Author: Sharon Jang | Reviewer: Cathy Nevens | Published: 7 September 2019 | Updated: ~
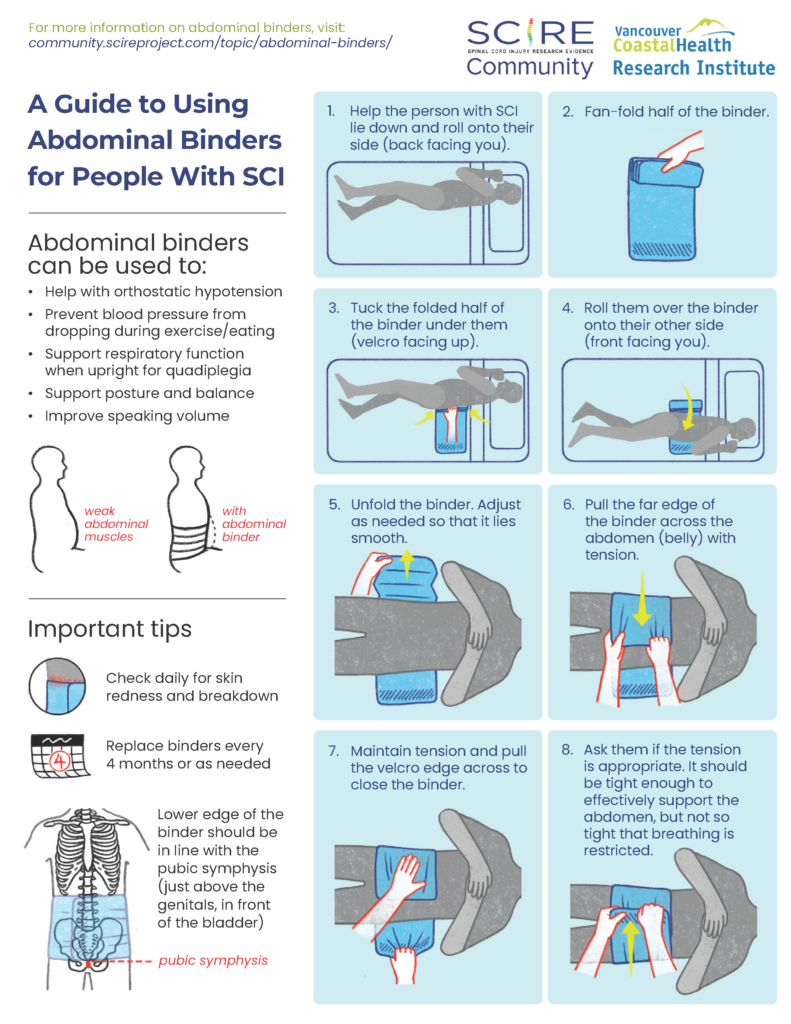
Abdominal binders are simple pieces of equipment that are used to support the abdomen. This page outlines what abdominal binders are and how they are used after spinal cord injury (SCI).
Key Points
- Abdominal binders are devices which apply pressure to the abdomen to help improve breathing and circulation in upright postures.
- These may be elastic or non-elastic devices that wrap around the lower torso to apply pressure and mimic the function of the abdominal muscles.
- Abdominal binders are considered safe with a minimal number of risks when used appropriately.
- Research suggests that abdominal binders can help to reduce changes in blood pressure (orthostatic hypotension) when moving from a lying to standing position and may help to improve breathing after SCI.

Abdominal binders wrap around to support the abdomen when the abdominal muscles are weak or paralyzed. They are normally worn under the shirt.1
An abdominal binder is an elastic piece of material that is placed normally placed around the lower torso to apply pressure to the abdomen. Abdominal binders should fit snugly around the torso and be tight enough to provide support, but should not be uncomfortable. Abdominal binders are typically worn under the shirt and are mainly used to improve circulation and breathing when in an upright position. They are also sometimes used to help maintain balance and stability of the trunk and to support sagging of the abdomen (sometimes called “quad belly”) that can happen when the abdominal muscles are weak.
There are two main types of abdominal binders: elastic and non-elastic binders. Each of these types will have a number of different models or designs available that may be used. Talk to your health providers about what type are most appropriate for you.
