA, Latimer AE, McKechnie K, Ditor DS, Hicks AL, Bugaresti J. Using exercise to enhance subjective well-being among people with spinal cord injury: The mediating influences of stress and pain. REHABIL PSYCHOL 2003;48(3):157-164.
Millar PJ, Rakobowchuk M, Adams MM, Hicks AL, McCartney N, MacDonald MJ. Effects of short-term training on heart rate dynamics in individuals with spinal cord injury. Auton Neurosci 2009; 150: 116-21.
Mohr T, Dela F, Handberg A, Biering-Sorensen F, Galbo H, Kjaer M. Insulin action and long- term electrically induced training in individuals with spinal cord injuries. Med Sci Sports Exerc 2001;33(8):1247-1252.
Mulroy, S. J., Thompson, L., Kemp, B., Hatchett, P. P., Newsam, C. J., Lupold, D. G., et al. (2011). Strengthening and Optimal Movements for Painful Shoulders (STOMPS) in chronic spinal cord injury: a randomized controlled trial. Physical Therapy, 91, 305—324.
Needham-Shropshire BM, Broton JG, Cameron TL, Klose KJ. Improved motor function in tetraplegics following neuromuscular stimulation-assisted arm ergometry. J Spinal Cord Med 1997;20(1):49-55.
Round JM, Barr FM, Moffat B, Jones DA. Fibre areas and histochemical fibre types in the quadriceps muscle of paraplegic subjects. J Neurol Sci 1993;116(2):207-211.
Sabatier, M. J., Stoner, L., Mahoney, E. T., Black, C., Elder, C., Dudley, G. A. et al. (2006). Electrically stimulated resistance training in SCI individuals increases muscle fatigue resistance but not femoral artery size or blood flow. Spinal Cord, 44, 227-233.
Silva AC, Neder JA, Chiurciu MV, Pasqualin DC, da Silva RC, Fernandez AC et al. Effect of aerobic training on ventilatory muscle endurance of spinal cord injured men. Spinal Cord 1998;36(4):240-245.
Sutbeyaz ST, Koseoglu BF, Gokkaya NK. The combined effects of controlled breathing techniques and ventilatory and upper extremity muscle exercise on cardiopulmonary responses in patients with spinal cord injury. Int J Rehabil Res 2005;28(3):273-276.
Stewart BG, Tarnopolsky MA, Hicks AL, McCartney N, Mahoney DJ, Staron RS et al. Treadmill training-induced adaptations in muscle phenotype in persons with incomplete spinal cord injury. Muscle Nerve 2004;30(1):61-68.
Evidence for “What are the exercise guidelines?” is based on:
Martin Ginis, K. A., van der Scheer, J. W., Latimer-Cheung, A. E., Barrow, A., Bourne, C., Carruthers, P., … Goosey-Tolfrey, V. L. (2018). Evidence-based scientific exercise guidelines for adults with spinal cord injury: an update and a new guideline. Spinal Cord, 56(4), 308–321.
SCIRE. (2020, March 6). Exercise after Spinal Cord Injury: How to Begin [Video file]. Retrieved from https://www.youtube.com/watch?v=P0EWCQawRbI&list=PLi2Dc1h0G7-vn6X1ROpMEMXJK6nmzinWu&index=2
Evidence for “How can I adapt exercises?” is based on:
SCIRE. (2020, March 6). Exercise after Spinal Cord Injury: How to Adapt Equipment [Video file]. Retrieved from https://www.youtube.com/watch?v=k7vTlHzYoug&list=PLi2Dc1h0G7-vn6X1ROpMEMXJK6nmzinWu&index=4
Evidence for “What should I be cautious of when exercising?” is based on:
SCIRE. (2020, March 6). Exercise after Spinal Cord Injury: Complications to Avoid [Video file]. Retrieved from: https://www.youtube.com/watch?v=HXVaLdhsBuk&list=PLi2Dc1h0G7-vn6X1ROpMEMXJK6nmzinWu&index=3
Evidence for ” How does aging affect physical activity after SCI?” is based on:
Cerrel Bazo, H. A., Demertzis, E., & Musumeci, A. (2018). The Aging Effects in Spinal Cord Injury Rehabilitation (pp. 379–402). https://doi.org/10.1007/978-3-319-57406-6_39
Cheung, L., Chiang, J., Kaiser, A., Patterson, K. K., & Musselman, K. E. (2023). Exploring the Experiences and Perceptions of Adults With Spinal Cord Injury or Disease Aged 50 Years or Older on Participation in Sports. Topics in Spinal Cord Injury Rehabilitation, 29(4), 37–50. https://doi.org/10.46292/sci23-00028