Elastic abdominal binders
The most common type of abdominal binder used by people with SCI is made from a stretchy elastic fabric that is placed around the abdomen and closed with Velcro. The material mimics the nature of the abdominal muscles by providing some pressure but also allowing the abdomen to expand and recoil while breathing. Some elastic abdominal binders have additional supports built into them that may be used to assist with balance and stability.
Non-elastic abdominal binders
Non-elastic abdominal binders include pieces of equipment such as a corset, girdle, straps or mechanical device to support the abdomen. These are made from a non-stretchy material that provides greater support. Non-elastic abdominal binders are not used as often after SCI because they have greater potential to injure the skin and may also restrict the abdomen while breathing, which may contribute to an abnormal breathing pattern.
Breathing and cough function
 People with cervical and thoracic SCI may experience breathing problems because of a loss of nerve control to the diaphragm and other breathing muscles (including the abdominal muscles). This causes the diaphragm to sit too low in the abdomen so it cannot work optimally.
People with cervical and thoracic SCI may experience breathing problems because of a loss of nerve control to the diaphragm and other breathing muscles (including the abdominal muscles). This causes the diaphragm to sit too low in the abdomen so it cannot work optimally.
Abdominal binders are thought to mimic some of the function of the abdominal muscles to help support breathing. The binder compresses the abdomen, which increases pressure and may help to raise the diaphragm into a better position for breathing.
There is evidence that abdominal binding in people with tetraplegia can improve respiratory function. Studies have shown that the use of abdominal binders can improve an individual’s ability to inhale and exhale. Overtime, the use of an abdominal binder can strengthen the muscles that are used to inhale. The design of the abdominal binder may also influence its effectiveness. For example, one (weak evidence) study found that a custom girdle may cause individuals to perceive breathing as easier.
More research is required to find out how using an abdominal binder strengthens the diaphragm and whether this leads to easier breathing. Abdominal binding for people with SCI should be introduced gradually due to potential adverse effects on one’s ability to breathe.
Refer to our article on Respiratory Changes After SCI for more information!
Blood pressure and circulation
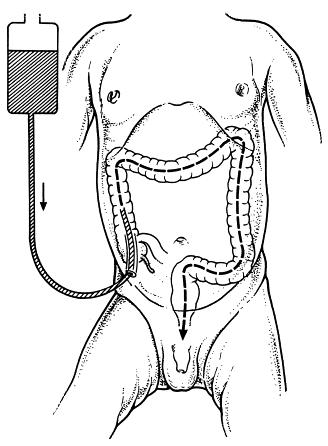
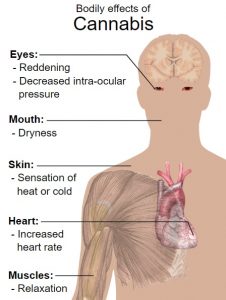
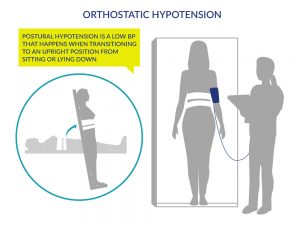
 Many people with SCI experience a drop in blood pressure when moving from a lying or sitting position to an upright position. This is known as orthostatic hypotension. This condition happens because a loss of nerve function can impair the body’s ability to tighten (constrict) the blood vessels and change heart rate, which is an important part of maintaining blood pressure in different positions.
Many people with SCI experience a drop in blood pressure when moving from a lying or sitting position to an upright position. This is known as orthostatic hypotension. This condition happens because a loss of nerve function can impair the body’s ability to tighten (constrict) the blood vessels and change heart rate, which is an important part of maintaining blood pressure in different positions.
Because abdominal binders wrap around and compress the abdomen, they may help to increase pressure in the abdominal area. This may help to prevent blood pooling in the blood vessels in the abdomen when upright, which may help maintain blood pressure and allow better circulation.
There is conflicting evidence based on limited research that abdominal binders have any effect on cardiovascular responses in people with SCI. One study found that abdominal binders do not have any effect on average blood pressure or other cardiovascular responses. However, other studies suggest that abdominal binders in combination with leg stockings may have an effect on cardiovascular responses during lower intensity arm exercise.
Refer to our article on Orthostatic Hypotension for more information!
Speech
 There is some weak evidence for the use of an abdominal binder to improve speech. One study found that participants with difficulty speaking due to cervical level injuries were able to produce more natural sounding speech, were able to speak louder, and improved overall voice quality with the use of an abdominal binder. Meanwhile, another study has shown that using an abdominal binder can extend the length that sound is produced for.
There is some weak evidence for the use of an abdominal binder to improve speech. One study found that participants with difficulty speaking due to cervical level injuries were able to produce more natural sounding speech, were able to speak louder, and improved overall voice quality with the use of an abdominal binder. Meanwhile, another study has shown that using an abdominal binder can extend the length that sound is produced for.
Balance, stability, and appearance
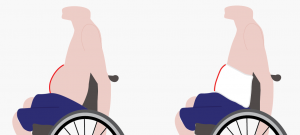
Abdominal binders may be used to support the abdomen to reduce the appearance of “quad belly”.5
Some individuals use an abdominal binder as they perceive it helps to support their trunk or assist with sitting balance. In addition, some individuals find that it helps them balance when performing two-handed exercises. However, no research has been done to support this. Some individuals may use a binder to reduce the appearance of the abdomen sagging forward, sometimes called “quad belly”.
Abdominal binders are considered safe for most people. In all cases, the skin under the binder should be regularly checked for pressure sores. However, there are situations in which abdominal binders may not be appropriate and carry possible risks. Please consult a health provider for detailed safety information.
Abdominal binders should be used with caution in the following situations:
- Do not use directly over areas prone to pressure injuries or over current injuries, wounds, or sores
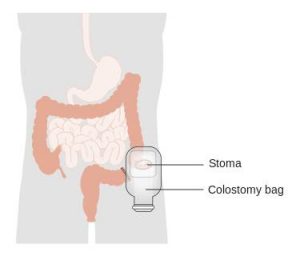
- Caution is advised if a person has a stoma (colostomy or urostomy bag) on the front of their abdomen. There is the possibility of the binder causing irritation or interference to the stoma site. A customized binder may be required to ensure no irritation to the area.
Risks of using abdominal binders may include:
- Pressure injuries, if the equipment is too tight and creates too much pressure or cuts into the skin.
- If the abdominal binder is tightened too much, it can get in the way of the abdomen and lower ribs expanding, which may make breathing difficult.
- Also, an overly tight abdominal binder could cause an increase in spasticity or trigger autonomic dysreflexia in some people.
Refer to our articles on Pressure Injuries, Spasticity, and Autonomic Dysreflexia for more information!
Abdominal binders are a physical treatment that supports the abdomen when the abdominal muscles are weak or paralyzed.
The support from the binder can improve cardiovascular and respiratory responses including blood pressure and breathing.
Some individuals may use a binder to help with balance and stabilizing the trunk but there is no research evidence to support this.
Some individuals may use a binder to reduce the appearance of abdominal muscles that bulge out following paralysis.
For a review of how we assess evidence at SCIRE Community and advice on making decisions, please see SCIRE Community Evidence.
This page has been adapted from SCIRE Professional “Respiratory Management” and “Orthostatic Hypotension” Modules:
Sheel AW, Reid WD, Townson AF (2018). Respiratory Management Following Spinal Cord Injury. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, Sproule S, Querée M, McIntyre A, editors. Spinal Cord Injury Rehabilitation Evidence. Version 6.0. Vancouver: p. 1-72.
Available from: scireproject.com/evidence/respiratory-management/
Krassioukov A, Wecht JM, Teasell RW, Eng JJ (2014). Orthostatic Hypotension Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, McIntyre A, editors. Spinal Cord Injury Rehabilitation Evidence. Version 5.0. Vancouver: p 1- 26.
Available from: scireproject.com/evidence/orthostatic-hypotension/non-pharmacological-management-of-oh/
Evidence for “Are abdominal binders safe to use?”