Galea, M. P. (2012). Spinal cord injury and physical activity: preservation of the body. Spinal Cord, 50(5), 344–351. https://doi.org/10.1038/sc.2011.149
Jiang, S.-D., Dai, L.-Y., & Jiang, L.-S. (2006). Osteoporosis after spinal cord injury. Osteoporosis International, 17(2), 180–192. https://doi.org/10.1007/s00198-005-2028-8
Krause, J. S., Vines, C. L., Farley, T. L., Sniezek, J., & Coker, J. (2001). An exploratory study of pressure ulcers after spinal cord injury: Relationship to protective behaviors and risk factors. Archives of Physical Medicine and Rehabilitation, 82(1), 107–113. https://doi.org/10.1053/apmr.2001.18050
Lee, A. K. Y., Miller, W. C., Townson, A. F., & Anton, H. A. (2010). Medication use is associated with fatigue in a sample of community-living individuals who have a spinal cord injury: a chart review. Spinal Cord, 48(5), 429–433. https://doi.org/10.1038/sc.2009.145
Lundström, U., Wahman, K., Seiger, Å., Gray, D. B., Isaksson, G., & Lilja, M. (2017). Participation in activities and secondary health complications among persons aging with traumatic spinal cord injury. Spinal Cord, 55(4), 367–372. https://doi.org/10.1038/sc.2016.153
Mulroy, S. J., Thompson, L., Kemp, B., Hatchett, P. P., Newsam, C. J., Lupold, D. G., Haubert, L. L., Eberly, V., Ge, T.-T., Azen, S. P., Winstein, C. J., & Gordon, J. (2011). Strengthening and Optimal Movements for Painful Shoulders (STOMPS) in Chronic Spinal Cord Injury: A Randomized Controlled Trial. Physical Therapy, 91(3), 305–324. https://doi.org/10.2522/ptj.20100182
Paterson, D. H., Jones, G. R., & Rice, C. L. (2007). Ageing and physical activity: evidence to develop exercise recommendations for older adults. Applied Physiology, Nutrition, and Metabolism, 32(S2E), S69–S108. https://doi.org/10.1139/H07-111
Tawashy, A. E., Eng, J. J., Lin, K. H., Tang, P. F., & Hung, C. (2009). Physical activity is related to lower levels of pain, fatigue and depression in individuals with spinal-cord injury: a correlational study. Spinal Cord, 47(4), 301–306. https://doi.org/10.1038/sc.2008.120
Tomasone, J. R., Wesch, N. N., Ginis, K. A. M., & Noreau, L. (2013). Spinal Cord Injury, Physical Activity, and Quality of Life: A Systematic Review. Kinesiology Review, 2(2), 113–129. https://doi.org/10.1123/krj.2.2.113
Waters, R., & Sie, I. (2001). Upper Extremity Changes with SCI Contrasted to Common Aging in the Musculoskeletal System. Topics in Spinal Cord Injury Rehabilitation, 6(3), 61–68. https://doi.org/10.1310/7TD2-Q5CX-5WH1-FDXH
Image credits
- Muscle ©Servier Medical Art, CC BY 3.0
- Woman on FES ©SCIRE, CC BY-NC 4.0
- Transferring ©SCIRE, CC BY-NC 4.0
- Wheelchair woman disability ©codipunnett, Pixabay License
- Modified from: Femur, Lungs, Heart ©Servier Medical Art, CC BY 3.0, and Lightning ©FLPLF, CC BY 3.0
- Arm cycling ©SCIRE, CC BY-NC 4.0
- Sledge Hockey: Italy/Sweden ©Mariska Richters, CC BY-NC-SA 2.0
- Bodyweight Support Treadmill ©SCIRE, CC BY-NC 4.0
- RPE Scale ©SCIRE, CC BY-NC 4.0
- RPE thumbnail ©SCIRE, CC BY-NC 4.0
- Adapted Exercise Thumbnail ©SCIRE, CC BY-NC 4.0
- Adaptive grip aids ©SCIRE, CC BY-NC 4.0
- Abdominal Binder ©SCIRE, CC BY-NC 4.0
- Dizzy ©Berkah Icorn, CC BY 3.0
- Exercise Video Series ©SCIRE, CC BY-NC 4.0
- High blood ©Eucalyp, CC BY 3.0
- Hot thermometer ©Abby, DE, CC BY 3.0
- Modified from: Man Resting on Long Chair ©Gan Khoon Lay, CC BY 3.0
- Shoulder injury ©ProSymbols, US, CC BY 3.0
- Aging Activity Thumbnail ©SCIRE, CC BY-NC 4.0





 Conditions impacting the heart and blood vessels, by improving the strength of the heart and balancing out the sympathetic (fight or flight; stimulation) and parasympathetic (relax and slowing) nervous systems,
Conditions impacting the heart and blood vessels, by improving the strength of the heart and balancing out the sympathetic (fight or flight; stimulation) and parasympathetic (relax and slowing) nervous systems,