Cornwell, P., Ward, E., Lim, Y., & Wadsworth, B. (2014). Impact of an Abdominal Binder on Speech Outcomes in People With Tetraplegic Spinal Cord Injury: Perceptual and Acoustic Measures. Topics in Spinal Cord Injury Rehabilitation, 20(1), 48–57. https://doi.org/10.1310/sci2001-48
Wadsworth, B. M., Haines, T. P., Cornwell, P. L., Rodwell, L. T., & Paratz, J. D. (2012). Abdominal Binder Improves Lung Volumes and Voice in People With Tetraplegic Spinal Cord Injury. YAPMR, 93(12), 2189–2197. https://doi.org/10.1016/j.apmr.2012.06.010
Image credits:
- Image by SCIRE
- Lungs ©karina, CC BY 3.0 US
- Blood Pressure ©Ricardo Moreira, CC BY 3.0 US
- speak ©Gregor Cresnar, CC BY 3.0 US
- Image by SCIRE













 Dutch
Dutch English
English German
German Indonesian
Indonesian Italian
Italian Korean
Korean Persian
Persian Spanish
Spanish Swedish
Swedish
 A group led by Dr. Kathleen Martin Ginis at the University of British Columbia and Dr. Victoria Goosey-Tolfrey at Loughborough University, UK developed international guidelines on exercise after SCI. The process of developing these guidelines involved a systematic review of relevant literature, consensus meetings, stakeholder feedback, and a formal audit of the process.
A group led by Dr. Kathleen Martin Ginis at the University of British Columbia and Dr. Victoria Goosey-Tolfrey at Loughborough University, UK developed international guidelines on exercise after SCI. The process of developing these guidelines involved a systematic review of relevant literature, consensus meetings, stakeholder feedback, and a formal audit of the process.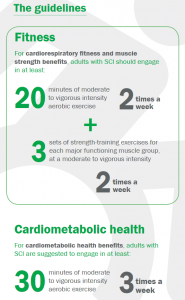

 If you are not already exercising, it is okay to start with smaller amounts of exercise and gradually increase duration, frequency, and intensity, as a progression toward meeting the guidelines. Doing exercise below the recommended levels may or may not bring small changes in fitness or cardiometabolic health.
If you are not already exercising, it is okay to start with smaller amounts of exercise and gradually increase duration, frequency, and intensity, as a progression toward meeting the guidelines. Doing exercise below the recommended levels may or may not bring small changes in fitness or cardiometabolic health. Exceeding these exercise guidelines would be expected to yield additional cardiorespiratory fitness and muscle strength and cardiometabolic health benefits. However, there are insufficient data to comment on the risks associated with a person with SCI exceeding these guidelines.
Exceeding these exercise guidelines would be expected to yield additional cardiorespiratory fitness and muscle strength and cardiometabolic health benefits. However, there are insufficient data to comment on the risks associated with a person with SCI exceeding these guidelines.








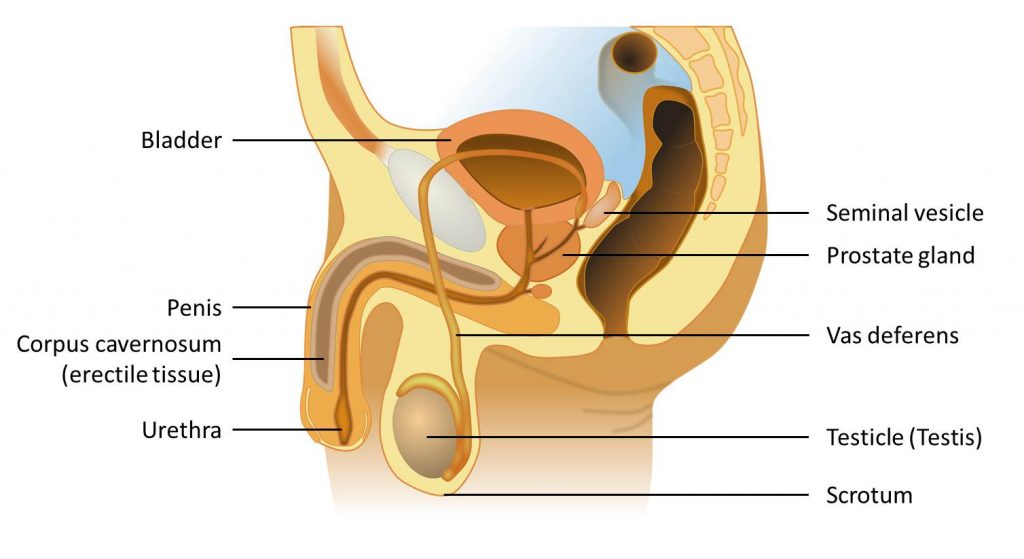
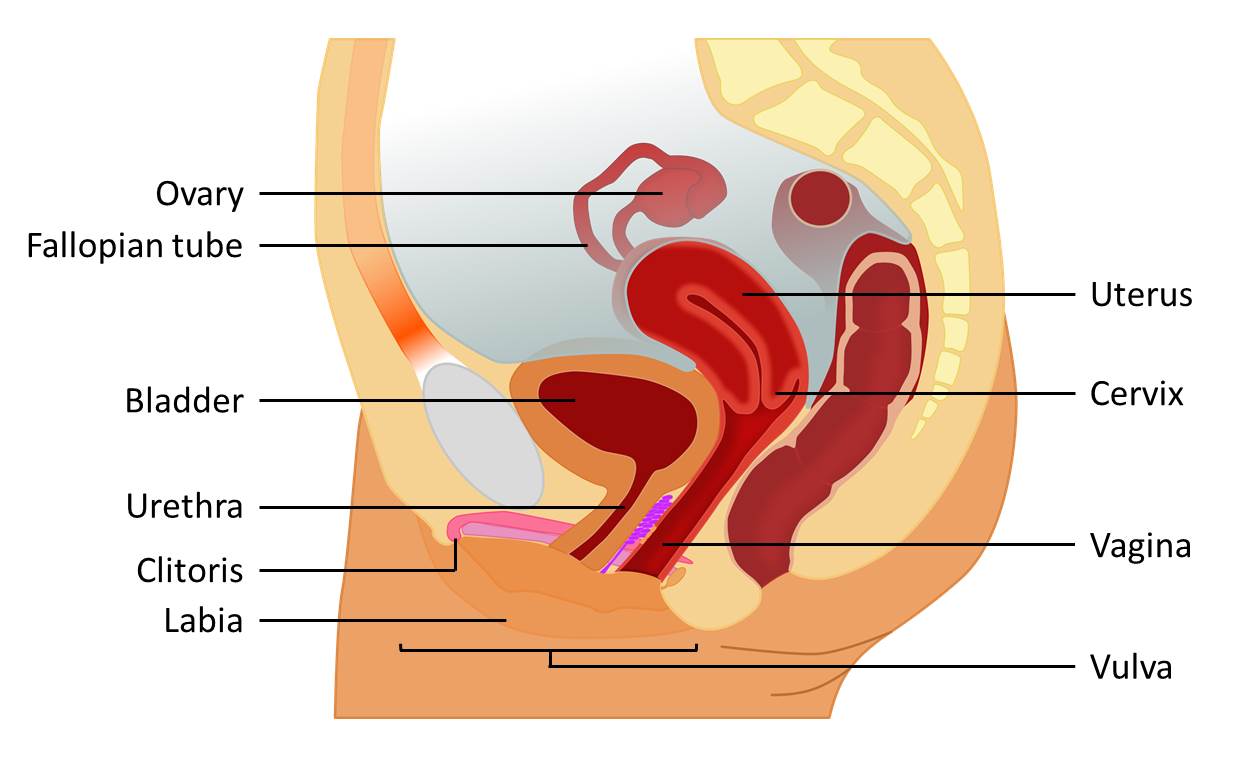




 Assuming positions for sex may be more challenging after an SCI because of changes in movement control and flexibility. It may also be hard to get into certain positions because of reduced flexibility caused by spasticity and joint contractures. It may help to:
Assuming positions for sex may be more challenging after an SCI because of changes in movement control and flexibility. It may also be hard to get into certain positions because of reduced flexibility caused by spasticity and joint contractures. It may help to:














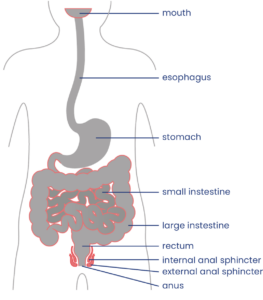




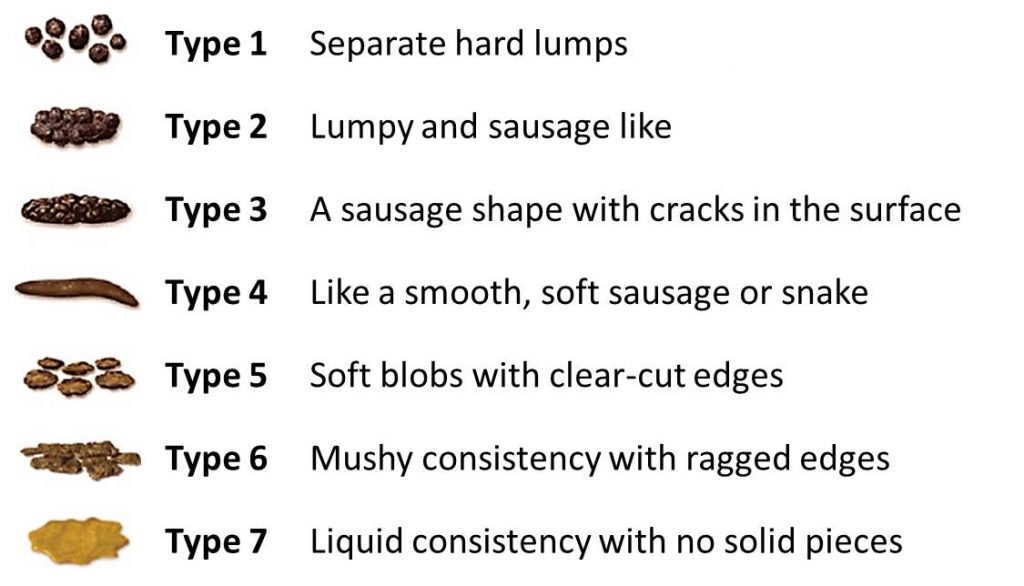
 Your bowel function and symptoms may change over time. Most health providers recommend people with SCI to have a check-up once every two to three years or if there are changes to bowel function to keep track of changes to your bowel function and care.
Your bowel function and symptoms may change over time. Most health providers recommend people with SCI to have a check-up once every two to three years or if there are changes to bowel function to keep track of changes to your bowel function and care. every day or every other day to empty the bowel. There is a wide range of different components that may make up a bowel routine, such as hands-on emptying techniques, diet and lifestyle changes, and the use of suppositories, mini-enemas and medications.
every day or every other day to empty the bowel. There is a wide range of different components that may make up a bowel routine, such as hands-on emptying techniques, diet and lifestyle changes, and the use of suppositories, mini-enemas and medications.
 People with injuries at T6 and above may trigger autonomic dysreflexia when performing digital stimulation and other bowel techniques. Keep an eye out for signs including sweating, headache, heart rate changes, goose bumps and increasing muscle spasms, and stop any techniques right away. Autonomic dysreflexia can also be triggered by bowel problems such as constipation or hemorrhoids.
People with injuries at T6 and above may trigger autonomic dysreflexia when performing digital stimulation and other bowel techniques. Keep an eye out for signs including sweating, headache, heart rate changes, goose bumps and increasing muscle spasms, and stop any techniques right away. Autonomic dysreflexia can also be triggered by bowel problems such as constipation or hemorrhoids.


 The gastrocolic reflex is when food or drink in the stomach triggers movement in the bowel. Some people eat food or drink warm fluids at least 30 minutes before their bowel routine to try to take advantage of this reflex, which is thought to be strongest in the morning. Many people use this technique as part of their bowel care; however the evidence is conflicting about whether the gastrocolic reflex is effective after SCI.
The gastrocolic reflex is when food or drink in the stomach triggers movement in the bowel. Some people eat food or drink warm fluids at least 30 minutes before their bowel routine to try to take advantage of this reflex, which is thought to be strongest in the morning. Many people use this technique as part of their bowel care; however the evidence is conflicting about whether the gastrocolic reflex is effective after SCI.